Overview of My Long-Term Experience in Japan
Yoshihiro Kitazawa, MD, PhD
Refractive surgery has a short but rich history that started in the early 1990s. I was among the early adopters, offering PRK first in 1992 and then LASIK in 1996 to my patients as ways to treat their refractive errors. Some of those who were interested in refractive surgery were not, however, suitable candidates for either procedure. In the early 2000s, phakic IOLs were introduced, and I became an early adopter of that technology, too. Over the years, not only has the EVO ICL (STAAR Surgical) become a major part of my practice but I stopped performing LASIK in 2018 in favor of the lens-based procedure.
Clinical trials for the ICL in Japan began in 2003. In 2010 and 2014, the Visian ICL and EVO ICLs were approved, respectively, by the country’s Ministry of Health, Labour and Welfare (MHLW).
REFRACTIVE SURGERY VOLUME BY PROCEDURE
Over the years, the volume of LASIK procedures performed in Japan, where I practice, has decreased and the volume of ICL procedures has increased. This is largely due to two separate events.
No. 1: A report of a mass incidence of postoperative infections experienced by LASIK patients (10.5%) in one center in Japan between July 2008 and January 2009.1 The National Consumer Affairs Center of Japan issued a warning about LASIK, stating that the risk of surgery should not be underestimated and that individuals should be fully briefed on the potential risks associated with the procedure. Additionally, class action lawsuits were brought against two major refractive centers in Japan. Consumer confidence in the procedure declined.
No. 2: Several prominent figures in Japanese pop culture underwent ICL surgery. As this news spread, the general population became more interested in the procedure. People who were interested in undergoing refractive surgery started to recognize the ICL procedure and were researching it online (Figure 1). The procedure has since become a popular refractive option in Japan, exceeding LASIK procedures.
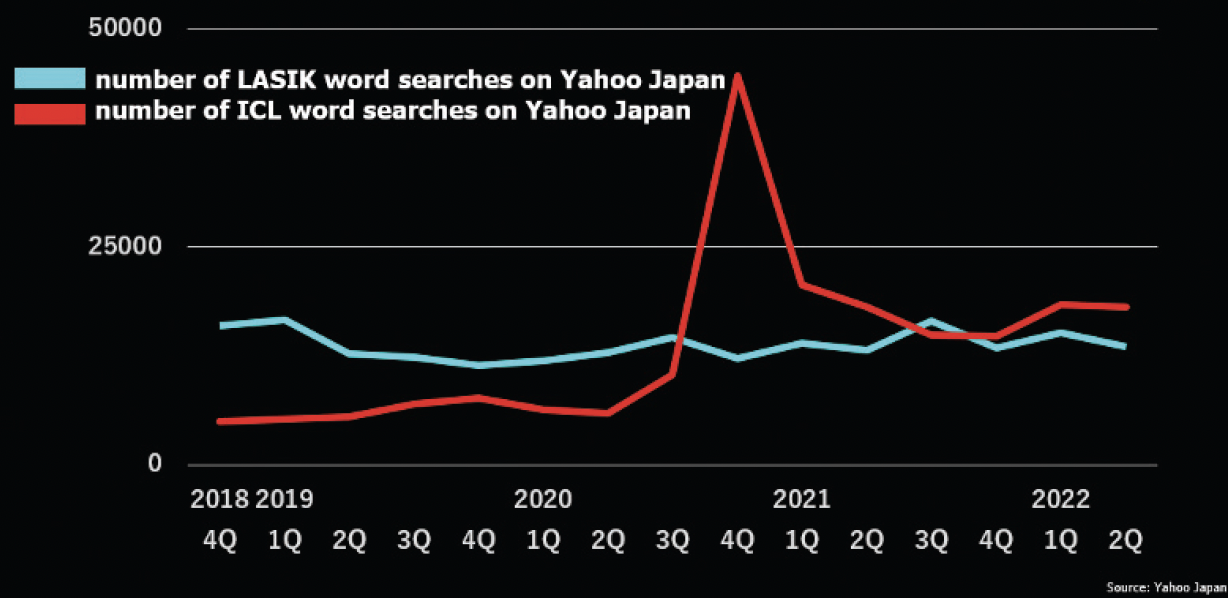
Figure 1. The number of searches for the words LASIK and ICL on Yahoo Japan from 2018 to 2022.
AN ICL-ONLY PRACTICE
I have performed more than 6,500 ICL procedures to date. In February 2019, I opened an ICL-only practice, and procedure volume has climbed steadily (Figure 2). My patient selection criteria for ICL surgery has evolved over time based both on clinical experience and the Japanese Ophthalmological Society’s (JOS) refractive surgery guidelines (for the JOS’s recommendations and the recommendations from a German society, see the sidebars on the following pages). In 2008, the average degree of myopia I treated was -9.36 D; in 2021, it was -6.55 D (Figure 3). I expect that the average degree will continue to decrease.
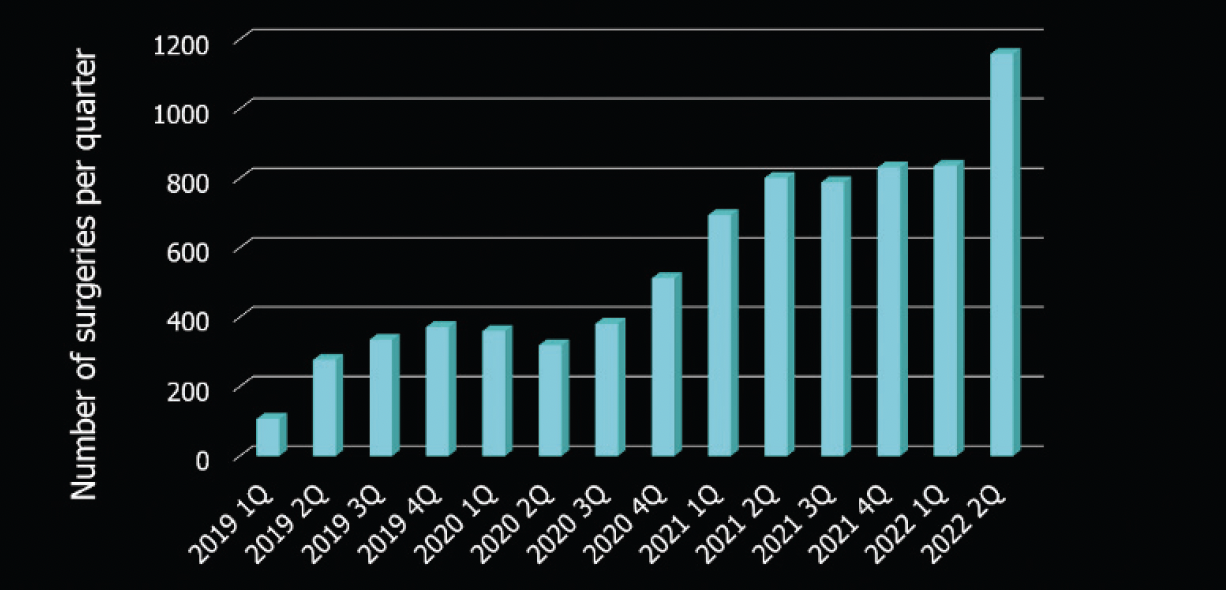
Figure 2. Dr. Kitazawa’s ICL procedure volume per quarter at Sapia Tower Eye Clinic from 2019 to 2022.
