AT A GLANCE
• In developing a comprehensive keratoconus treatment plan, corneal surgeons and contact lens specialists must work together to find the most effective and secure modality of correction.
•Due to the recent development of a wide array of lenses, it has become standard of care to conduct a specialty lens trial before referring a keratoconus patient for surgery.
• Many patients will find that contact lens correction provides them with unequaled quality of vision,excellent lens tolerance, and long wearing times.
Rigid corneal lenses remain the first choice of treatment for the visual rehabilitation of patients with irregular corneas; however, for too many years, patients who have worn them suffered in silence because of discomfort and limited wearing times. Typically, novice contact lens wearers are happy about the crisp visual acuity they achieve with these lenses, and, unless questioned, they will not spontaneously disclose any discomfort issues.
Patients with keratoconus no longer need to tolerate contact lens discomfort in order to obtain good vision. In recent years, surgeons have gained access to a wide array of specialty lens types that can offer both excellent visual acuity and comfort, while simultaneously respecting the physiology of the cornea.
Fundamental 1. RGP LENSES ARE THE GOLD STANDARD FOR IRREGULAR ASTIGMATISM
Rigid gas-permeable (RGP) lenses are still the lenses of choice for the correction of irregular astigmatism because they mask the underlying irregularity of the cornea and create a perfectly regular anterior refractive surface for
the eye.
RGP lenses can correct for all types and stages of keratoconus. They also offer maximal correction of visual acuity, the ability to fine-tune any refraction, adjustable power and lens parameters if the cornea changes, complete reversibility of contact lens correction, and a good safety profile. The limiting factor for contact lens correction is corneal scarring, with opacification at the corneal apex so that good visual acuity is no longer obtainable; in these cases, corneal transplant surgery is indicated.
Keratoconus presents an unusual, complex situation for contact lens fitters, in that the front surface of the cornea is extremely steep at the apex of the cone but flattens toward the midperiphery, or the base of the cone. Additionally, the lower cones can be quite asymmetric, especially along the vertical meridian.
.png)
Figure 1. The three parts of a scleral lens:optic, transitional zone, and haptic zone. The red arrow indicates the sagittal height of the lens.
The trial-and-error method of fitting cannot be abandoned completely, but the systematic use of corneal topography and fitting guides has reduced chair time significantly. Major advances have been made in offering adapted lens designs that better approximate the altered topography of the cornea in keratoconus. Different back surface designs are available for central nipple cones, more inferiorly located cones, and very low cones with central flattening.
A large choice of lens parameters allows lenses to be adapted to individual corneas so that each lens is, in fact, custom-made. Modern RGP lenses have high oxygen transmissibility and can therefore be made in larger diameters, allowing lid attachment fitting and avoiding irritation of the upper lid during blinking. The fitting strategy should aim to distribute the weight of the lens over the corneal surface and avoid pressure on the apex of the cone so as not to induce scarring.
Most patients with keratoconus are well habituated to their corneal RGP lenses and wear them mostly to great satisfaction. They appreciate the ease of handling and care, as well as the fact that RGP lenses are a relatively cheap option among specialty lenses. Too many patients, however, do not tolerate these lenses well, either because of allergy and dry eye or because of subjective discomfort. In some cases, it is not possible to find a lens that centers well and avoids apical bearing and staining of the epithelium. For these eyes, an alternative solution is necessary.
Fundamental 2.SPECIALTY SOFT LENSES CAN WORK WONDERS IN MILD KERATOCONUS
Soft contact lenses designed for keratoconus are generally thicker centrally than standard soft lenses, ranging from 0.3 to 0.6 mm compared with 0.1 mm in a standard lens. This increased central thickness helps prevent the lens from conforming to the irregular shape of the cornea, so that mild to moderate irregular astigmatism can be masked. Increasing lens thickness in hydrogel lenses, however, decreases oxygen permeability, raising concerns for hypoxia-related disturbances. Lathe-cut lenses in more oxygen-permeable silicone hydrogel materials are now available in an almost unlimited range of parameters. These lenses are available in the high spherical and toric powers commonly required for keratoconus.
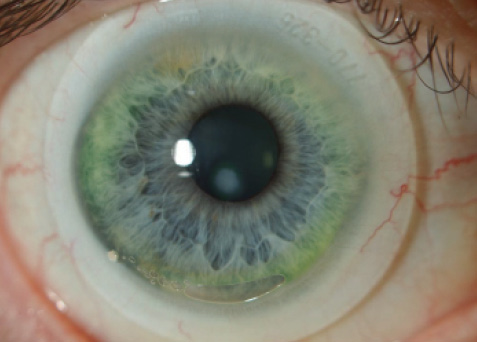
Figure 2. A scleral lens fitted on a keratoconic eye with a paracentral scar.
