CASE PRESENTATION
A 66-year-old man presents with a desire to reduce his refractive error and improve his distance visual acuity. The patient’s history is significant for a Russian-style eight-incision radial keratotomy (RK) using a 2.75-mm optical zone in 1992.
Upon examination, the corneas appear to be normal except for the RK. Manifest refractions are stable and do not fluctuate from morning to evening. UCVA is 20/100 OD and 20/40 OS. BCVA is +1.25 +1.50 x 018º = 20/30 OD and +0.50 +0.25 x 115º = 20/25 OS.
The slit-lamp examination is notable for RK using a small optical zone, with obvious decentration of the optical zone and irregular incisions. A Tecnis 1-Piece IOL (model ZCBOO, Johnson & Johnson Vision) is well centered in each eye. No retinal pathology is evident, and the patient has no systemic diseases. The posterior capsule of each eye is intact and clear (Figures 1 and 2).
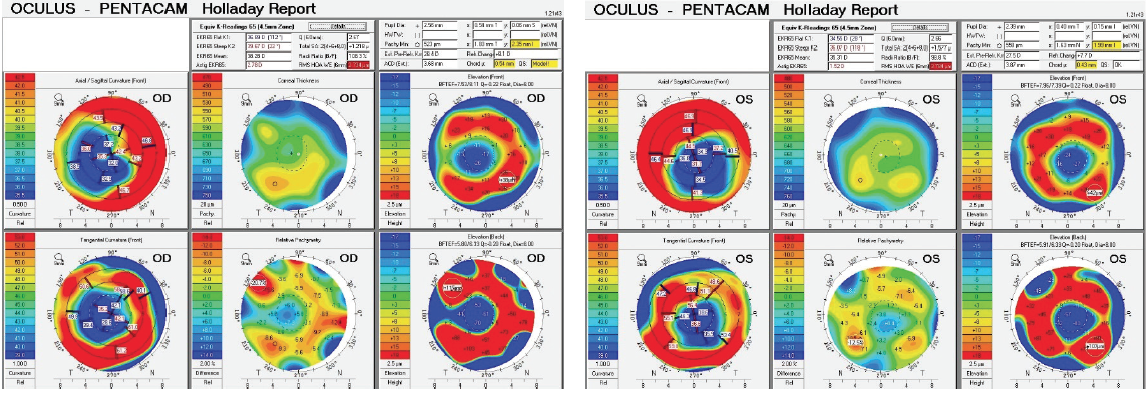
Figure 1. Holladay Reports from the Pentacam (Oculus Optikgeräte) for the right and left eyes.
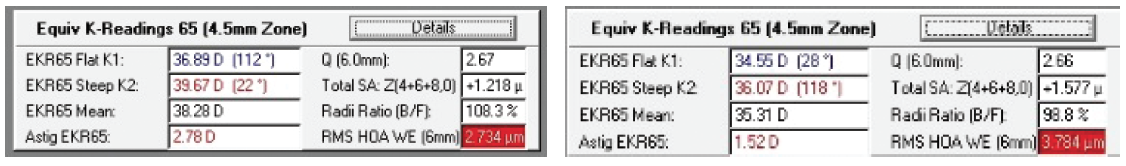
Figure 2. RMS HOA data show the patient’s distorted corneas.
How would you proceed?
—Case prepared by Karl G. Stonecipher, MD

H. BURKHARD DICK, MD, PHD, FEBOS-CR
This case is certainly a harbinger of things to come. During the next few years, we can expect to see a large number of men and women who, in their younger days, were a part of the first generation to undergo refractive surgery using methods considered revolutionary then but that seem rather crude today. For pseudophakic eyes with irregular RK incisions and a decentered optical zone, I tend to avoid scleral lenses and photoablative techniques because controlling the effects of laser vision correction (LVC) can be challenging and there is considerable risk of complications with LVC, even if ablation guided by corneal ray tracing could be performed.
My preferred strategy is based on a principle first described by the Chinese philosopher Mo-Ti in the 5th century BC and elaborated upon by Christoph Scheiner in the 17th century: the pinhole. Several surgical optical technologies use a small aperture to achieve an extended depth of focus, improve near visual acuity, and neutralize astigmatism. These include corneal inlays (Kamra, CorneaGen), IOLs (IC-8, AcuFocus), and other implants (XtraFocus Pinhole Implant, Morcher).
