

Small-incision lenticule extraction (SMILE) is the latest addition to mainstream corneal refractive surgery. Tissue depth per diopter of correction with SMILE is roughly equivalent to that with PRK and LASIK. Unlike in LASIK and PRK, however, in SMILE a femtosecond laser (VisuMax, Carl Zeiss Meditec) is used to dissect a lens-shaped portion of stromal tissue for refractive correction, followed by manual removal of that lenticule (see video below).
FINE-TUNING THE SETTINGS
In our clinical experience with SMILE, the ease of lenticule dissection is directly related to the speed of the patient’s visual recovery. Typically, the less force needed, the faster the recovery.
The adjustability of the laser’s spot spacing, track spacing, and laser energy level allow the surgeon to expand the transition zone of the lenticule dissection. Additionally, the incision angle may now be as small as 60º, representing a potential one-third reduction in the cutting of superficial nerves.
A common observation is that not all femtosecond lasers are the same. Mirrors become worn over time, or environmental factors can alter effectiveness. The result is a lack of plug-and-play setting optimization. Each laser must be separately optimized. Most US SMILE surgeons are now in the process of optimizing their settings, which holds promise for achieving smoother dissections and allowing faster visual recovery in the future.
As they optimize their settings, many surgeons are finding success using spot and track spacing in the range of 4.2 to 4.5 µm and energy levels of 125 to 150 nJ. Most are now also using the smaller, 2-clock-hour incision angle.
If SMILE surgeons are now able to achieve significant improvements in healing speed as the lasers are optimized, it would not be the first time the refractive market has noted such improvements. Early ophthalmic femtosecond lasers used for LASIK flap creation struggled to compete with microkeratomes regarding corneal clarity. Today, however, femtosecond lasers provide excellent visual results with a level of safety that no microkeratome could ever match. We now can inspect flap quality before the tissue bridges are released upon lifting the flap.
what’s on the horizon?
SMILE is impressive in that it has already become a rival to LASIK in a short time. Just like other forms of vision correction, it will continue to improve (see “Six Tips for Getting Started With SMILE”). LASIK, PRK, phakic IOLs, and lens-based refractive surgery are all significantly better today than their first generations, and SMILE is already better than it was just a few years ago.
SIX TIPS FOR GETTING STARTED WITH SMILE
Tip No. 1: Start with moderate to high myopes. Because the nonrefractive component of the lenticule cannot yet be modified in the United States, selecting these patients allows use of a thicker lenticule and permits easier dissection. Energy settings that have not been optimized can more easily affect the results with thinner lenticules.
Tip No. 2: Optimize energy settings. This is where SMILE and LASIK flaps differ. Because in SMILE the refractive treatment is done by the femtosecond rather than the excimer laser, improper energy settings can cause a rougher interface and an opaque bubble layer, which results in difficult dissection and slower visual recovery. In general, lower is better, but setting the energy too low can result in black spots of incomplete treatment, leading to rougher surfaces and difficult dissection. This all affects the patient’s rate of visual recovery and the final result.
Tip No. 3: Recognize the importance of cap distention. Microdistortions cause slow visual recovery and poor visual outcomes,1 as they do in LASIK. In the experience of one of us (R.L.R.), this process requires more manipulation than a LASIK flap would require.
Tip No. 4: Pay attention to centration. There is no pupil tracker or iris registration for SMILE. This allows the surgeon to have perfect control over the treatment centration, but it also requires the surgeon to have perfect control over the treatment centration. The importance of this step cannot be overstated. There are many devices that help with centration, including the AcuTarget HD (Visiometrics), Pentacam (Oculus Optikgeräte), Orbscan (Bausch + Lomb), and others. Corneas should be marked at 0° and 180° (and more axes if needed) to account for cyclorotation. One of us (O.B.W.) particularly advises first becoming comfortable with the low-suction, curved interface of the femtosecond laser for LASIK flaps before attempting the first SMILE case.
Tip No. 5: Have a strategy—including dissecting the anterior plane first—but know how to make a rescue. Most surgeons will find themselves in the posterior plane before the anterior plane at some point. This does not affect visual recovery, but it can make dissecting the anterior plane more difficult. Learn the rescue technique, as demonstrated in the video at the top of the article and depicted in Figures 1 through 3.
