Cataract surgery is one of the safest surgical procedures in the world. The procedure is not, however, without risks, such as posterior capsular opacification (PCO). PCO occurs in 20% to 40% of patients within 2 to 5 years after cataract surgery1 and can result in decreased visual acuity and visual function. It is generally treated with an Nd:YAG laser capsulotomy, but there is considerable variation in how the posterior laser capsulotomy is performed in clinical practice.2 I have developed guidelines to help surgeons overcome the final hurdle to premium visual outcomes and restore patients’ baseline BCVA after PCO has occurred.
BACKGROUND
The ideal opening for a posterior capsulotomy is between 5 and 6 mm. Additionally, it should be free of lens epithelia to obtain an optimal view of the retinal periphery (Figure 1). Many surgeons prefer a circular YAG posterior capsulotomy to avoid lens pitting in the IOL center (Figure 2). This results, however, in a large free-floating capsule lobe, which for many patients can be a distressing iatrogenic floater. The cruciate pattern is also commonly performed because it allows the capsule flaps to retract out of the visual axis with less incidence of a free-floating capsule.
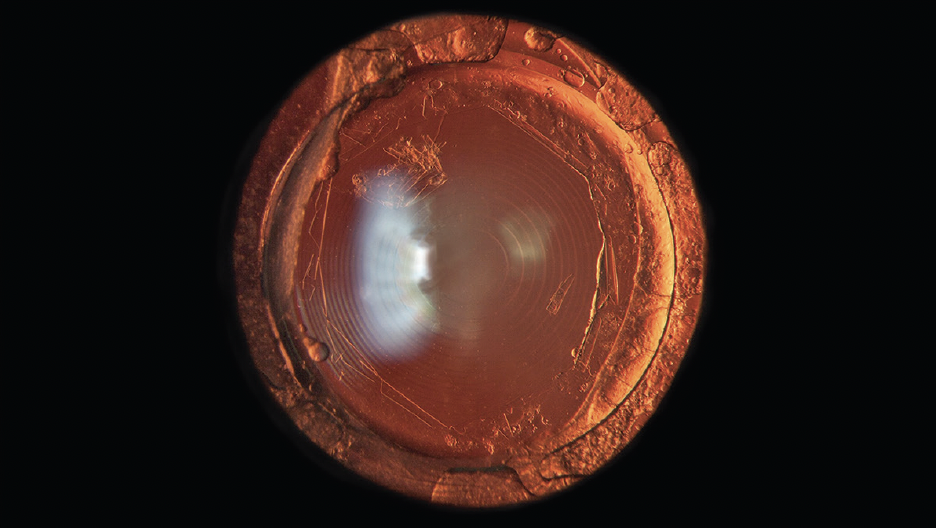
Figure 1. An iatrogenic floater is visible behind a multifocal IOL.
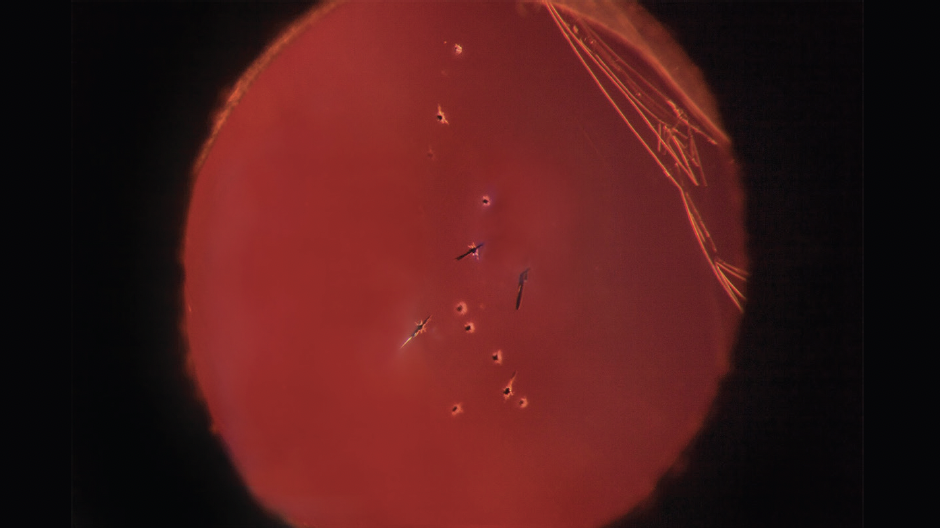
Figure 2. Damage to an IOL caused by Nd:YAG capsulotomy.
