
Digitization in health care is vitally important because of the number of patients we treat and the amount of information needed to successfully manage even the simplest of cases. In the past 10 years, the digital era has redefined cataract surgery and astigmatism correction because it allows us to analyze the huge amounts of data needed to obtain the best refractive outcomes.
When using toric IOLs, surgeons must adapt their routines and surgical techniques. Calculating the correct IOL power and accurately marking the axis are the most important steps, directly responsible for the final refractive result.
In the classic technique, marking of the steep axis is performed manually, a time-consuming process that is subject to human error.1 Ink can fade, spread, or even entirely disappear. Surgeons can now benefit from interconnected digital devices that offer a multimodal approach, boosting efficiency, precision, and accuracy so that cataract surgeons can deliver optimal outcomes, and at the same time gathering and processing information from all stages of cataract case management.
PATIENT SELECTION FOR TORIC IOLS
Spectacle independence has become more important for today’s patients, and emmetropia after cataract surgery has become the gold standard. Using a toric IOL to correct corneal astigmatism offers economic benefits as well as desirable aesthetics and practical advantages for patients. Toric IOLs are typically considered premium IOLs, but ideally they should be regarded as standard IOLs.
If we consider the minimum corneal astigmatism for toric IOL implantation to be 0.75 D, then more than 40% of patients can benefit from toric IOL correction.2 These patients are at risk to experience blurred uncorrected distance visual acuity after surgery due to residual astigmatism. To resolve this would require additional surgery, spectacles, or contact lenses if corneal astigmatism is not correctly managed from the outset.
Selection criteria for toric IOLs include a calculated postoperative residual astigmatism greater than 0.75 D cylinder, regular bow-tie astigmatism, no preexisting ocular pathologies that can negatively influence toric IOL efficacy (corneal dystrophy, keratoconus, pellucid marginal degeneration, corneal scar tissue), and no capsular bag instability issues (advanced pseudoexfoliation syndrome or trauma that can induce zonulolysis).
CALCULATING TORIC IOL POWER
Despite the availability of several ways to calculate toric IOL power that are designed to be as accurate as possible, the final refractive result can sometimes still be a surprise. This is why it is recommended to use at least two methods to determine corneal astigmatism, such as keratometric readings, corneal topography, and tomography.
Surgeons must take into consideration several factors:
- Total corneal astigmatism (keratometric and posterior astigmatism);
- Central astigmatism;
- Surgically induced astigmatism (SIA); and
- Effective lens position.3,4
All toric IOL manufacturers have user-friendly, web-based toric calculators, and it is advised to have a printout of the axis calculator results in the OR. Additionally there are many toric calculation formulae available to determine the right IOL power.
Toric IOL efficacy decreases with the increase of axis misalignment. Clinical effects can include decreased toric correction,5,6 hyperopic spherical shift, and change of axis orientation.
INTRAOPERATIVE TECHNOLOGY FOR ALIGNMENT
Several digital technologies can be used to help exclude human error and provide a higher degree of assurance in intraoperative toric IOL alignment. Interconnected devices can measure IOL power, process data, and share information to the surgical microscope.1 These technologies include real-time eye-tracking technology that compensates for cyclorotation and eye movements to ensure that the superimposed visual templates always remain in the same position in relation to the eye.
The chance to intraoperatively combine systems to increase precision exists, but attention must be paid when matching limbal registration with iris fingerprinting because, for example, femtosecond laser systems tend to alter the conjunctival vascular architecture. Also, the type of anesthesia can influence the recognition, especially if the globe is tilted or conjunctival chemosis limits visualization of the vessels.
There are three main principles used by these technologies:
- Limbal registration (image-guided): An image of the vascularization of the conjunctiva and sclera is captured during biometry and matched with the image obtained by the surgical microscope. An overlay then indicates the steepest axis (Figure 1). The intended axis can be automatically selected from preoperative biometry data or manually entered depending on the IOL calculation formula used.
- Intraoperative wavefront aberrometry: This technology offers the possibility to intraoperatively determine real-time analysis of refraction, astigmatism, and aphakic lens power. The surgeon can instantly adjust the toric IOL to the suggested position based on the data provided.
- Iris fingerprinting (iris detection): Combining this technology with corneal shape analysis ensures marking of the steep corneal axis by the femtosecond laser in a way that compensates for cyclorotation. It appears to be that using these types of marks can offer better correction of corneal astigmatism during cataract surgery (Figure 2).
The markings can be classified into two categories:
- Virtual markings that are visible only as projections during surgery, making it difficult to monitor postoperative misalignment (image-guided systems or intraoperative wavefront aberrometry); and
- Real semipermanent or permanent markings (intrastromal corneal or capsular markings; Figure 3).
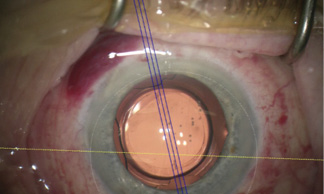
Figure 1. The Z Align function with the Callisto Eye (Carl Zeiss Meditec) allows markerless toric IOL alignment.