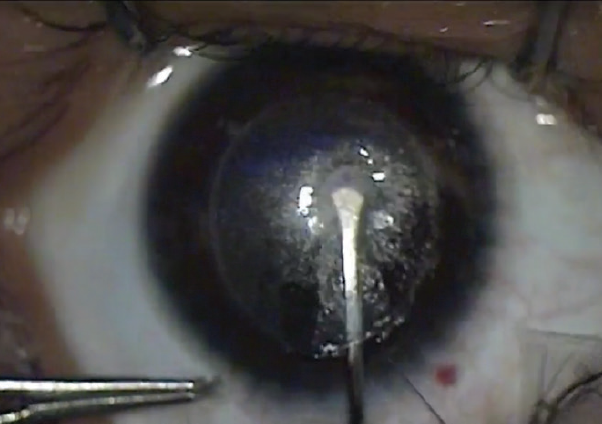
Figure 1. Perceived anterior dissection but in the posterior plane.
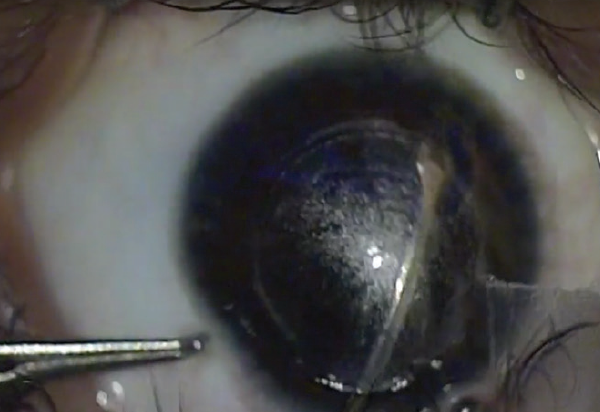
Figure 2. A visible bubble in the anterior segment is a clue that you are in the posterior plane.
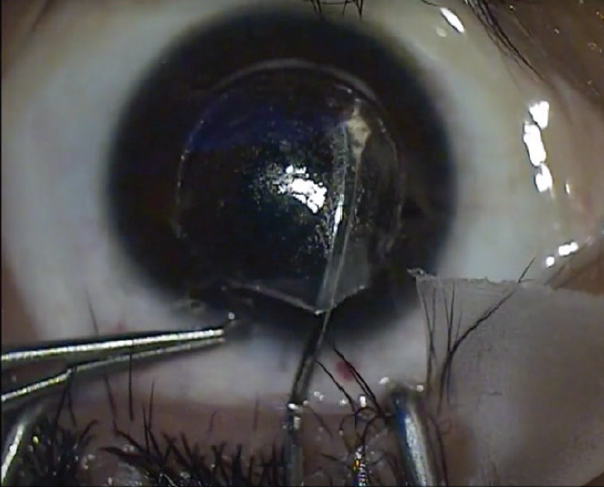
Figure 3. Rescue technique to find and dissect the anterior plane.
Tip No. 6: Have an excimer laser available. It is not a failure to convert to LASIK if you encounter an opaque bubble layer, a suction break, or a difficult dissection. Many times, LASIK can be performed on the same day, but waiting for another day can sometimes be a better option. This is a possibility we discuss with all SMILE patients as part of the informed consent process out of an abundance of preparation and precaution.
1. Reinstein DZ, Archer TJ, Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vis (Lond). 2014;1:3.
There are many things to look forward to in the future of SMILE.
Unlocking parameters. We look forward to having the ability to vary the thickness of the lenticule, change the location and size of the primary incision, vary the cap thickness to allow LASIK enhancements, and change energy settings even further.
Treating hyperopia and aberrations. Studies are already being done for hyperopia.
Developing new techniques. New ideas are always being generated.
conclusion
It is exciting to have another option for laser vision correction. As the articles in this cover focus look to the future of ophthalmology, it is helpful to keep in mind that SMILE will perform best when we evaluate each patient as an individual to determine the optimal personalized treatment modality for that patient. Let us hope that the future of ophthalmology makes room for all safe and effective refractive surgical options so that we can best serve each patient.
We look forward to future iterations of SMILE.
1. VisuMax Femtosecond Laser. Small incision lenticule extraction (SMILE) procedure for the correction of myopia. Professional use information. Carl Zeiss Meditec. 2016. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150040D.pdf. Accessed May 2, 2019.
2. Premarket approval. US Food and Drug Administration. VisuMax Femtosecond Laser. Femtosecond laser system for refractive correction. October 25, 2018. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150040S003D.pdf. Accessed May 2, 2019.
3. Reinstein DZ, Archer TJ, Randleman JB. Mathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extraction. J Refract Surg. 2013;29(7):454-460.
4. Hou J, Wang Y, Lei Y, Zheng X. Comparison of effective optical zone after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2018;44(10):1179-1185.
5. Chiche A, Trinh L, Saada O, et al. Early recovery of quality of vision and optical performance after refractive surgery: Small-incision lenticule extraction versus laser in situ keratomileusis. J Cataract Refract Surg. 2018;44(9):1073-1079.