.jpg)
Figure 3. OCT showing the clearance of a scleral lens over a keratoconic cornea with a proud nebula.
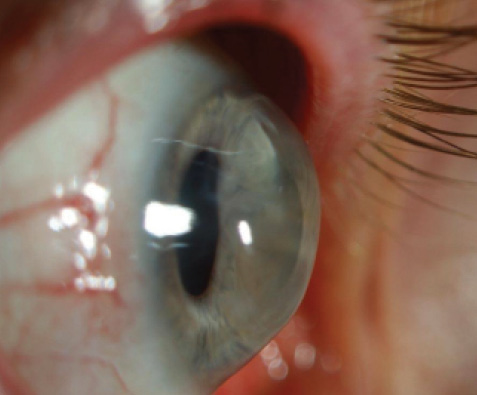
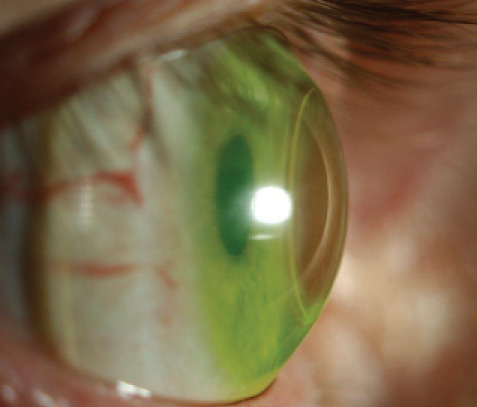
Figure 4. A scleral lens fitted on a penetrating graft for keratoconus with high postkeratoplasty astigmatism.
Although improvements in the stabilization of toric designs have been made, the best candidates for this type of lens are the high ametropes or myopes with relatively low cylindric corrections. These types of keratoconic eyes are also the best suited for phakic IOLs.
Fundamental 3. PIGGYBACK AND HYBRID LENSES: THE BEST OF BOTH WORLDS?
The piggyback concept of fitting an RGP lens over a soft lens can be applied not only in patients with RGP lens intolerance but also as a problem-solver for lens decentration and dryness issues. The soft lens provides comfort by avoiding contact between the RGP lens and the cornea, while the rigid lens provides better acuity than the soft lens ever could. Patients, however, are often not attracted to the idea of using and caring for two lenses in one eye. Also, eyelid sensitivity is not eliminated. However, piggyback fitting is easy to try out using a thin soft lens if the patient’s keratoconus is not too advanced.
Hybrid lenses combine the best of both worlds by integrating an RGP core in a soft skirt so that the eyelids do not move over the rigid lens edge, further increasing comfort. Patient reports of comfort are immediately positive, and the lenses are by default well centered and stable on the eye. In the medium term, however, problems with lens tightening and intolerance were reported with initial hybrid designs.
Newer-generation hybrid lenses offer materials with highly increased oxygen permeability and a wider array of geometries, ideally providing apical clearance. At the moment, this lens type seems to be best suited for more central, less advanced cones. It is worth mentioning that hybrid lenses can provide patients with regular astigmatism with a crisp quality of vision that cannot always be obtained with soft toric IOLs.
Fundamental 4. SCLERAL LENSES TICK ALL THE BOXES
Scleral lenses have been around for more than a century; however, they were long relegated to the sidelines of contactology because of their large diameters (20-25 mm), problems with corneal hypoxia related to the use of non–gas-permeable materials, and the intricacies of handling them. Since around 2010, industry and optometry have developed a lively interest in this type of lens, and the reactions of wearers and fitters to new designs have been extremely positive.
With the advent of these modern scleral lenses, any type of irregular cornea can now be fitted with a well-centered, stable lens that provides maximal visual acuity and comfort. A scleral lens is a large-diameter lens that vaults the cornea and has its resting zone beyond the limbus, on the sclera. The geometry of a typical lens can be broken down into three zones: (1) the optic zone, (2) the haptic zone landing on the sclera, and (3) the transitional zone setting the sagittal height of the lens (Figure 1). Ideally, this type of lens does not make contact with the cornea; it technically is no longer a contact lens.
