
The most commonly used treatment paradigm in laser vision correction is the application of an ablation pattern on the cornea to correct manifest refraction sphere and cylinder. Corrections based on wavefront refraction employ a similar paradigm, though they take the refraction from a wavefront aberrometer—an objective device to measure the refractive status of the eye—rather than from manifest refraction, which includes the perceptual component.
These two modes of treatment have one thing in common: a disregard for differences between refractive and corneal astigmatism parameters. When the differences in refractive and corneal astigmatism are significant, as quantified by ocular residual astigmatism (ORA),1 both modes of treatment will cause the differences (ie, the ORA) to be sculpted onto the cornea as postoperative astigmatism to neutralize the internal aberrations.
There is a flaw in these 100% refractive-based treatment paradigms: There is no limit to how much astigmatism will be left on the cornea when the preoperative corneal/refractive differences are not taken into account before the refractive surgery ablation is performed. Preoperative ORA has been found to be greater than 1.00 D in 34% to 46% of eyes undergoing LASIK.1,2 With traditional refractive-based treatments, therefore, this would leave greater than 1.00 D of residual corneal astigmatism postoperatively (see Case Study). Without an ORA assessment preoperatively, this could result in astigmatism in magnitudes on the order of 2.00 to 3.00 D being targeted to the cornea.
Case Study
A 34-year-old man presented to my practice after undergoing LASIK with another surgeon. He reported symptoms of glare, ghosting, starbursts, and halos with a loss of contrast sensitivity, a syndrome referred to by the acronym GASH. Preoperatively, the patient had myopic astigmatism with a BCVA of 20/20 in each eye with regular topography.
Postoperatively, his UCVA was 20/20 in each eye with no refractive error, but he could drive at night only by shining his cell phone flashlight in his eyes to reduce his pupil size and thereby reduce his GASH symptoms. He had more than 1.00 D of corneal astigmatism in each eye postoperatively because he had undergone LASIK treatment based on traditional 100% refractive parameters.
NEW SYNDROME: PALS
This newly described syndrome,3 in which the patient’s preoperative ORA is greater than 1.00 D and there is more than 1.00 D of corneal astigmatism postoperatively, together with one or more GASH symptoms (described in Case Study), I have termed predictable, avoidable LASIK surprise (PALS).
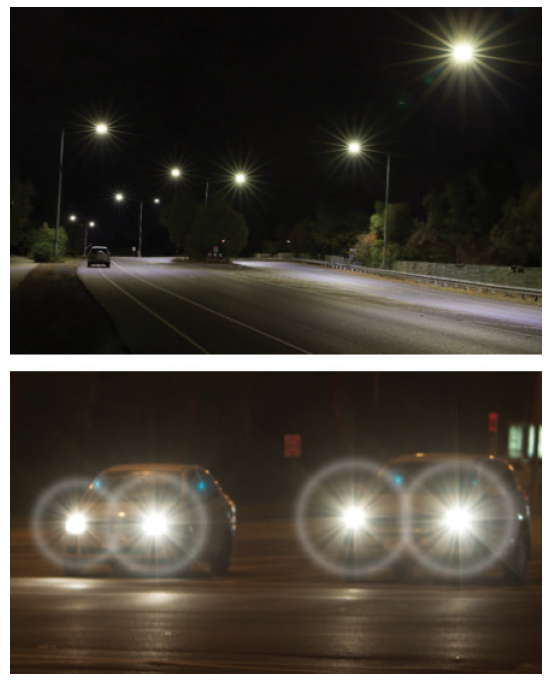
Figure. GASH can occur due to excess corneal astigmatism after LASIK.
PALS is predictable due to high preoperative ORA and avoidable because incorporating corneal parameters into the treatment plan using Vector Planning (a registered trademark of ASSORT) would reduce the postoperative corneal astigmatism and, hence, the visual symptoms of GASH (Figure). I include LASIK in the PALS acronym because it is the predominant refractive laser surgery procedure, but PALS can also occur after PRK and SMILE procedures (see When Does PALS Syndrome Occur?).
When Does PALS Syndrome Occur?
- Preoperative ocular residual astigmatism and postoperative corneal astigmatism are greater than 1.00 D
- Patient experiences one or more symptoms of glare, ghosting, starbursts, halos, and loss of contrast (GASH) postoperatively
Vector Planning can avoid PALS syndrome
- Calculate ORA preoperatively, and
- Treat based on both corneal and refractive parameters
AVOIDING PALS
PALS can be avoided using the technique of Vector Planning,1,3,4 in which both corneal and refractive parameters are used in creating a treatment plan. With this technique, residual corneal astigmatism could be reduced by 41%, as demonstrated by Arbelaez et al in a 2017 publication.5 Those study authors compared the use of Vector Planning with treatment using refractive parameters alone and noted superior visual results in eyes treated based on Vector Planning, with 41% less corneal astigmatism than in those treated with refractive parameters only. The mean refractive cylinder postoperatively was equivalent in the two groups. The Amaris 1050 (Schwind eye-tech-solutions) was used in that study, the same advanced laser that was used in the treatment of the eyes discussed in the sidebar Case Study.
The symptoms associated with GASH as a result of excess astigmatism on the cornea have been frequently cited in patient complaints about LASIK submitted to the US FDA.6 A report in The New York Times,7 and social media posts describing and discussing these distressing patient experiences have also drawn attention to these symptoms.
A SAFE BUTTON
None of the lasers currently in use for the treatment of LASIK limit corneal astigmatism after laser vision correction, and this parameter is not considered in routine treatments worldwide, which are based on refractive parameters alone. Considering the prevalence of GASH symptoms among the complaints of dissatisfied patients, likely due to excess postoperative corneal astigmatism, it would be beneficial to have a Safe button on every laser, which would provide a low-astigmatism mode or Vector Planning mode to ensure that both corneal and refractive cylinder are used in the treatment plan. This is true for all types of laser vision correction, not only LASIK but also PRK and SMILE.
Surgeons can perform the necessary calculations on the free-to-use ORA and Vector Planning calculator available at www.isrs.org for all laser vision corrections that require the correction of astigmatism. They and their patients can benefit from a more than 40% reduction in corneal astigmatism, optimal reduction in the refractive cylinder, and from reduction of the risk that their patients will experience the predictable, avoidable LASIK surprise of GASH.
1. Alpins NA. New method of targeting vectors to treat astigmatism. J Cataract Refract Surg. 1997;23(1):65-75.
2. Frings A, Katz T, Steinberg J, et al. Ocular residual astigmatism: Effect of demographic and ocular parameters in myopic laser in situ keratomileusis. J Cataract Refract Surg. 2014;40:232-238.
3. Alpins N. Vector planning method: Residual astigmatism minimised—LASIK surprises avoided. Paper presented at: the American Academy of Ophthalmology Annual Meeting; October 12-15, 2019; San Francisco.
4. Alpins N. Practical astigmatism planning and analysis. Thorofare, NJ: Slack; 2018.
5. Arbelaez MC, Alpins N, Verma S, et al. Clinical outcomes of laser in-situ keratomileusis with an aberration -neutral profile centred on the corneal vertex comparing vector planning with manifest refraction planning for the treatment of myopic astigmatism. J Cataract Refract Surg. 2017;43:1504-1514.
6. LASIK Complaints Filed With the FDA. Available at: www.lasikcomplications.com/lasik-complaints.htm. Accessed February 20, 2019.
7. Rabin RC. Blurred vision, burning eyes; This is a LASIK success? The New York Times. https://www.nytimes.com/2018/06/11/well/lasik-complications-vision.html. June 11, 2019. Accessed October 4, 2019.


