
The introduction of optical biometry in the late 1990s revolutionized the exactitude of IOL power calculation. The major source of error in IOL choice and refractive results until then, the measurement of axial length (AL), suddenly became the most accurate and reliable parameter in the planning of a cataract procedure.
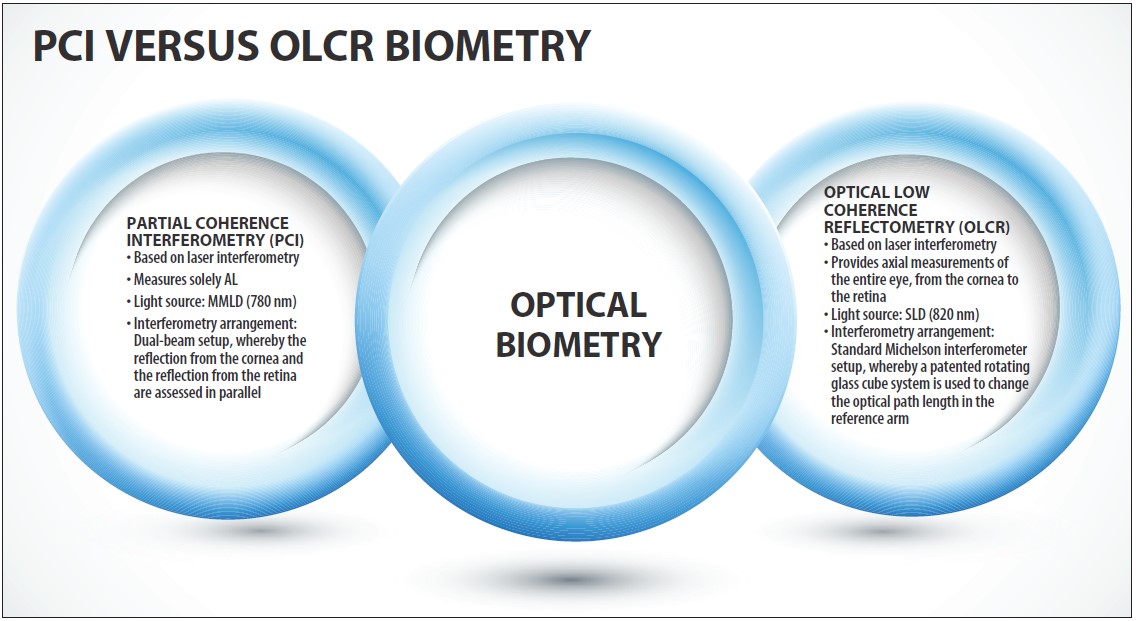
The first optical biometer introduced, the IOLMaster (Carl Zeiss Meditec), used the partial coherence interferometry (PCI) principle to measure solely AL. A decade later, Haag-Streit introduced another optical biometer, the Lenstar, based on its experience with its Pachµmeter (discontinued). Like the Pachµmeter, the Lenstar used optical low coherence reflectometry (OLCR), and it provided axial measurements of the entire eye—from the cornea to the retina—with laser precision. Thus, two devices designed for the same purpose used slightly different technologies.
Even today, almost 2 decades after optical biometry was introduced, some practitioners are uncertain of the main differences between PCI and OLCR biometry and of each technology’s pros and cons. This article aims to describe these variances in the hopes of helping cataract surgeons further their quests in accurate surgical planning and IOL power calculation (see PCI Versus OLCR Biometry).
TWO FUNDAMENTAL DIFFERENCES
Both PCI and OLCR are based on laser interferometry, first described by Albert Abraham Michelson.1 But PCI and OLCR differ in two fundamental details: their light sources and the optical setup of their interferometers. These two differences are also the reason why the OLCR biometer provides a full A-scan of the entire eye whereas the PCI biometer provides only a single parameter, the AL.
This article discusses the capabilities of the IOLMaster 500, the classic PCI optical biometer. It does not address the manufacturer’s more recently introduced IOLMaster 700 with swept-source OCT technology. (Editor’s Note: For a description of this technology, see IOLMaster 700: A Debut of Swept-Source OCT Technology.)
THE LIGHT SOURCE
The IOLMaster 500 and earlier models use a multimode laser diode (MMLD) at 780 nm. MMLDs provide a light spectrum with a discrete pattern of individual wavelengths (Figure 1A). The Lenstar OLCR biometer utilizes a superluminescent diode (SLD) at 820 nm. In contrast to an MMLD, the spectrum of an SLD is continuous (Figure 1B).