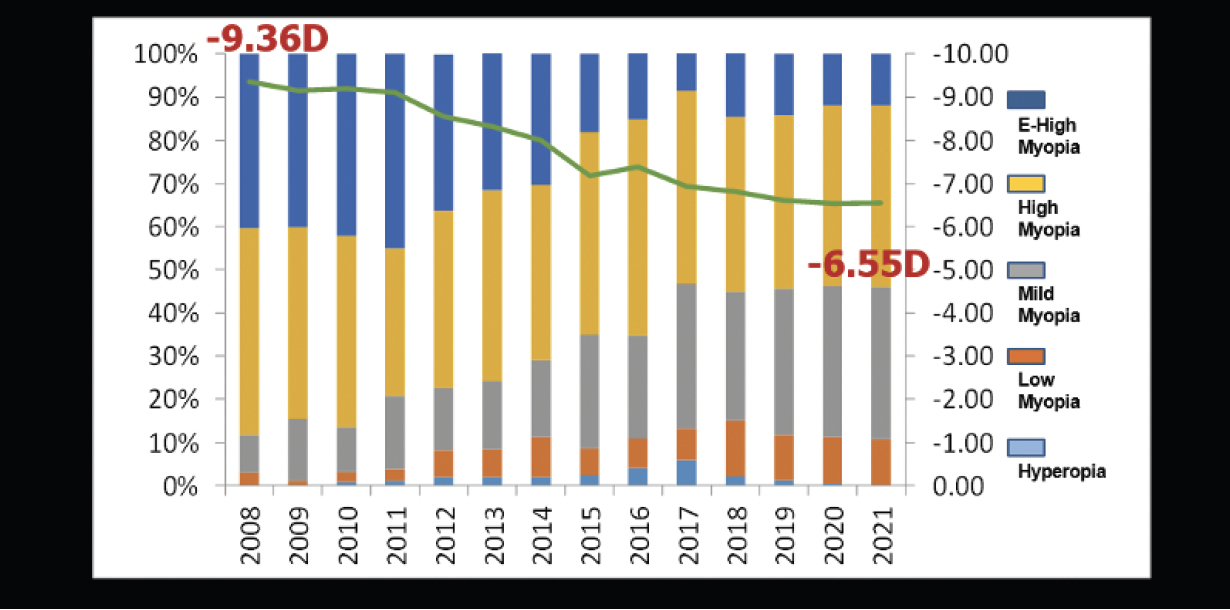
Figure 3. The evolution of the average degree of myopia treatment with the ICL in Dr. Kitazawa’s practice from 2008 to 2021.
In addition to ICL surgery for high myopia, I have extensive experience with the procedure for low to moderate myopia and in 2018 was an investigator for a comparative multicenter study in 351 eyes with low to moderate and high myopia.2 In the study, we found that there were no significant differences in postoperative refraction and visual acuity between the low to moderate myopia and the high myopia groups. The approved power range in Japan for the EVO ICL is from -3.00 to -18.00 D of myopia and 1.00 to 4.50 D of cylinder.
MULTICENTER STUDY RESULTS
My colleagues and I from the Japan ICL Study Group also recently published a retrospective nationwide multicenter study on the 1-year outcomes with the EVO ICL in patients with low myopia.3 These results are detailed here. The study population consisted of 172 eyes of 111 patients with low myopia and myopic astigmatism (manifest spherical equivalent [MSE] -2.26 ±0.57 D, range -0.38 to -3.28 D). The target in all eyes was plano. Safety, efficacy, predictability, stability, and adverse events were evaluated at 1 week and 1, 3, 6, and 12 months.
Uncorrected distance visual acuity at 12 months was excellent, with 99% achieving 20/32 or better, 97% achieving 20/25 or better, 94% achieving 20/20 or better, 88% achieving 20/16 or better, and 73% achieving 20/12.5 (Figure 4). Additionally, 90% experienced no change in corrected distance visual acuity, and no eye lost 2 or more lines of vision. Seven percent gained 1 line, and 1% gained 2 lines (Figure 5). The attempted versus achieved spherical equivalent is found in Figure 6. Predictability and stability of the ICL procedure were also excellent, with 100% and 91% of eyes within ±1.00 and ±0.50 D of intended correction, respectively (Figure 7).