For this patient, I would use the XtraFocus, a small-aperture diaphragm made of a hydrophobic material whose optic portion incorporates a black mask with a 1.3-mm central opening. Its overall diameter is 14 mm. The device is implanted in the sulcus and blocks visible light but, interestingly, not infrared wavelengths. Although an Nd:YAG laser capsulotomy is possible with the device in place, I would perform the capsulotomy before implanting an XtraFocus. I strongly recommend using a cylindrical rod tip for insertion rather than a flat rod tip, which I have found has a tendency to go under this very thin device.
Once in place, the XtraFocus does not prevent a thorough examination of the posterior segment, but there is a learning curve to the technique. I should note that the XtraFocus, like the IC-8, can achieve good outcomes in eyes with large iris defects.1
It will be important to counsel this patient that his nighttime visual acuity will be reduced—not surprising with a pupillary opening of 1.3 mm. What is surprising is the amount by which retinal sensitivity has increased in patients after about 6 months, as recently described by Artal and colleagues.2,3 After thorough informed consent, I would implant the XtraFocus in the nondominant eye. If the patient is happy with the outcome, I would discuss a potential IOL exchange for an IC-8 IOL in the dominant eye. If on the contrary the patient is dissatisfied, the XtraFocus could be removed.

MICHAEL MARINO, OD
This case presents two potential problems for the patient. First, he may be experiencing a reduction in BCVA with spectacles. Second, he may be experiencing glare from the RK incisions and the small treatment zone.
In these situations, I generally start by fitting scleral contact lenses (Zenlens, Alden Optical). I would use an oblate design in this case because of the flat central corneas. It will even out the lens clearance over the entire cornea. Too much clearance centrally will reduce oxygen transmissivity, which could lead to neovascularization along the incision scars. A scleral lens creates a stable optical surface, which gives patients the best possible visual acuity. Depending on the amount of residual astigmatism, multifocal correction could be possible as well. Another benefit of scleral lenses is their effectiveness at treating dry eye.
Even when scleral contact lenses provide adequate visual acuity, patients such as this one may be bothered more by glare than by reduced visual acuity. To these patients, I recommend prosthetic soft BioColors contact lenses (Orion Vision Group). They may not give patients the best visual acuity because of the limitations of soft contact lenses, but they can be made with an opaque underprint, which is effective at reducing glare.

ALEKSANDAR STOJANOVIC, MD, PHD
Probably owing to 3 decades of neural adaptation, the patient does not mention reduced quality of vision as a symptom despite objectively quite distorted corneal optics, which probably makes treating the corneal higher-order aberrations (HOAs) unnecessary. Moreover, corneal surgery may disturb the current biomechanical balance of the compromised cornea, which must be considered when choosing between a corneal and a noncorneal approach to correcting the refractive error. I would most likely choose a noncorneal approach in this case, but, because therapeutic corneal laser surgery is my main sphere of interest, I will discuss LVC.
Regarding technique, LASIK should automatically be excluded for two reasons. First, it hazards creating a poor-quality flap that resembles pizza slices. Second, treatment that will have the lowest possible biomechanical impact is preferable. Among surface ablation techniques, classic epithelial removal is also contraindicated because of the pronounced epithelial remodeling to be expected in this case; any ablation plan based on measurements taken with the epithelium on—but applied after epithelial removal—would result in a significant error because of the difference in landscape.
The options remaining are transepithelial wavefront-optimized laser ablation based on the manifest refraction and topography-guided ablation (TGA), for which programming of the spherocylindrical endpoint may be challenging. Because TGA will correct anterior corneal HOAs, the effects of spherical aberration subjectively refracting as sphere and odd-order aberrations as cylinder will be removed. This must be accounted for by subtracting this effect from the manifest refraction to avoid a double correction (Figures 3–6). Significantly distorted posterior corneal optics are another problem that cannot be addressed unless total (anterior and posterior) corneal ray tracing–guided ablation is performed. It is to be hoped that this option will soon be available.
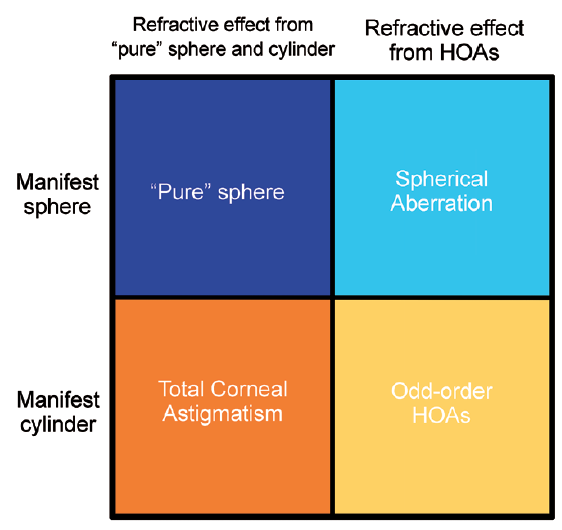
Figure 3. Components of the manifest refraction in eyes with highly irregular corneas (with lenticular astigmatism taken out of the equation). Manifest sphere = pure sphere (dark blue) + spherical aberration refracting as sphere (light blue). Manifest cylinder = total corneal cylinder (orange) + odd-order HOAs refracting as cylinder (yellow).
