
It is essential for the surgeon to have a strategy and a clear vision in place before embarking upon surgery for a rock-hard cataract. Removing a hard cataract is like skating on thin ice, and the surgeon must take great care to avoid any trouble. Hard cataracts make preoperative assessment of intraocular structures difficult, and operating on them is an even greater challenge. The difficulty of these cases is compounded by a thin capsule and densely packed nuclear fibers, and they often require a longer surgical time than cataracts with less-dense nuclei. Therefore, it is extremely important for the surgeon to analyze preoperatively whether the eye can take the challenge and to choose the right technique for the case (Figure 1).
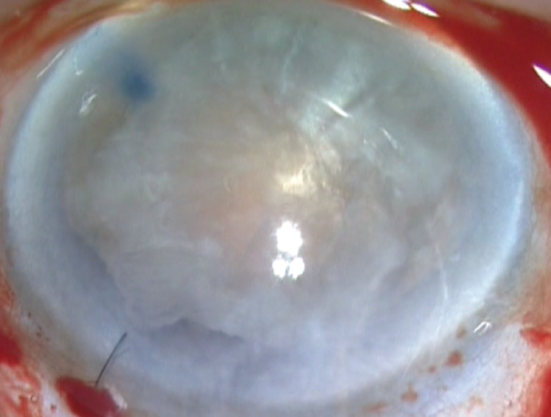
Figure 1. A hard cataract prolapsed into the anterior chamber.
Patients with hard cataracts must be well informed and advised preoperatively about all the possible outcomes of cataract surgery, especially when a guarded prognosis is anticipated, as in patients with ocular comorbidities. As with any surgery, patients with anxious personalities must be taken care of and comforted during the preoperative counseling process and also immediately before surgery. Managing such patients with slight sedation or an antianxiety drug on the day of surgery helps add to the comfort for both patient and surgeon.
AT A GLANCE
• In patients with hard cataracts, it is vital to assess the patient’s visual potential and to identify comorbidities.
• Preoperative tests should include eliciting pupillary response to light and checking for relative afferent pupillary defect.
• Checking preoperatively for phacodonesis and zonular compromise can be done with high-speed recording on an iPhone.
With the presence of a hard cataract, all of these factors influence the surgeon’s decision about which form of anesthesia to use and whether sedation is needed. It is always advisable to operate on hard cataracts under peribulbar anesthesia, and that is what I use in all of my cases.
STEPS IN ASSESSMENT
History and workup. To ensure a smooth outcome, it is important to elicit the patient’s systemic medication history, especially if he or she is on anticoagulants or, in men, drugs for prostate enlargement, as these can lead to intraoperative floppy iris syndrome (IFIS). Queries should elicit any previous episode of uveitis, as this helps to determine the best postoperative drug regime for the patient. Any history of drug hypersensitivity should also be obtained.
All the tests that are part of routine cataract preoperative workup should be performed in eyes with hard cataracts, including IOP measurement, ultrasound A-scan, pachymetry, fundus examination, and OCT.
There are also certain preoperative workups that require special mention for hard cataracts. Anterior chamber depth is an essential parameter that must be assessed in these eyes. If a patient has a shallow anterior chamber, I usually give intravenous mannitol at least 45 minutes before surgery. This helps to shrink the vitreous component and thereby to slightly deepen the anterior chamber. The additional advantage of preoperative mannitol is that, in case of an inadvertent posterior capsule rupture (PCR), vitreous loss can be curtailed to a certain extent.
Visual potential. The patient’s visual symptoms should always be analyzed to establish whether they are consistent with the presence of and correspond to the density of the cataract. It can be challenging to evaluate the visual potential of a patient with an advanced or mature cataract. However, a reliable estimate of retinal function can usually be obtained by testing the patient’s ability to interpret projection and perception of light from all quadrants. A structural evaluation with B-scan ultrasonography should be performed to provide a gross idea of the anatomic normality of the eye and to rule out any posterior segment pathology such as vitreous hemorrhage or retinal detachment.
Pupillary reflexes should be elicited, and the pupils should normally react briskly to light even in the presence of very hard cataracts. A sluggish response or a relative afferent pupillary defect hints at the possibility of optic nerve conduction defects that might lead to a poor postoperative visual outcome.
Specular microscopy. The endothelial cell count or endothelial cell density (ECD) reflects the status of the endothelium and its capacity to overcome any surgical trauma that might lead to decline in ECD. The morphology of the endothelium is equally important, and patients with poor endothelial morphology may require strategies to prevent further ECD loss, especially in eyes with hard cataracts. An OVD should be used to provide adequate endothelial protection, thereby minimizing trauma to endothelial cells. In the presence of Fuchs dystrophy, the approach to surgery should be aimed at causing minimal ECD loss postoperatively.
Slit-lamp examination. During this examination, the surgeon should assess the density of the cataract and the pupil size on dilation. A correlation between these two findings helps to decide whether pupil dilation devices will be needed during surgery. Associated features also help to judge the type of device that may be needed. For example, in cases in which I anticipate a struggle (Figure 2) or a complication such as a PCR, I prefer to use iris hooks, whereas in other cases I use the Malyugin Ring (MicroSurgical Technology). This is for the simple reason that, if a complication occurs in an eye in which a ring is being used, it is necessary to remove the ring and then manage the complication, whereas iris hooks can stay where they are and be removed only at the end of the surgery.