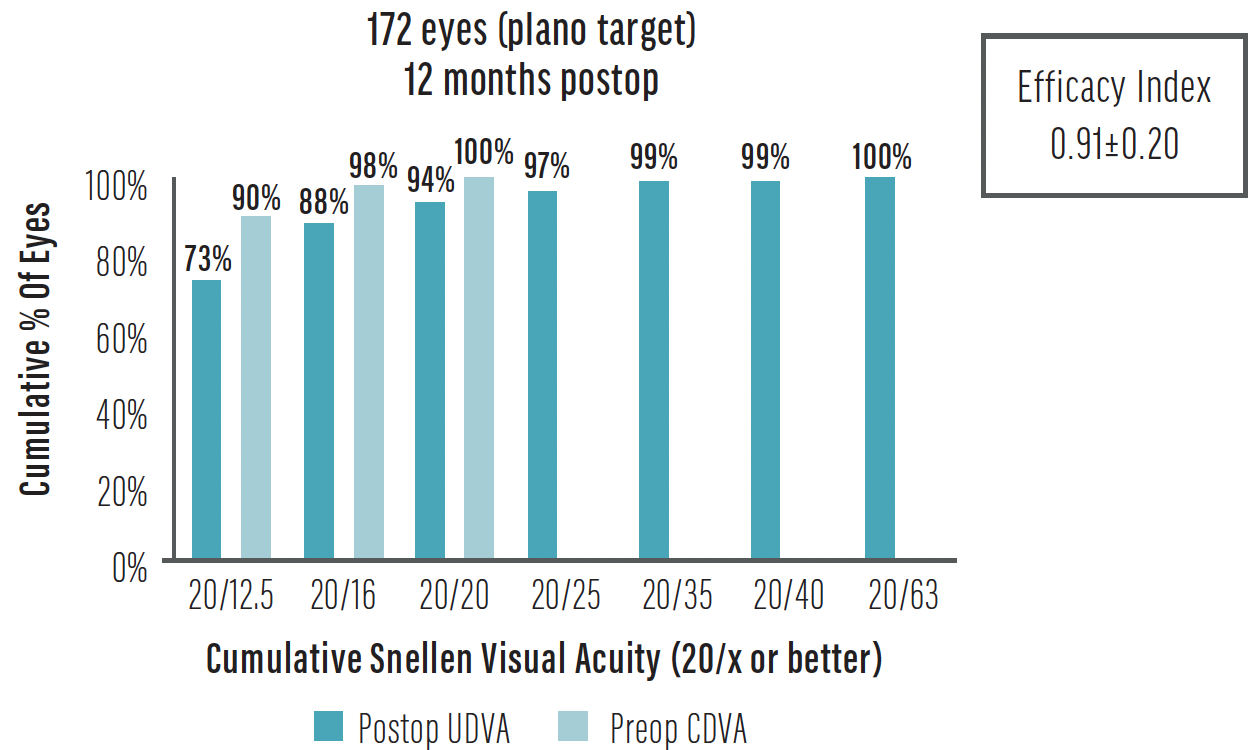
Figure 4. Uncorrected distance visual acuity at 12 months postoperative.3
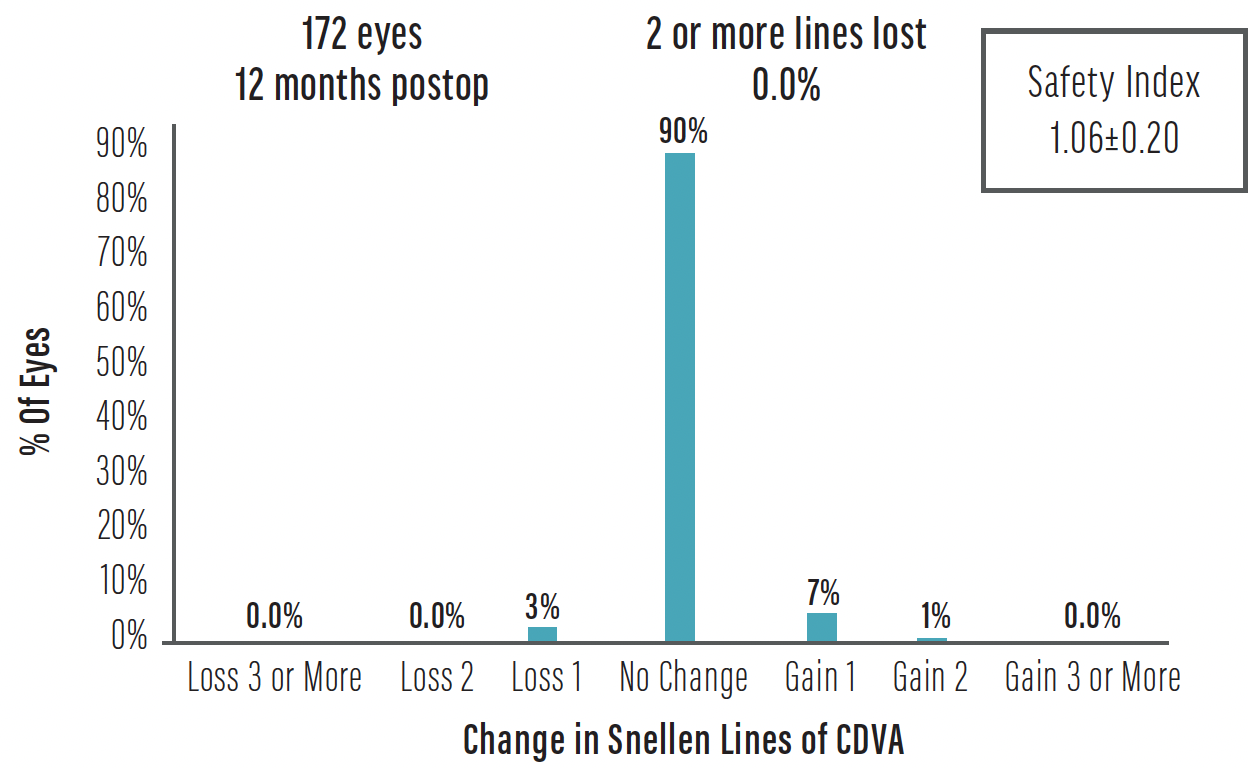
Figure 5. Change in corrected distance visual acuity at 12 months postoperative.3
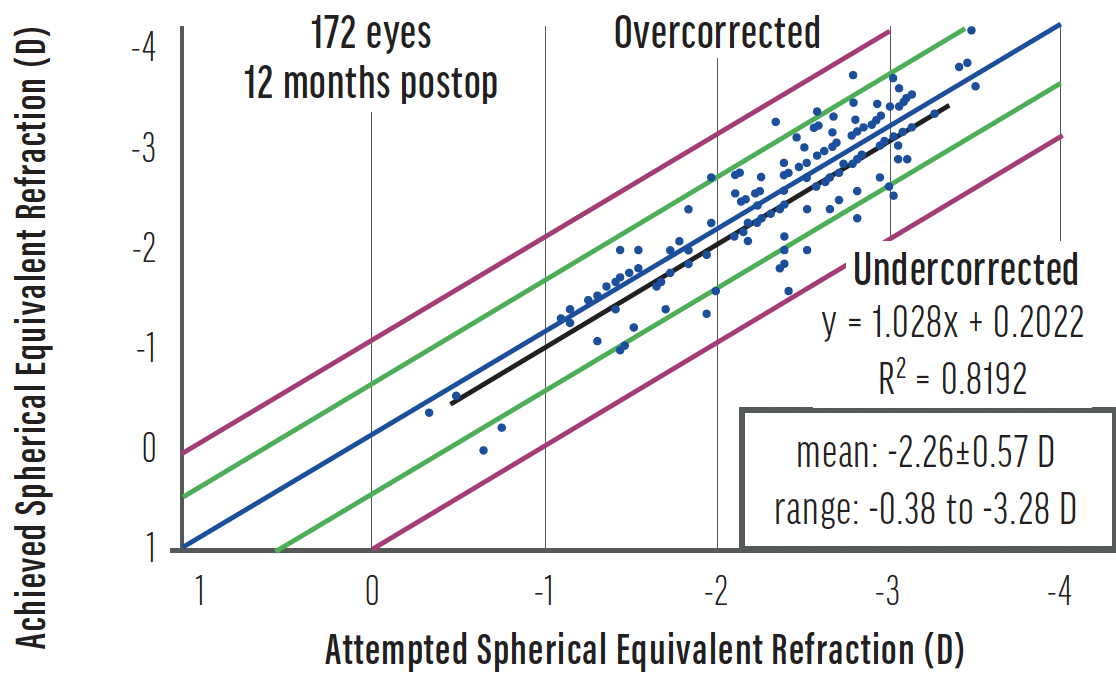
Figure 6. Attempted versus achieved spherical equivalent in 172 eyes at 12 months postoperative.3
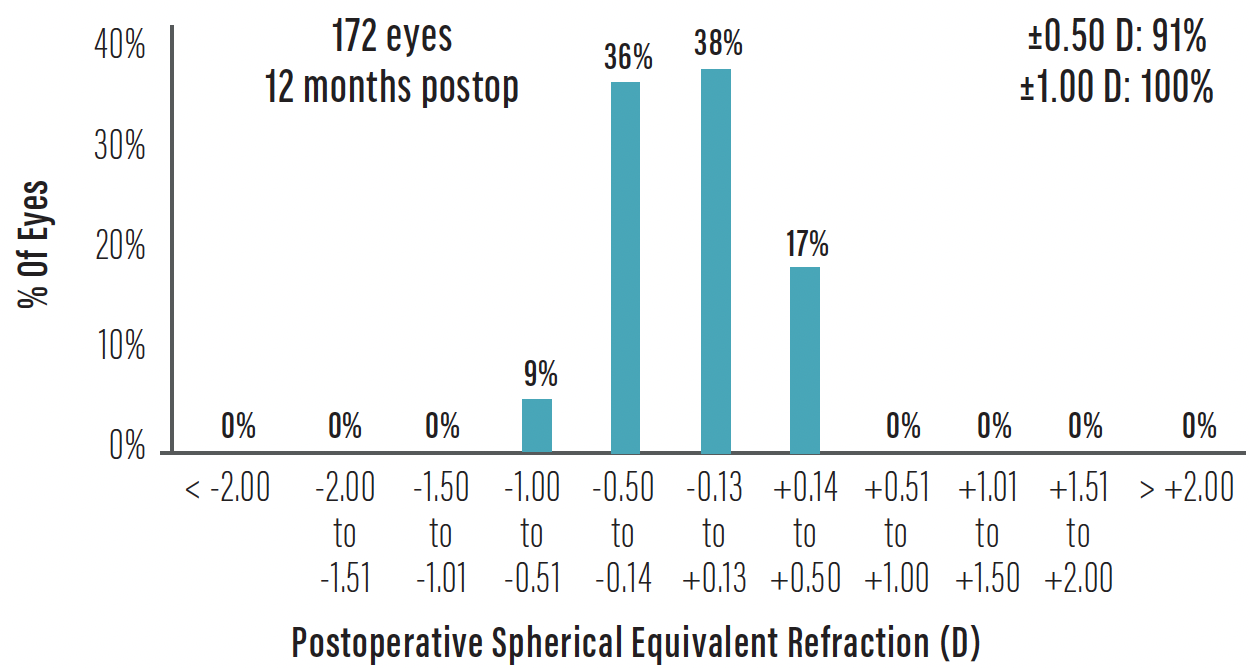
Figure 7. Predictability at 12 months postoperative.3
Stability is shown in Figure 8. Postoperative refraction was stable at -0.14 ±0.28 D at 1 year postoperatively. Additionally, there were no intraoperative complications, and no incidence of removal due to endothelial cell loss, cataract formation, or endophthalmitis. Of the 172 eyes, only four had symptoms of glare and halos. Axis realignment was required in four eyes and an exchange for a new lens power in one.
