
The glaucoma surgical landscape has evolved substantially in the past decade. As early as the 1990s, primary surgical treatments for glaucoma were evaluated in clinical trials, including the Moorfields Primary Therapy Trial (MPTT)1 and the Collaborative Initial Glaucoma Treatment Study (CIGTS).2 In the former study, patients (N = 168) were randomly assigned to receive one of three treatments—laser, surgery, or medication—and were followed for a minimum of 5 years. Better visual field outcomes were found in the laser and surgery groups compared to the medication group. In the latter study, primary trabeculectomy versus medicine were overall similar in terms of visual fields, but there was less optic disc progression in the primary surgery group and less visual field progression for more moderate to advanced patients. The results of this and other studies underscore the importance of surgical intervention for elevated IOP. Historically, however, the timing of surgery is often reserved for later stages of disease progression.
As practicing ophthalmologists, we can sometimes have trouble getting around the standard indications for glaucoma surgery. We're programmed to proceed to surgery when the IOP is elevated and the patient is on the maximally tolerated medical therapy and has advanced disease. We're taught in medical school, residency, and fellowship to follow this dictum, and our colleagues reinforce this school of thought at meetings. We do glaucoma surgery when the disease is advanced and medical therapy is no longer effective.
But what about cataract surgery? No surgeon waits to perform phacoemulsification until the patient’s cataract is white or the disease has progressed so far that the patient’s visual acuity is count fingers. Rather, they perform cataract surgery much earlier in the disease state now to achieve optimal outcomes for their patients and, in the process, decrease the risk of intraoperative complications. The same is true with corneal surgery. No one waits to perform corneal surgery until an invasive procedure such as penetrating keratoplasty is required. Today, it is more likely that these patients will undergo less-invasive procedures such as Descemet membrane endothelial keratoplasty and Descemet stripping endothelial keratoplasty while their vision is still 20/25 or 20/30 with glare due to significant Fuchs dystrophy. Why is it not the same for glaucoma surgery?
EMBRACING THE PARADIGM SHIFT
In the past, the benefits of early glaucoma surgical intervention were insufficient and the significant risks too great to justify the early use of traditional procedures such as trabeculectomy or tube shunts. The emergence of MIGS procedures, however, has potentially tipped the risk-benefit scale in favor of early surgery to afford quality of life benefits to patients who otherwise would not be considered appropriate surgical candidates. Furthermore, decreased IOP fluctuation and the likelihood of improved adherence may reduce the risk of visual field progression and/or need to progress to further, more invasive surgery.3 This is a paradigm shift that I am hopeful more surgeons will continue to consider. (See The Risk-Benefit Scale of Early Glaucoma Surgical Intervention.)
MIGS procedures combined with cataract surgery create a pathway for early surgical intervention for glaucoma. It also creates the opportunity to intervene without adding significant risk to the patient. Conversely, MIGS as a standalone procedure is a more deterministic decision. In other words, modest efficacy may justify performing MIGS at the time of cataract surgery, but it might not justify using MIGS as a standalone procedure. The MIGS approach should therefore be selected carefully depending on the surgical goals. For a standalone procedure, the chosen MIGS approach should maximize the potential for effectiveness without sacrificing a favorable safety profile.
ENTER THE OMNI SURGICAL SYSTEM
The OMNI Surgical System (Sight Sciences) is an innovative MIGS device that is indicated for both a standalone procedure and in combination with cataract surgery. This technology combines three mechanisms to alleviate resistance in the conventional outflow pathway: ab-interno canaloplasty, distal outflow dilation, and trabeculotomy.
The OMNI is unique because it addresses both proximal (trabeculotomy) and distal (canaloplasty) resistance with a single, implant-free device. Both procedures are performed sequentially, enabling the surgeon to treat 360º of Schlemm’s canal and address all three sources of outflow resistance (trabecular meshwork, Schlemm’s canal, and collector channels) in a single surgery.
SUBSTANTIATING THE BENEFITS OF A STANDALONE APPROACH
A recent study by Vold et al evaluated the effectiveness of OMNI when used as a standalone procedure in pseudophakic eyes.4 The primary effectiveness of the procedure was defined as the proportion of patients who achieved a 20% reduction in IOP from the preoperative baseline or an IOP between 6 and 18 mm Hg (inclusive) at month 12 while on the same or fewer ocular hypotensive medications as baseline and without the need for a secondary surgical intervention for IOP control. Most patients (72.9%) met the success criteria (Figure).