The smaller diameters of modern scleral lenses (15-20 mm) are less frightening for patients. Once the lens is on the eye, even supposedly contact lens–intolerant patients are convinced that comfortable contact lens correction is now possible for them. Worldwide interest in these lenses is rising, as they allow effective and stable correction of all types of irregularity of the corneal surface. They rest on the relatively insensitive sclera and vault the cornea, thereby facilitating fitting on highly irregular corneas (Figure 2). Due to the large diameters of these lenses, the eyelids do not touch the lens edges, which greatly enhances comfort. Some specialists suggest that scleral lenses should become the first choice for correction of irregular corneas, not only for patients with keratoconus but also for patients after keratoplasty or refractive surgery.
Anterior segment OCT (Figure 3) has helped us develop a better appreciation of the shape of the cornea and sclera, which has led to improvements in scleral lens curve design. In the clinic, OCT can also be used to document the settling behavior of scleral lenses on the eye during lens wear to ensure corneal and limbal clearance throughout the day.
Fundamental 5. A NEW DEFINITION OF CONTACT LENS INTOLERANCE AND A TRIAL FITTING ARE RECOMMENDED
Contact lenses, refractive surgery, and corneal transplant surgery are complementary approaches in the treatment of irregular astigmatism. Refractive surgery is indicated in patients who are contact lens intolerant, for whatever reason. If neither contact lenses nor refractive surgery can provide the keratoconus patient with a satisfactory visual acuity—generally better than 20/40 is considered acceptable—then transplant surgery is required.
Recent developments in specialty lenses have broadened the opportunities for contact lens correction in these cases. Scleral lenses in particular are so successful that they might replace corneal lenses as a first-choice treatment. As a consequence, we need to redefine contact lens intolerance and do a trial fitting with the new specialty lenses before deciding to offer surgery.
Being dependent on lenses for daily life has, however, been established as a negative factor in quality of life for keratoconus patients. In selected patients, refractive surgery can offer the prospect of improving UCVA and BCVA more or less successfully. It is up to the patient and the treating ophthalmologist to weigh all of the options available and establish a treatment plan tailored to the needs and expectations of the individual.
The same reasoning is true for patients with stage 4 keratoconus—the advanced cones with pronounced thinning and scarring—for whom the literature will advise transplant surgery. DeLoss et al1 conducted a study comparing scleral lenses and keratoplasty in the treatment of ectasia. The investigators found that visual outcomes were better and more rapidly achieved with scleral lenses than with keratoplasty. The percentage of eyes achieving 20/25 was 80% for scleral lenses and about 35% for keratoplasty.
A scleral lens trial should therefore be considered in patients with advanced corneal ectasia before proceeding to keratoplasty, especially if the ectasia is deemed stable. Of note, in the aforementioned study, 27% of postkeratoplasty eyes needed lens correction. Patients should be informed beforehand that contact lens correction may still be necessary after transplant surgery (Figure 4).
CONCLUSION
In developing a comprehensive keratoconus treatment plan, corneal surgeons and contact lens specialists must work together to find the most effective and secure modality of correction. Typically, refractive surgery—involving intrastromal corneal rings, implants, etc.—is indicated if the patient is contact lens intolerant.
Due to the recent development of a wide array of lenses, it has become standard of care to conduct a specialty lens trial before referring a patient for surgery. Many patients will find that contact lens correction provides them with unequaled quality of vision, excellent lens tolerance, and long wearing times. This may be bad news for refractive surgery volume; however, including specialty contact lenses in one’s clinic gives a boost to a practice’s reputation as a one-stop keratoconus center.
1. DeLoss KS, Fatteh NH, Hood CT. Prosthetic replacement of the Ocular Surface Ecosystem (PROSE) scleral device compared to keratoplasty for the treatment of corneal ectasia. Am J Ophthalmol. 2014;158(5):974-982.
Further reading:
Eiden SB, Chang C, Davis R, Brafman S. Contact lens options for managing keratoconus and keractectasias. Contact Lens Spectrum. 2013;28;38-44.
Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011;30(12):1510-1516.
Koppen C. Corneal cross-linking and keratoconus: the change in treatment paradigm of keratoconus. Bull Soc Belge Ophtalmol. 2012;321:5, 9-23, 25-27 passim.
Parker JS, van Dijk K, Melles GR. Treatment options for advanced keratoconus: a review. Surv Ophthalmol. 2015;60(5):459-480.
van der Worp E, Bornman D, Ferreira DL, Faria-Riberio M, Garcia-Porta N, Gonzalez-Meijome JM. Modern scleral contact lenses: a review. Cont Lens Anterior Eye. 2014;37(4):240-250.
Carina Koppen, MD, PhD
• Associate Professor of Ophthalmology, University of Antwerp,Belgium
• carina.koppen@outlook.be
• Financial disclosure: None