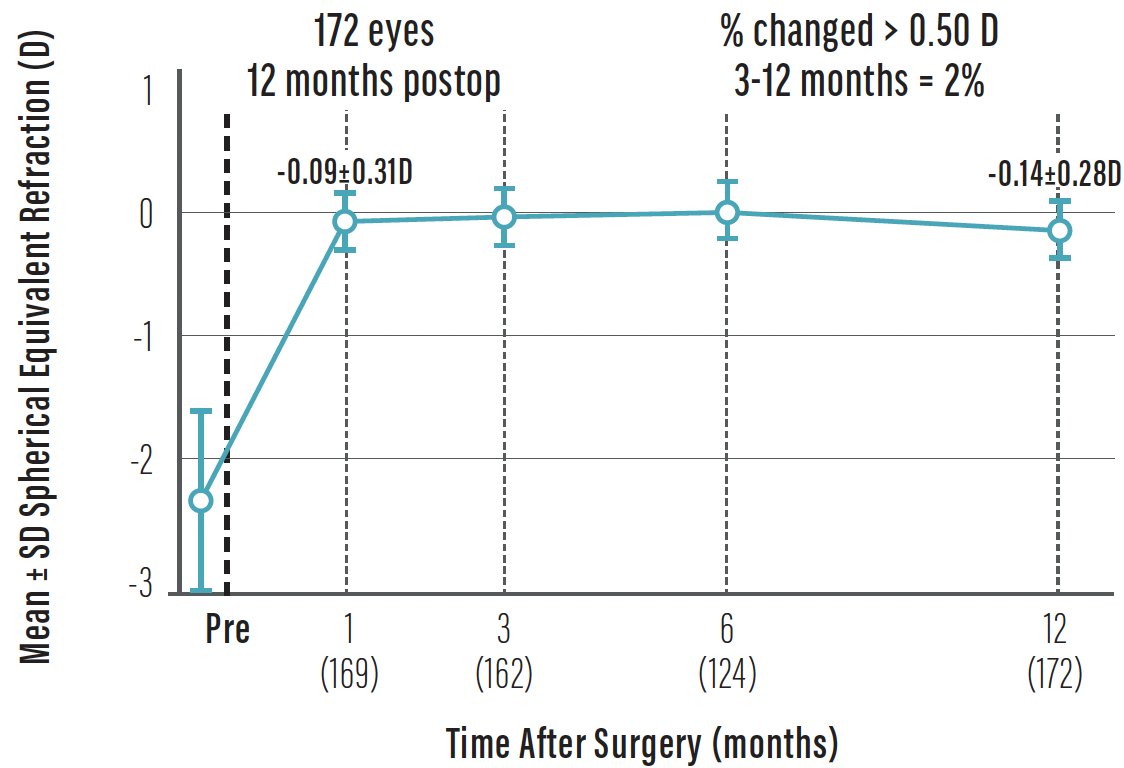
Figure 8. The stability of spherical equivalent refraction in 172 eyes at 12 months postoperative.3
According to our study results, the EVO ICL performed well for the treatment of low myopia without significant complications through the 12-month study period. We therefore support the use of the EVO ICL for correcting low myopia. Additionally, I have performed ICL surgery on patients with low myopia who had decreased visual acuity after LASIK surgery and achieved good UCVA (unpublished data; Figure 9).
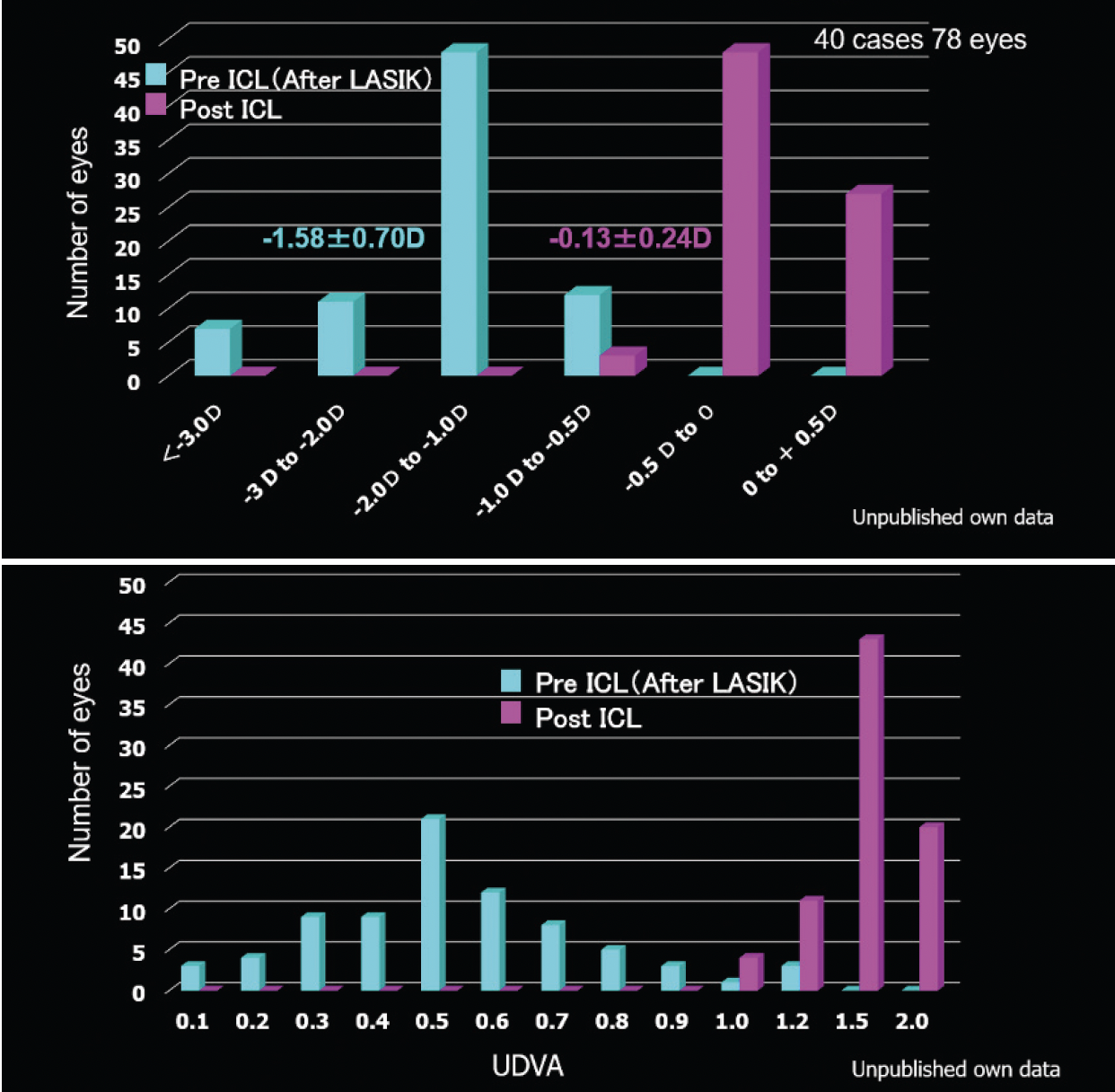
Figure 9. Pre- and postoperative spherical equivalent refraction (top) and uncorrected distance visual acuity (bottom) in 78 eyes of 40 patients treated (unpublished data from Dr. Kitazawa’s clinic).