In the measurement process, MMLD generates secondary maxima for every structure it passes. For the PCI biometer, this means that every measurement signal creates repetitive side maxima in front of and behind the real measurement peak, at a separation of about 0.8 mm (Figure 2A). Specifically for the measurement of pseudophakic patients with certain IOL models, this might lead to difficulties in the detection of the correct AL peak.
SLD-driven biometers do not show these secondary maxima (Figure 2B) and therefore allow easy peak detection throughout the entire eye, permitting display of a full A-scan from the cornea to the retina, including pachymetry (central corneal thickness; CCT), anterior chamber depth (ACD), lens thickness (LT; also IOL thickness), and overall AL.
At a Glance
• With ever-evolving lens designs and increasing patient expectations, having the best possible measurements is key for successful surgery with satisfactory refractive results and happy patients.
• Both PCI and OLCR biometry are based on laser interferometry; however, these technologies differ in two fundamental details, their light sources and the optical setup of their interferometers.
• OLCR offers significant additional advantages for use of the latest state-of-the-art IOL formulas.
The difference in the wavelength of the light source used does not lead to any differences in device performance. Even though wavelength is associated with cataract penetration capability, no significant difference in this regard has been reported between the devices. The reported values for cataract penetration success rates are equivalent for PCI and OLCR biometry, ranging from 85% to 95% depending on cataract grades and patient demographics.2-5
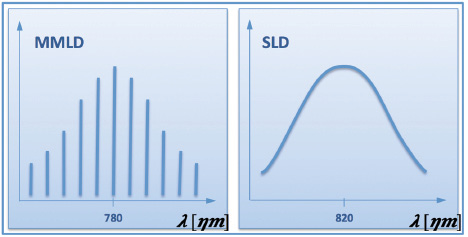
Figure 1. Schematic example of a discrete light spectrum emitted by an ideal multimode laser diode (MMLD; A). Schematic example of a continuous light spectrum emitted by an ideal superluminescent diode (SLD; B).
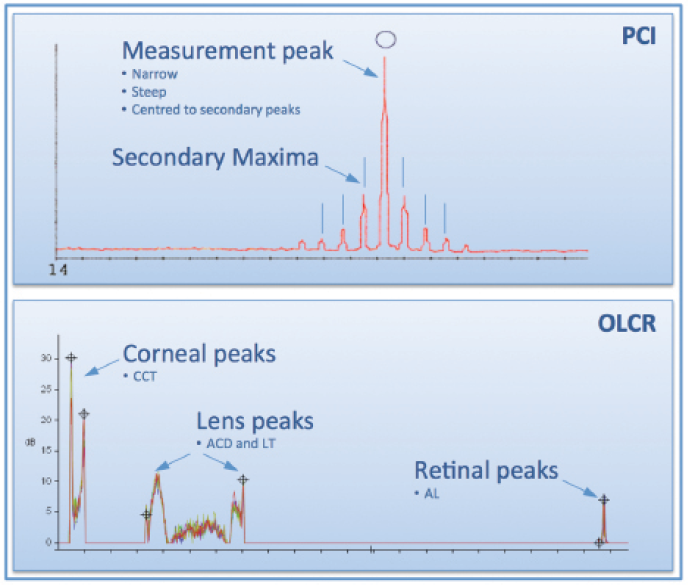
Figure 2. A-scan representation of a PCI biometer with the main measurement peak and the system-characteristic secondary maxima at about 0.8 mm from the main peak on each side (A). OLCR A-scan of an entire eye starting on the left with the two peaks for the cornea front and back surfaces, followed by anterior and posterior capsular bag of the lens, with some noise from nuclear cataract formation in between, and retinal peaks from the retinal pigment epithelium (RPE; main measurement peak for axial length) and internal limiting membrane just in front of the RPE peak (B).
THE INTERFEROMETER SETUPs
PCI and OLCR biometry are each based on individually patented interferometry arrangements. With PCI biometry, a dual-beam setup is used. In this arrangement, the reflection from the cornea and the reflection from the retina are assessed in parallel. The optical path length of the corneal signal is increased using a movable mirror, and the interference is detected when the optical path length of the signal from the cornea and the one from the retina are equivalent. Because the displacement of the mirror used to move the reflection from the cornea to the retina is known, the AL of the eye can be calculated using a group index of refraction for the entire eye.6 The advantage of this setup is that the measurement of the AL is motion-independent, and the operating distance from the device to the patient can vary significantly because only one structure is measured.
