
Every refractive cataract practice has some patients who are unhappy with their vision after receiving presbyopia-correcting IOLs. Ideally, steps that we surgeons take preoperatively minimize the chance of postoperative dissatisfaction, but it’s important for us to have some tools on hand to address problems when they occur.
AN OUNCE OF PREVENTION
Setting expectations. The primary preventive strategy is to set realistic patient expectations. I tell patients that IOL surgery can reduce but not eliminate their dependence on spectacles. I also tell them to expect to experience halos, glare, and/or starbursts around lights at night. Patients are shown illustrations of dysphotopsia symptoms. When patients understand before surgery that night vision symptoms are a possibility after surgery, I find they are less likely to consider dysphotopsias to be a complication. I say, “These phenomena shouldn’t limit your vision, but if you find them bothersome, be sure to let me know.”
Patient selection. It’s important to identify appropriate candidates for presbyopia-correcting IOLs through a thorough diagnostic workup. Irregular astigmatism and other corneal abnormalities, epiretinal membrane, and macular degeneration are contraindications for multifocal IOLs. Individuals with a history of LASIK may be candidates for a multifocal IOL if the ablation was well centered and higher-order aberrations are minimal. Ocular surface disease (OSD) should be diagnosed and treated before surgery to enhance the accuracy of biometry and maximize vision quality after surgery.
DISSATISFACTION AT DISTANCE
When patients are unhappy after surgery, telling them that everything is fine is a brush-off. A better strategy is to bring these patients back in quickly so that the source of the complaint can be identified and addressed. Much of the preoperative testing is repeated to determine if a diagnosis of OSD or retinal disease was missed or the condition has worsened. In either situation, the disease is treated. Patients who report fluctuating vision usually have an unhealthy ocular surface, so they are offered treatments such as lubrication, punctal occlusion, and lid hygiene to achieve stable vision.
I have found the most common source of blurry distance vision and bothersome night vision symptoms to be residual refractive error. Even a small amount of residual astigmatism can compromise multifocal IOL optics. In my practice, a LASIK or PRK enhancement, when warranted, is offered free of charge to patients who elected a premium IOL. Enhancements are how I most frequently address problems after surgery with a premium IOL. I perform laser vision correction after the eye has stabilized. Until then, I reassure patients that I understand the source of their problem and can fix it, and if necessary, I prescribe glasses or contact lenses for them to use in the interim.
DISSATISFACTION AT NEAR
Reassuring an unhappy premium IOL patient can be more challenging when they don’t achieve the near vision they expected after surgery. Perhaps the lens or combination of lenses implanted allows them to work at a computer and drive, but they can’t read in bed at night and are unhappy about that. Several IOLs, including the Tecnis Eyhance and Tecnis Symfony (both from Johnson & Johnson Vision), AcrySof IQ Vivity (Alcon), and ActiveFocus multifocal toric (Alcon), are specifically designed with lower add powers to provide a better quality of distance vision and fewer night vision symptoms than are typically obtained with a bifocal or trifocal IOL. These advantages, however, require sacrificing some near vision.
If residual astigmatism, macular issues, and OSD are ruled out, a contact lens trial is performed in one eye to evaluate whether a mini-monovision strategy with PRK or LASIK would improve their near vision. A surgical fix, however, may not be an option if the patient has dry eye disease or cannot tolerate monovision. In this situation, one option is to prescribe pupil-modulating presbyopia-correcting drops. Pilocarpine HCL ophthalmic solution 1.25% (Vuity, Allergan) is approved by the FDA, and others are in clinical trials.
The miotic effect of presbyopia-correcting drops can provide better depth of focus for near vision. A smaller pupil can also reduce the effect of corneal irregularities and higher-order aberrations, thereby improving the quality of vision at all distances.1-3 The pupil-modulating drops that are currently and soon to be on the market have advanced vehicle formulations and delivery techniques, but their active ingredients—agents such as pilocarpine, carbachol, and brimonidine—have well-established safety profiles (Table). I therefore don’t have significant concerns about prescribing the drops to individuals who may be able to benefit from them, including pseudophakic patients who would like more functional near vision.