Japan Ophthalmological Society Recommendations for Phakic IOLs
According to the Japan Ophthalmological Society (JOS), phakic IOLs are recommended for the treatment of moderate myopia of -6.00 D or more.1 For moderate myopia of -3.00 D to less than -6.00 D and for severe myopia of greater than 15.00 D, phakic IOLs can be used with caution. The JOS also recommends that the intended postoperative refraction should not aim for an overcorrection. The organization emphasizes the importance of collecting postoperative results regularly evaluating the safety and surgical efficacy of refractive surgery. The approved power range in Japan for the EVO ICL is from -3.00 to -18.00 D of myopia and 1.00 to 4.50 D of cylinder.
1. Guidelines for refractive surgery (7th edition). Journal of Japanese Ophthalmology Society. 2019;123(2):167-169.
1. Yamaguchi T, Bissen-Miyajima H, Hori-Komai Y, et al. Infectious keratitis outbreak after laser in situ keratomileusis at a single laser center in Japan. J Cataract Refract Surg. 2011;37(5):894-900.
2. Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102:177-181.
3. Kamiya K, Shimizu K, Igarashi A, et al. A nationwide multicenter study on 1-year outcomes of posterior chamber phakic intraocular lens implantation for low myopia. Frontiers in Medicine. 2022;9:762153.
My Experience With EVO in Spain
Ernesto Alonso Juárez, MD
It’s an exciting time to be a refractive surgeon. Approximately 2.3 billion people worldwide with access to eye care require vision correction, and the global demand for refractive surgery is expected to grow at a compound annual rate of 9.6% through 2025.1 The best way to capitalize on the potential growth is to offer a variety of procedures including laser vision correction, phakic IOL implantation, presbyopia correction, and refractive lens exchange. Of these, the EVO ICL is my preferred treatment. Now, there is growing evidence that the procedure is an excellent option for patients with low myopia.2
PERSONAL EXPERIENCE
At Clinic INSADOF, we started performing ICL surgery in 2002. From that time to 2020, our ICL volume grew from 0% to 85% of refractive surgery procedures performed in patients who are up to 45 years of age. At first, we positioned the procedure as an alternative for those who were not suitable candidates for laser vision correction, and we only used the procedure for eyes with thin corneas or the treatment of -7.00 D of myopia or greater. After excellent results and high patient satisfaction, we expanded our patient selection progressively to include a wider diopter range. We started with expanding to moderate myopia and eventually to low myopia.
Today, any patient who is a suitable candidate for refractive surgery—regardless of the refractive power—is informed of the advantages and disadvantages of all options, including LASIK, PRK, and ICL surgery.
CLINICAL STUDY
We performed a study at Clinic INSADOF and Clinic Villoria, both in Spain, from 2016 to 2020 to determine the safety and efficacy of ICL surgery for the treatment of low myopia or myopic astigmatism (-3.50 D or lower). All patients (N = 82) were candidates for both ICL and corneal laser surgery, selected the procedure after learning about the pros and cons versus corneal laser surgery, and completed at least 12 months of follow-up after ICL implantation. One eye per patient was treated, and all eyes had an anterior chamber depth of at least 2.8 mm, measured from the endothelium. The average sphere and spherical equivalent were -1.94 ±0.84 and -2.34 ±0.82 D, respectively. The mean ICL spherical power was -3.04 ±0.79 D, and approximately 38% of patients received a toric EVO ICL. The results of our study, published in 2022, are summarized here.3
The mean uncorrected and corrected distance visual acuity at 1 month postoperative were 1.09 ±0.18 and 1.09 ±0.14, respectively, and the mean sphere and cylinder were -0.01 ±0.14 and -0.05 ±0.15, respectively. The vault was also good at 573 ±240 µm. There was no incidence of lens removal, exchange, or modification. The efficacy and safety indices were 1.07 ±0.17 and 1.09 ±0.17, respectively.
The results were stable over time. At 12 months postoperative, the mean uncorrected and corrected distance visual acuity were 1.07 ±0.14 and 1.09 ±0.13, respectively. The mean changes from preoperative to 12 months postoperative for uncorrected and corrected distance visual acuity were 0.87 ±0.23 and 0.07 ±0.22, respectively (Figure 10). Additionally, the mean sphere and cylinder were -0.02 ±0.12 and -0.02 ±0.18, respectively. The vault was 513.78 ±262.87 µm. The efficacy and safety indices were 1.07 ±0.15 and 1.09 ±0.13, respectively. The refractive precision for sphere and cylinder is shown in Figure 11, and the refractive stability is shown in Figure 12. Both analyses support that the EVO ICL is safe, effective, and stable for the correction of low myopia.
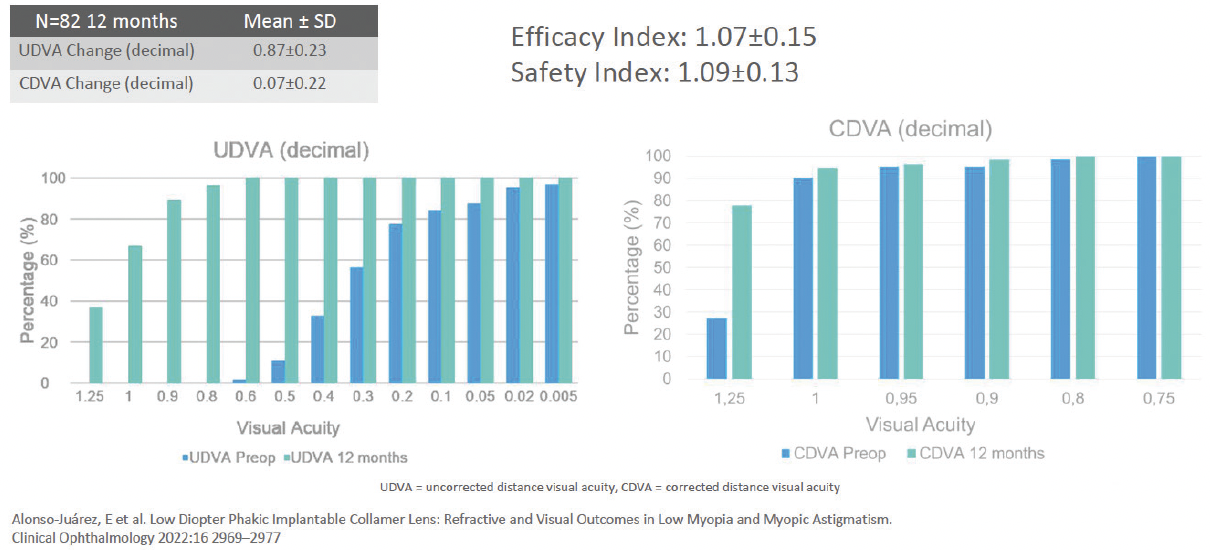
Figure 10. Changes in uncorrected and corrected distance visual acuity at 12 months postoperative.