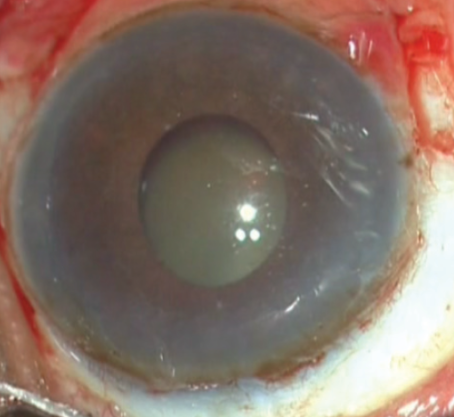
Figure 2. A hard cataract with a nondilating pupil and lens subluxation.
Evaluation at the slit lamp is also the time to look for lens subluxation and for the presence of vitreous in the anterior chamber (Figures 3 and 4). In eyes with hypermature hard cataracts with phacolytic glaucoma, the presence of lens matter in the anterior chamber can also be an associated feature (Figure 5).
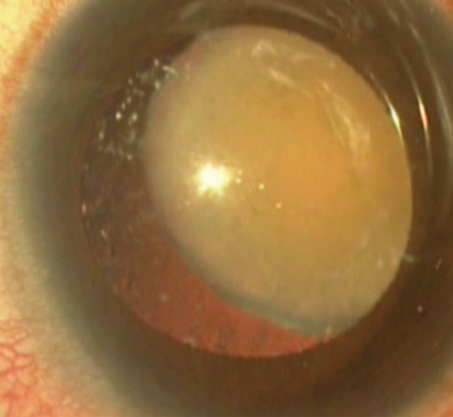
Figure 3. A hard cataract with massive lenticular subluxation.
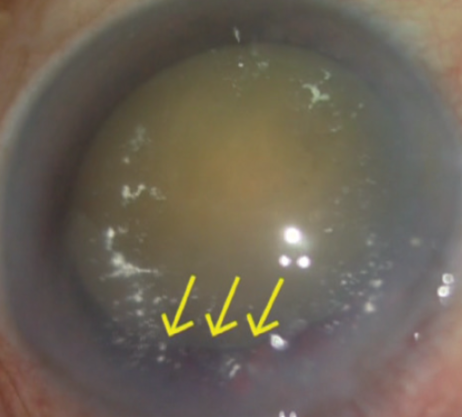
Figure 4. A hard cataract with compromised zonules (yellow arrows).
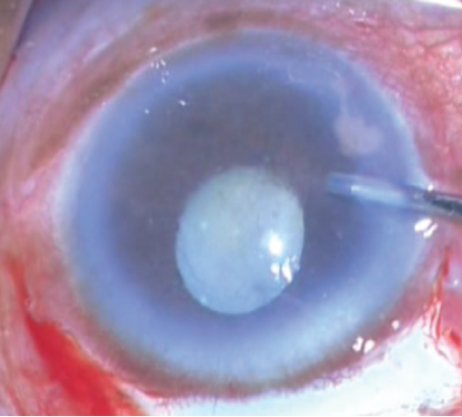
Figure 5. A hypermature cataract with phacolytic glaucoma and lens matter in the anterior chamber.
Assessment of phacodonesis. Often hard cataracts are associated with zonular compromise, and, in such cases, the surgical outcome can be optimized if phacodonesis can be assessed preoperatively. Taking this aspect into consideration, I introduced the concept of high-frame-per-second recording with an iPhone (Apple), which allows preoperative detection of even minimal phacodonesis.1 This method can apprise the surgeon of the clinical scenario beforehand and prevent intraoperative surprises.
Cataracts with zonular compromise often need support during surgery, and placement of a capsular tension ring in the bag helps to stabilize the zonular apparatus and also prevents the capsular phimosis that is often seen with hard cataracts. Additionally, this preoperative investigation allows the surgeon to gauge whether other devices may be required, so that he or she can have all such devices ready during surgery.
CHOOSING THE RIGHT TECHNIQUE
In recent decades, techniques for cataract extraction have been revolutionized, resulting in shortened recovery times and increased expectations for visual outcomes. To achieve these outcomes, it is crucially important that the surgeon chooses the right tool for the right job. As the saying goes, “We shape our tools, and thereafter our tools shape us.”
With very hard cataracts, it is often difficult to perform phacoemulsification, as the high energy required for the procedure might be detrimental to the corneal endothelium. A manual small-incision cataract surgery technique (Figure 6) or a simple extracapsular cataract extraction may suffice in such cases.
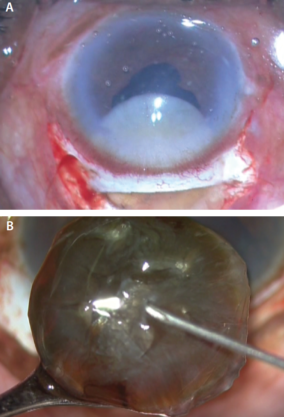
Figure 6. Small-incision cataract surgery being performed in hard, mature cataracts (A,B).
Trypan blue dye staining can be helpful in hard cataracts in which the glow from retroillumination is not sufficient. The contrast between the stained and the unstained capsule allows adequate visualization of the progression of the capsulorrhexis margin flap and facilitates its completion with precision.
CONCLUSION
Proper counseling regarding all the possible outcomes of surgery in the presence of a hard nucleus helps to improve patient satisfaction and also to set realistic preoperative expectations. It has been shown that ocular comorbidity and complications are major predictors of patient dissatisfaction.2 The patient’s understanding of the situation is an important factor in overall patient satisfaction in the treatment of a hard cataract.
1. Narang P, Agarwal A, Sanu AS. Detecting subtle intraocular movements: Enhanced frames per second recording (slow motion) using smartphones. J Cataract Refract Surg. 2015;41(6):1321-1323.
2. Yorston D. Are intraocular lenses the solution to cataract blindness in Africa? Br J Ophthalmol. 1998;82:469-471.