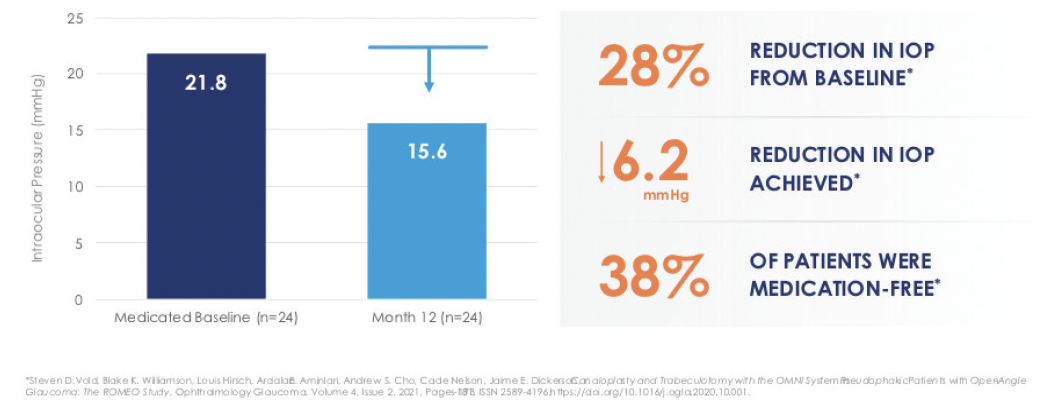
Figure. Demonstrated IOP reduction in pseudophakic patients enrolled in the ROMEO study.
In a subgroup analysis of patients with a baseline IOP of greater than 22 mm Hg, a mean reduction of 8.8 mm Hg was observed. Adverse events were typical for the patient population that undergoes angle surgery and included mild inflammation (13%), IOP spikes (6%), hyphema (4%), corneal edema (4%), and BCVA loss (4%).
A study by Klabe et al showed similar outcomes.5 A total of 38 eyes of 27 patients with mild to moderate open-angle glaucoma that was medically uncontrolled received the OMNI in a standalone procedure. At 24 months postoperatively, IOP was reduced by 10.0 mm Hg from a preoperative baseline of 24.6 mm Hg. Patients were on an average of 1.9 medications. Additionally, all eyes achieved a 20% or greater reduction in IOP at 24 months.
Studies that will provide longer-term data to confirm the duration of effectiveness and the long-term safety of OMNI as a standalone procedure are currently underway. Head-to-head comparative effectiveness studies versus other MIGS technologies and ocular hypotensive drops will also help shape the evolution of glaucoma treatment in years to come.
CONCLUSION
The benefits of early surgical intervention for glaucoma are becoming more apparent. The biggest advantages include addressing adherence issues with medical therapy with better disease control, the avoidance of medication-related side effects, and potential improved quality of life.
Having an effective and safe standalone glaucoma intervention such as OMNI is valuable to the growing population of pseudophakic and phakic patients with glaucoma.
1. Migdal C, Gregory W, Hitchings R. Long-term functional outcome after early surgery compared with laser and medicine in open-angle glaucoma. Ophthalmology. 1994;101(10):1651-1656.
2. Feiner L, Piltz-Seymour JR, Collaborative Initial Glaucoma Treatment Study. Collaborative Initial Glaucoma Treatment Study: a summary of results to date. Curr Opin Ophthalmol. 2003;14(20:106-111.
3. Pyfer MF, Gallardo M, Campbell A, et al. Suppression of diurnal (9AM-4PM) IOP fluctuations with minimally invasive glaucoma surgery: an analysis of data from the prospective, multicenter, single-arm GEMINI study. Clin Ophthalmol. 2021;15:3931-3938.
4. Vold SD, Williamson BK, Hirsch L, et al. Canaloplasty and trabeculotomy with the OMNI system in pseudophakic patients with open-angle glaucoma: the ROMEO study. Ophthalmology Glaucoma. 2021;4:173-181.
5. Klabe K, Kaymak H. Standalone trabeculotomy and viscodilation of Schlemm’s canal and collector channels in open-angle glaucoma using the OMNI Surgical System: 24-month outcomes. Clinical Ophthalmology. 2021;15:3121-3129.