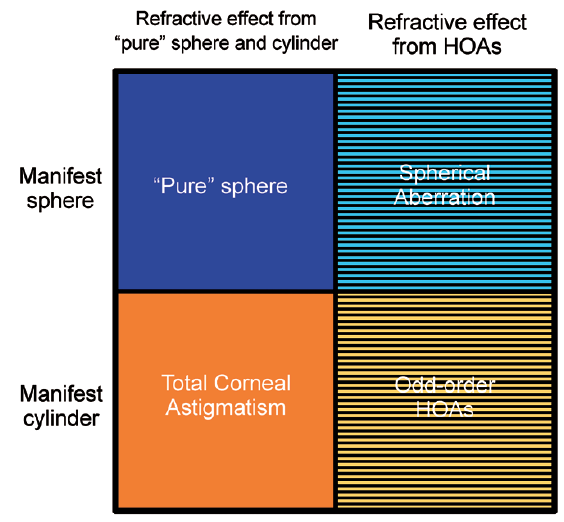
Figure 4. TGA programmed to treat zero sphere and cylinder will still treat anterior corneal HOAs (including asphericity) and will remove their effect (horizontal stripes).
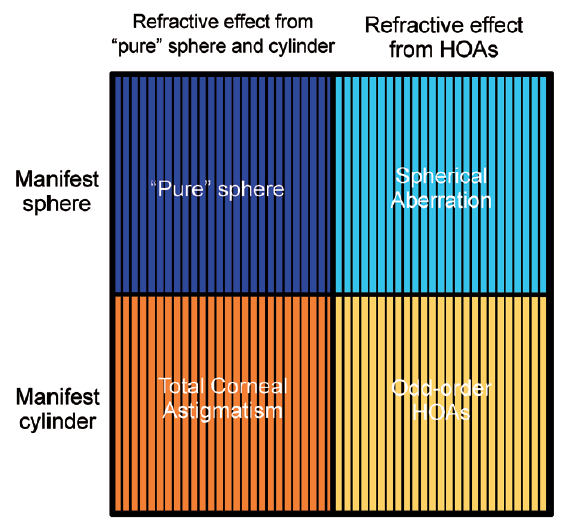
Figure 5. TGA programmed to treat total corneal astigmatism and pure sphere will remove all the components of manifest refraction (vertical stripes).
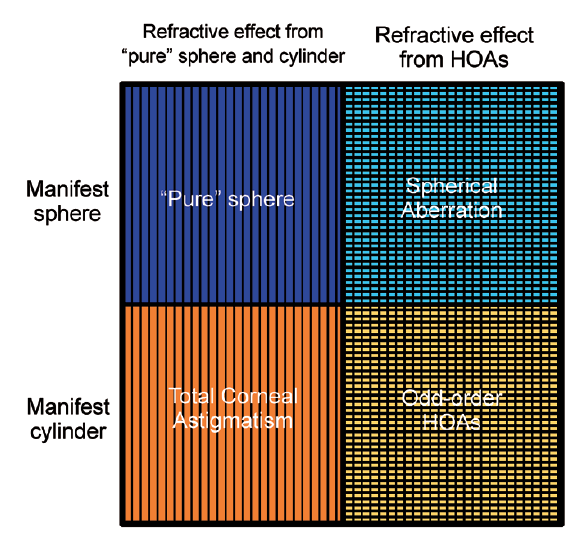
Figure 6. TGA programmed to treat manifest sphere and cylinder will treat all the components of the manifest refraction (vertical stripes), but, because treating the anterior corneal HOAs will also remove their effect on the manifest refraction, treatment will be doubled (area covered by both horizontal and vertical stripes), addressing both the cause and the effect of HOAs. A residual refractive error consisting of astigmatism inverse to the refractive effect of the odd-order HOAs and the sphere inverse to the refractive effect of the spherical aberration will be induced.
Figures 3–6 courtesy of Aleksandar Stojanovic, MD, PhD