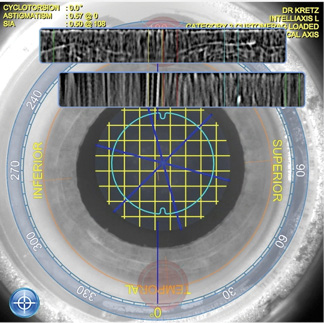
Figure 2. Intelli Axis-L of the Streamline IV software in the Lensar laser system (Lensar) for iris fingerprint detection. Reference image taken with the Pentacam HD (Oculus).
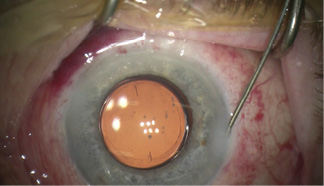
Figure 3. Toric IOL alignment using Lensar capsular markings.
Lensar Streamline IV:
An Intelligent Way to Address Corneal Astigmatism During Cataract Surgery
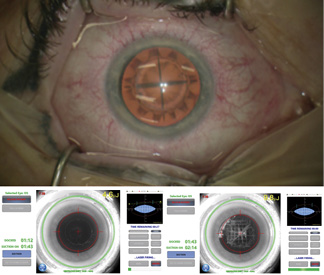
Figure. Capsulotomy and cataract segmentation as performed by the Lensar Femtosecond Laser System.
1. Kretz TA. Comparison of different automated approaches for toric IOL alignment: femtosecond laser-assisted capsular markings vs digital visual guidance system. Paper presented at: ESCRS Annual Meeting; September 21-26, 2018; Vienna, Austria.
ADVANTAGES OF USING A DIGITAL SYSTEM
The advantages of using a digital system when implanting toric IOLs are many:
- Improved efficiency and refractive outcomes: Preoperative and intraoperative marking is not required, improving workflow and OR efficiency;
- Reduced time per case;
- Lower risk of human error, as automation eliminates transcription errors;
- Increased profit via the ability to treat more patients per day;
- Increased patient and surgeon satisfaction; and
- Photographic and video documentation of surgery and toric IOL alignment.
TIPS AND TRICKS
For perfect keratometry (K) readings, we must ensure that the patient’s head is perfectly positioned in order to avoid using a false horizontal axis. The patient’s eyelids must be wide open, and the light in the room must not be too bright, to prevent reflections on the sclera. During K readings, the curvature of the cornea is not directly measured, but rather a reflection from the tear film; therefore, it is recommended to do the K reading on an intact corneal tear film, before pupil dilation or topical anesthesia drops are applied, which can degrade the tear film. In severe dry eye cases, preoperative treatment is recommended to ensure good tear film stability during measurement.
When limbal registration is employed, several factors can alter the conjunctival vascular architecture, including pharmacologic mydriasis, increased blood flow, use of balanced salt solution, application of topical anesthesia, conjunctival chemosis, or subconjunctival hemorrhages. Head position in relation to the preoperative image can also influence digital guidance systems.
When intraoperative wavefront aberrometry is used, external factors can negatively influence the intraoperative measurements, including the eyelid speculum, dry eye, IOP, and corneal hydration.7-9 For precise aphakic power calculation, it is advised to use an OVD or balanced salt solution to moisten the cornea, maintain an IOP of 20 to 30 mm Hg, ensure that there are no air bubbles in the visual pathway, and avoid excessive wound hydration.
CONCLUSION
We believe that the future of cataract surgery is digital and that these technologies offer many advantages for surgeons and patients. Digitization allows rapid, precise, automatic transfer of information and incorporates it all into high-tech, modern equipment.
A surgeon’s hands are acknowledged for their remarkable performance in the most complex of cataract surgery cases. Still, those hands, no matter how skillful, are only as accurate as what the surgeon’s eyes can see. This is why the benefits of digital technologies are to be embraced. n
1. Mayer WJ, Kreutzer T, Dirisamer M, et al. Comparison of visual outcomes, alignment accuracy, and surgical time between 2 methods of corneal marking for toric intraocular lens implantation. J Cataract Refract Surg. 2017;43(10):1281-1286.
2. Ferrer-Blasco T, Montes-Mico R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35(1):70-75.
3. Savini G, Versaci F, Vestri G, et al. Influence of posterior corneal astigmatism on total corneal astigmatism in eyes with moderate to high astigmatism. J Cataract Refract Surg. 2014;40(10):1645-1653.
4. Savini G, Hoffer KJ, Carbonelli M, et al. Influence of axial length and corneal power on the astigmatic power of toric intraocular lenses. J Cataract Refract Surg. 2013;39(12):1900-1903.
5. Langenbucher A, Viestenz A, Szentmary N, et al. Toric intraocular lenses–theory, matrix calculations, and clinical practice. J Refract Surg. 2009;25(7):611-622.
6. Langenbucher A, Viestenz A, Seitz B. Toric intraocular lenses for compensation of corneal astigmatism. Klin Monbl Augenheilkd. 2004;221(3):182-190.
7. Thulasi P, Khandelwal SS, Randleman JB. Intraocular lens alignment methods. Curr Opin Ophthalmol. 2016;27(1):65-75.
8. Dick HB, Schultz T. Laser-assisted marking for toric intraocular lens alignment. J Cataract Refract Surg. 2016;42(1):7-10.
9. Ventura BV, Wang L, Weikert MP, et al. Surgical management of astigmatism with toric intraocular lenses. Arq Bras Oftalmol. 2014;77(2):125-131.