OLCR biometry uses a standard Michelson interferometer setup equipped with a measurement path (ie, the patient’s eye) and an internal reference path. To allow the measurement of a large structure such as the human eye with this setup at high scanning rates, OLCR uses a patented rotating glass cube system to change the optical path length in the reference arm.7 This configuration enables the acquisition of a full A-scan of the entire eye at a fast scanning speed. Additionally, built-in signal processing minimizes possible motion artifacts. The A-scan is represented in a manner similar to the display seen with immersion ultrasound, allowing the user easy navigation. If desired, each individual peak can be adjusted (Figure 2).
For CCT, ACD, and LT, individual indices of refractions are used to generate geometric readings from the optical path lengths acquired. In its current implementation, OLCR biometry provides the AL also based on a group index of refraction, equivalent to PCI biometry. For research purposes, the incremental optical path lengths, composed of the sum of the individual compartments of the eye, are accessible;8 this allows assessment of the dimensions of every compartment of the eye based on unbiased optical path length data. The availability of this detailed information might lead to new innovations, such as the statistical IOL calculation model presented by Warren E. Hill, MD, in his 2014 Charles D. Kelman lecture.9
SUMMARY AND CONCLUSION
Almost 2 decades ago, PCI biometry revolutionized cataract surgery, with its precise and user-friendly method of AL measurement. It set the gold standard for optical biometry and was the first device to provide this key parameter for cataract surgery with laser precision. Optical biometry soon became the choice for axial measurement in relation to cataract interventions.
OLCR biometry was the logical consequence of PCI, providing users with more information on the patient’s eye yet maintaining the same levels of precision and usability as PCI biometry.3,4,10 With precise information on AL, CCT, ACD, and LT, the surgeon can take full advantage of the latest developments in IOL calculation formulas (eg, Barrett, Holladay 2, and Olsen). Using additional parameters, specifically LT, these new formulas for IOL prediction allow significant improvement in the accuracy of planning the cataract intervention.
With ever-evolving lens designs and increasing patient expectations, having the best possible measurements is key for successful surgery with satisfactory refractive results and happy patients.
In conclusion, both PCI and OLCR biometry are precise technologies for accurate planning of cataract surgery, and both devices also measure the keratometry values of the cornea (not with laser). However, OLCR offers significant additional advantages for use of the latest state-of-the-art IOL formulas. n
1. Michelson A, Morley E. On the relative motion of the Earth and the luminiferous ether. Am J Sci. 1887;34(203):333-345.
2. Chen YA, Hirnschall N, Findl O. Evaluation of 2 new optical biometry devices and comparison with the current gold standard biometer. J Cataract Refract Surg. 2011; 37(3):513-517.
3. Buckhurst PJ, Wolffsohn JS, Shah S, Naroo SA, Davies LN, Berrow EJ. A new optical low coherence reflectometry device for ocular biometry in cataract patients. Br J Ophthalmol. 2009;93(7):949-953.
4. Rohrer K, Frueh BE, Wälti R, Clemetson IA, Tappeiner C, Goldblum D. Comparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometer. Ophthalmology. 2009;116(11):2087-2092.
5. McAlinden C, Wang Q, Pesudovs K, et al. Axial length measurement failure rates with the IOLMaster and Lenstar LS 900 in eyes with cataract. PLoS One. 2015;10(6):e0128929. doi: 10.1371/journal.pone.0128929.
6. Santodomingo-Rubido J, Mallen EA, Gilmartin B, Wolffsohn JS. A new non-contact optical device for ocular biometry. Br J Ophthalmol. 2002;86(4):458-462.
7. Schmid GF. Axial and peripheral eye length measured with optical low coherence reflectometry. J Biomed Opt. 2003;8(4):655-662.
8. Suheimat M, Verkicharla PK, Mallen EA, Rozema JJ, Atchison DA. Refractive indices used by the Haag-Streit Lenstar to calculate axial biometric dimensions. Ophthalmic Physiol Opt. 2015;35(1):90-96. doi: 10.1111/opo.12182.
9. Hill WE. Something borrowed, something new: Improved accuracy for IOL selection. Paper presented at: the American Society of Cataract and Refractive Surgery Annual Meeting; April 25-29, 2014; Boston, MA.
10. Hoffer KJ, Shammas HJ, Savini G. Comparison of 2 laser instruments for measuring axial length. J Cataract Refract Surg. 2010;36:644-648.
David Goldblum, MD
• Head of Anterior Segment and Oculoplastics, Department of Ophthalmology, University Hospital Basel, Switzerland
• david.goldblum@usb.ch
• Financial disclosure: Lecture honoraria (Haag-Streit)