Two common complications that occur during Nd:YAG laser capsulotomy are pitting of the IOL optic, which can lead to disturbing light effects, and creating too small of a capsulotomy opening. Both can affect postoperative outcomes, especially with premium IOLs. Both can also be avoided by following the treatment guidelines detailed here.
Another fundamental source of error is performing the treatment without a contact lens, which concentrates the laser energy to an optimal point of focus. The Nd:YAG beam is delivered at a convergence angle of 16º from the laser aperture and further focused through a capsulotomy contact lens, increasing the convergence angle to 24°.
TREATMENT GUIDELINES
A premium YAG posterior capsulotomy technique begins with proper patient positioning. The patient should be comfortably seated and restrained from moving their head with help from an assistant. A contact lens such as the Brasse Widefield Capsulotomy Lens (Ocular; Figure 3) is applied to control eye movement and improve the optical efficiency of the laser energy delivery.

Figure 3. The Brasse Widefield Capsulotomy Lens.
The binocular eyepieces should be adjusted to the treating physician’s refraction. Because a conventional posterior offset does not allow the cavitation bubble, formed by YAG optical breakdown, to complete its natural life cycle, an offset of up to 2 mm is selected on the laser. This provides significantly more protection against damage to the IOL.3,4 Additionally, a sufficient posterior offset ensures the collapsing cavitation bubble is positioned far enough away from the IOL to produce a powerful jet effect, cleanly dissecting tissue with minimal debris.3,4
Laser equipment with an integrated posterior offset of 2 mm is recommended. The Tango Reflex™ Neo by Ellex (Lumibird Medical) is the only laser with a posterior offset greater than 500 μm. Prior to the laser’s extended offset availability, I would manually perform a 2-mm offset by leaving the manufacturer’s offset control set to 0 and moving the slit lamp instinctively. The device performs with exact equivalence to my ordinary manual offset YAG technique.
The YAG procedure should be performed in a dark room. The patient is instructed to fixate with their fellow eye on the green fixation light (set at minimum intensity). A clean contact lens is applied to the eye with a viscous gel interface such as sodium hyaluronate 1.8%, free from air bubbles. It can be helpful to use the ridge of the patient’s forehead rest as a support to stabilize the surgeon’s hand along with an elbow support.
Minimum slit illumination intensity is used, with binocular magnification preferably of 10 or 16. The two green aiming beams are focused to coalesce as one beam at the center of the visual field on the posterior capsule and an initial laser pulse is delivered.
The shape of the initial capsule opening will generally resemble a polygon. The polygon angles are under tension. The laser is positioned systematically at each angle while a pulse is fired to extend the capsulotomy diameter, creating a symmetrical exposure behind the IOL. The shape of the polygon can be changed by firing a laser pulse midway between two angles, increasing the number of sides by one. A series of low-energy laser pulses can be applied beneath the capsule edges to dislodge residual lens epithelium. This results in clean, perfectly curled capsule edges (Figure 4).