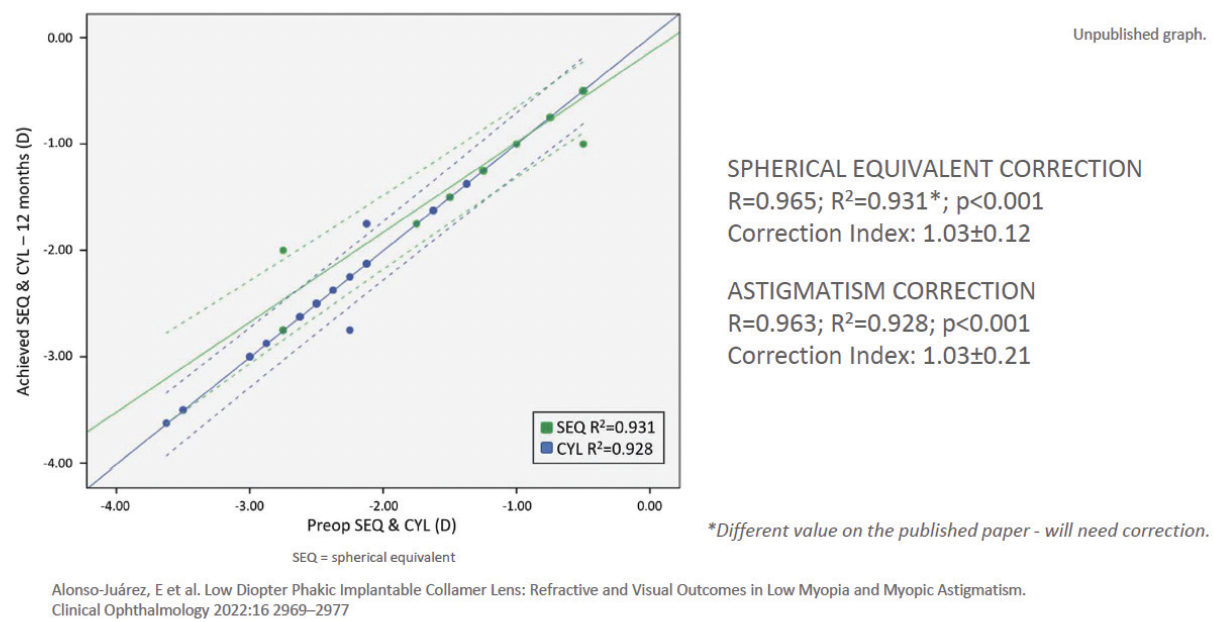
Figure 11. The refractive precision at 12 months postoperative for both sphere and cylinder.
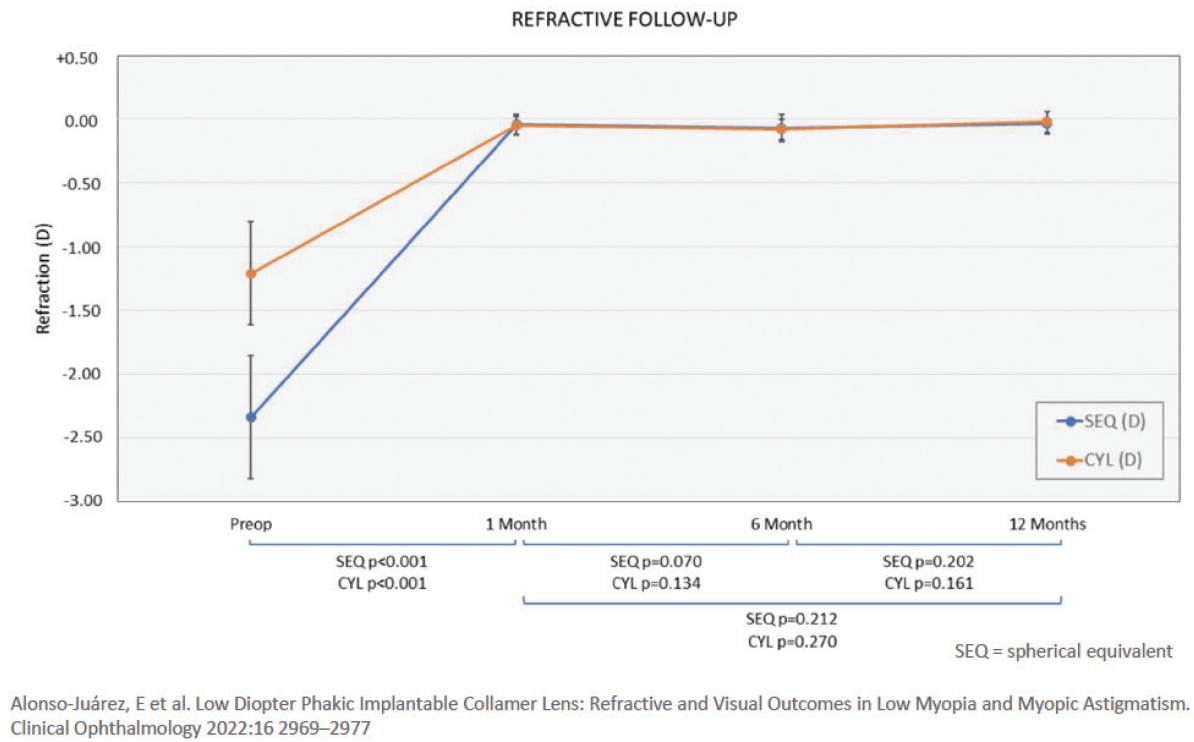
Figure 12. The refractive stability at 12 months postoperative.