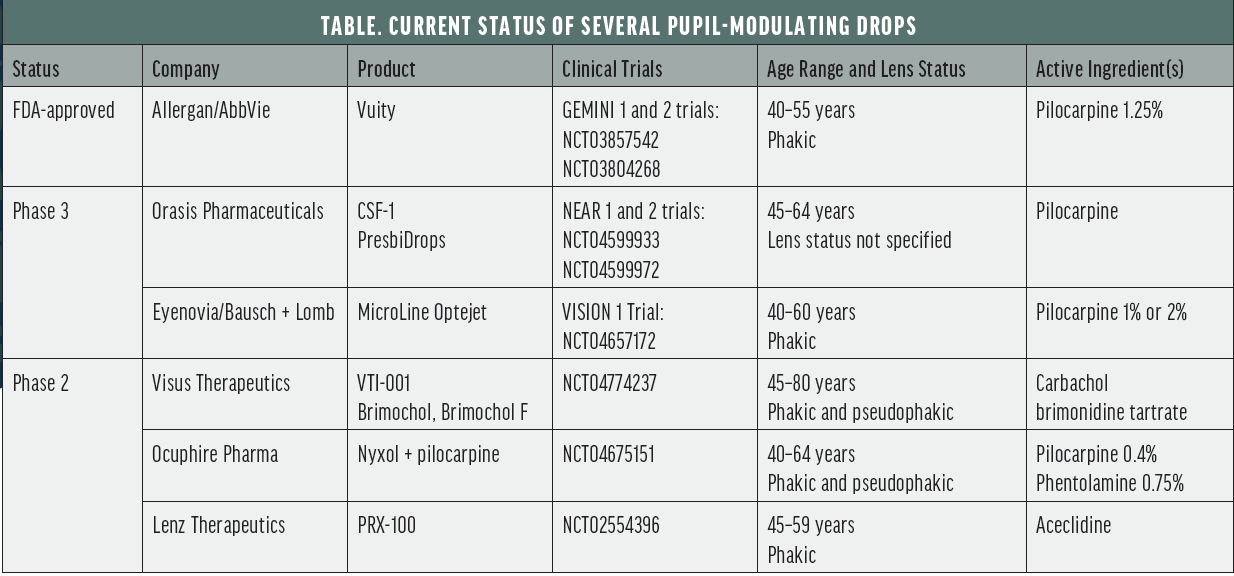
As we begin to prescribe pupil-modulating drops, we should pay close attention both to their impact on the ocular surface and on older patients’ night vision. Based on studies of small apertures conducted to date,4 I don’t expect night vision to be a major issue. Nevertheless, I plan to monitor closely patients who use drops that haven’t been tested on older groups. For example, Vuity was evaluated only in phakic patients who were 40 to 55 years old. Of concern is whether night vision problems affect these individuals’ ability to ambulate safely in a dark environment. In contrast, a fixed combination of carbochol and brimonidine tartrate (Brimochol, Visus Therapeutics) and 0.75% phentolamine (Nyxol, Ocuphire) are being studied in pseudophakic patients from different age groups (Table).
Experience with pupil-modulating drops will help us determine the best candidates for treatment and the optimal patterns of use (ie, once daily or more frequently).
CONCLUSION
The goal with any presbyopia-correcting IOL is to satisfy the patient’s visual needs and expectations. Luckily, most times this is achieved. When it is not, however, we have a variety of surgical and pharmacological options in our armamentarium to address patient complaints and turn an unhappy patient into a happy one.
1. Langer J, Shajari M, Kreutzer T, Priglinger S, Mayer WJ, Mackert MJ. Predictability of refractive outcome of a small-aperture intraocular lens in eyes with irregular corneal astigmatism. J Refract Surg. 2021;37(5):312-317.
2. Shajari M, Mackert MJ, Langer J, et al. Safety and efficacy of a small aperture capsular bag-fixated intraocular lens in eyes with severe corneal irregularities. J Cataract Refract Surg. 2020;46:188-192.
3. Abdelkader A, Kaufman HE. Clinical outcomes of combined versus separate carbachol and brimonidine drops in correcting presbyopia. Eye Vis (Lond). 2106;3:31.
4. Ang RE, Picache GCS, Rivera MCR, Lopez LRL, Cruz EM. A comparative evaluation of visual, refractive, and patient-reported outcomes of three extended depth of focus (EDOF) intraocular lenses. Clin Ophthalmol. 2020;14:2339-2351.