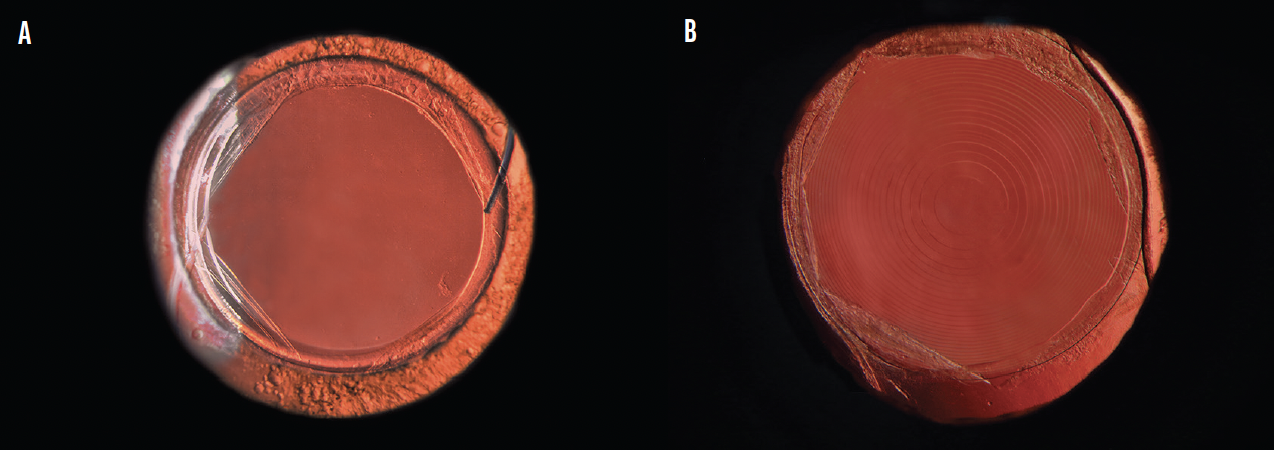
Figure 4. After Nd:YAG posterior laser capsulotomy treatment with PROcap™ in eyes with monofocal (A) and multifocal (B) IOLs.
The technique presented here works best when the PCO is a pearl type. Optimizing the posterior capsule opening in fibrotic PCO is more difficult, but good results can be achieved with patience.
Dr. Brasse explains the PROcap treatment guidelines at the 2022 ESCRS symposium.
OTHER CONSIDERATIONS
An Nd:YAG posterior capsulotomy laser treatment can only be achieved with simultaneous removal of the anterior vitreous body border membrane. It is not always easy, however, to remove this completely, and any remaining strand of vitreous can become stretched by the inwardly rolled capsule, potentially developing great tension. The search for such vitreous traction bands must be meticulous. Most times, they are easy to cut with pulses of low energy, tearing them like a rubber band.
Other fundamental considerations include regular inspection and calibration of the laser equipment. We suggest meticulous care of contact lenses using compressed air and a Hama lens-cleaning pen to keep them free of dust and debris.
FILM FESTIVAL AWARD RECIPIENT
Dr. Brasse has been the recipient of several film festival awards for innovative ophthalmic YAG laser applications.


CONCLUSION
Following the guidelines outlined here can help surgeons perform a very clean and safe Nd:YAG posterior capsulotomy that is free from iatrogenic floaters and without any damage to IOLs. Performing this treatment is our patients’ best opportunity to return to their baseline BCVA after experiencing PCO.
1. Awasthi N, Guo S, Wagner BJ. Posterior capsular opacification: a problem reduced but not yet eradicated. Arch Ophthalmol. 2009;127(4):555–562.
2. Gomaa A, Liu C. Nd:YAG laser capsulotomy: a survey of UK practice and recommendations. Eur J Ophthalmol. 2011;21(4):385-390.
3. Hawlina G, Drnovsek-Oluk B, Mozina J, Gregorcic P. Photodisruption of an thin membrane near a solid boundary: an in vitro study of laser capsulotomy. Appl. Phys. A. 2016;122:118.
4. Orthaber U. Development and evaluation of a laser for posterior capsulotomy–doctorial thesis. University of Ljubljana, Faculty of Mathematics and Physics, Department of Physics.
5. Isselin JC, Alloncle AP, Dufresne D, Autric M. Behavior of a cavitation bubble near a solid wall. Contribution to the study of the erosion mechanism. Houille Blanche. 1997;83(6):29-33.