DISCUSSION
Other published studies have also shown that the EVO ICL is a good option for low myopia. One study that compared postoperative results between patients with low (mean spherical equivalent -4.89 D) and moderate to high myopia (mean spherical equivalent >-6.00 D) found efficacy and safety indices of 1.05 ±0.17 and 1.13 ±0.18, respectively, in the low myopia group.4 For comparison, the efficacy and safety indices of other refractive surgery procedures are reported to be 0.95 ±0.14 and 0.96 ±0.13, respectively, for transepithelial PRK and 0.98 ±0.12 and 0.99 ±0.12, respectively, for LASIK.5 Another study found a mean vault reduction of -41 ±64 µm from 6 to 12 months postoperative and remained stable at 12 months.6 In our study, the mean reduction in central vault was 28.66 µm from 1 month to 6 months.
Commission on Refractive Surgery Recommendations for Phakic IOLs in Germany
In June 2022, the German Commission on Refractive Surgery (KRC), a joint commission of the German Ophthalmological Society and the Professional Association of Ophthalmologists of Germany, updated its recommendations for the quality assurance of refractive surgery procedures, including phakic IOL surgery.1 The following recommendations are for the EVO ICL (STAAR Surgical) and Artisan/Artiflex IOLs (Ophtec).
Phakic IOLs are indicated for the correction of myopia and myopic astigmatism from -1.00 D and hyperopia and hyperopic astigmatism from 1.00 D in individuals aged 18 years and older. A laser procedure or toric phakic IOL implantation can be performed for the treatment of concomitant astigmatism or residual ametropia after phakic IOL implantation. The KRC does not recommend same-day bilateral implantation of phakic IOLs, and it requires follow-up examinations for corneal endothelial cell density at least annually. In Germany, the procedure is contraindicated in patients with glaucoma and marked visual field damage; those with preexisting corneal damage and severely reduced endothelial cell counts and endothelial cell density below 2,000/mm2; and in eyes with inadequate anterior chamber depth (below 2.8 mm for myopia or 3.0 mm for hyperopia measured from the endothelium). *See the Important Safety Information below for complete details about the approved range.
1. Refractive Surgery Commission – KRC. Assessment and quality assurance (KRC recommendations). June 2022. Accessed April 24, 2023. Deutsch Ophthalmologische Gesellschaft. http://bva.dog/krc/?seite=empfehlungen
CONCLUSION
The EVO ICL and toric EVO ICL are valid options for the correction of low myopia. They preserve the cornea, have a proven long-term safety profile,7-9 and induce low higher-order aberrations on the cornea.10 Additionally, other studies confirm our results showing that the procedure is predictable, effective, safe, and stable with high efficacy and safety indices over time.2
1. Market Scope: Refractive surgery to grow 9.6% a year through 2025, despite COVID-19. January 19, 2021. Accessed March 3, 2022. https://eyewire.news/articles/market-scope-refractive-surgery-to-grow-9-6-a-year-through-2025-despite-covid-19/?c4src=article:infinite-scroll
2. Packer M. The Implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427-38.
3. Alonso-Juárez E, et al. Low diopter phakic implantable collamer lens: refractive and visual outcomes in low myopia and myopic astigmatism. Clin Ophthalmol. 2022;16:2969-2977.
4. Pinto C, Monteiro T, Franqueira N, Faria-Correia F, Mendes J, Vaz F. Posterior chamber collamer phakic intraocular lens implantation: Comparison of efficacy and safety for low and moderate-to-high myopia. Eur J Ophthalmol. 2022;32(2):894-901.
5. Gershoni A, Reitblat O, Mimouni M, Livny E, Nahum Y, Bahar I. Femtosecond laser assisted in situ keratomileusis (FS-LASIK) yields better results than transepithelial photorefractive keratectomy (Trans-PRK) for correction of low to moderate grade myopia. Eur J Ophthalmol. 2020; dec 14 AoP.
6. Alfonso JF, Fernández-Vega L, Lisa C, et al. Long-term evaluation of the central vault after phakic Collamer lens (ICL) implantation using OCT. Graefe’s Arch Clin Exp Ophthalmol. 2012;250(12):1807-1812.
7. Kohnen T. Phakic intraocular lenses: where are we now? J Cataract Refract Surg. 2018;44(2):121-123.
8. Papa-Vettorazzi M, et al. Long term efficacy and safety profiles following posterior chamber phakic intraocular lens implantation in eyes with a 10-year follow-up. J Cataract Refract Surg. 2022;48:813-818.
9. Packer M. Evaluation of the EVO/EVO+ sphere and toric Visian ICL: six month results from the United States Food and Drug Administration clinical trial. Clin Ophthalmol. 2022;16:1541-1553.
10. Igarashi A. Posterior chamber phakic IOLs vs. LASIK: benefits and complications. Exp Rev Ophthalmol. 2019;14(1):43-52.
Important Safety Information for the Phakic ICL Family
The EVO/EVO+ ICL is indicated for phakic patients 21-60 years of age to correct/reduce myopia up to -20.0 D with up to 6.0 D of astigmatism, the EVO Viva ICL is indicated for phakic patients 21-60 years of age to correct/reduce myopia up to -20.0 D with or without presbyopia, and the Visian ICL is indicated for phakic patients 21- 45 years of age, to correct/reduce hyperopia up to +16.0 D with up to 6.0 D of astigmatism. Careful preoperative evaluation and sound clinical judgment should be used by the surgeon to decide the risk/ benefit ratio before implanting a lens in a patient with any of the conditions described in the DFU. Prior to surgery, physicians should inform prospective patients of possible risks and benefits associated with the EVO/EVO+ ICL, EVO Viva ICL or Visian ICL.
ATTENTION: Reference the EVO/EVO+ ICL, EVO Viva ICL, and Visian ICL DFUs available at https://edfu.staar.com/edfu/ for a complete listing of indications, contraindications, warnings and precautions.