
A radialized anterior capsulotomy usually occurs as a result of posterior or intralenticular pressure. But it may also occur during phacoemulsification or automated irrigation and aspiration if the edge of the capsulotomy is weak, as is occasionally observed with a laser capsulotomy. This article describes strategies for preventing and managing this complication.
POSTERIOR PRESSURE
When performing the capsulorhexis, surgeons can usually sense if its edge is centrifugalizing. The first step in this situation is to look for obvious causes of posterior pressure. Examples include those described herein.
No. 1: A lid speculum opened too wide can transfer pressure to the globe. Loosening a tight lid speculum and deepening the anterior chamber with a dispersive OVD to flatten the anterior capsule can help to stabilize a capsulotomy that is starting to radialize.
No. 2: Retrobulbar or peribulbar injections. If an injection is administered, pressure on the closed eyelids and globe delivered manually with the fingers or with a Honan balloon or Mercury bag should be maintained for at least 3 to 5 minutes after the block to minimize the bleeding that may occur and to help disperse orbital fluid. Using hyaluronidase in retro- and peribulbar injections helps the bolus of fluid to disperse in the retrobulbar tissues, thereby minimizing posterior pressure.
No. 3: The presence of silicone oil in the posterior segment. Silicone oil can usually be removed before cataract surgery. If the patient has a chronic retinal detachment, however, it may have to stay in place. An overfill of oil may be suspected if the anterior chamber is very shallow and an A-scan shows that the lens is not thick and the eye is not short. In this situation, it is necessary to vent the posterior segment with a sclerotomy located 3.5 mm posterior to the limbus to burp out some oil prior to creation of the capsulorhexis. It is difficult to evacuate silicone oil with a cannula on a syringe.
VECTOR FORCES
Not allowing the diameter of the capsulotomy to exceed 5.5 mm helps to prevent radialization. I like to use a double cross-action Utrata-type forceps (Bakewell-Haldipurkar Forceps, Epsilon), which has an etching 5 mm from the tips to facilitate sizing of the capsulotomy.
If the capsulotomy becomes large, it can approach the edge of the capsular bag, which is more convex than the central capsule, causing the capsulorhexis to radialize. If the zonules extend significantly onto the anterior capsule, it is best to keep the capsulotomy anterior to them to prevent radialization.
During the capsulorhexis, the forceps for the capsulotomy should be positioned 25º to 90º centripetal to the direction of the actual tear. Keeping the capsulorhexis forceps at the plane of the anterior capsule helps to prevent radialization.
WHITE CATARACT
Intumescent white cataracts are notorious for causing radialization of the anterior capsulorhexis, resulting in the Argentinian flag sign (Figure 1) caused by the intralenticular pressure from liquified cortex. Figueiredo et al postulated that liquefied cortex exists both anterior and posterior to a large nucleus that prevents communication between the two compartments.2 Both the anterior and posterior compartments must be decompressed to prevent an errant capsular tear.
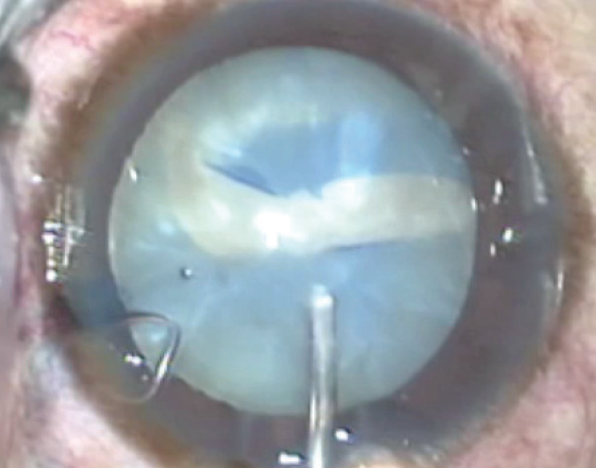
Figure 1. Argentinian flag sign.
As suggested by Figueiredo et al,1 patients with a white cataract should receive 250 mL of 20% mannitol 50 minutes before cataract surgery to dehydrate the vitreous and minimize other sources of posterior pressure. If a retro- or peribulbar anesthetic block is being used, pressure should be applied to the lids in the manner described earlier in this article to soften the orbit. It is important to stain the capsule (trypan blue dye produces more intense staining than indocyanine green dye) so that the anterior capsule can be visualized during the capsulorhexis. The dye should be painted on the anterior capsule, either under air or an OVD. If the dye is simply injected into the anterior chamber, it may pass posteriorly through a zonular dehiscence and stain the posterior capsule and vitreous. This may impair visualization of the anterior capsule.
Figueiredo et al also recommended using a dispersive OVD and decompressing intralenticular pressure with a 27- or 30-gauge needle (attached to a 3-mL syringe) introduced bevel down through a paracentesis incision and into the center of the anterior capsule (Figure 2). When the anterior capsule is punctured, gentle retraction of the syringe aspirates liquid cortex in the anterior compartment of the bag. By gentle retropulsion of the nucleus, liquid cortex in the posterior compartment may then be decompressed. A 3-mm capsulorhexis is created with coaxial forceps through a paracentesis incision, followed by bimanual irrigation and aspiration to the capsular bag to ensure that intralenticular pressure is relieved. The capsulotomy is then enlarged to 5 mm, and phacoemulsification proceeds.
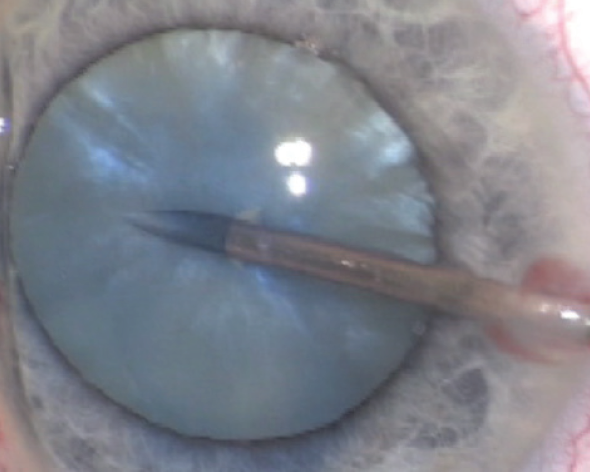
Figure 2. A 27- or 30-gauge needle (attached to a 3-mL syringe) is introduced bevel down through a paracentesis incision and into the center of the anterior capsule to help control intralenticular pressure.
MANAGEMENT
If radialization of the capsulorhexis occurs, it is often possible to retrieve the edge with a rescue maneuver described by Brian Little, MA, FRCS, FRCOphth, FHEA.2 In this technique, the capsulorhexis edge is tensioned by pulling it back in the direction from which it originated and pulling it centrally to initiate the return of the tear (Figure 3). All of the pulling must be done in the capsular plane.
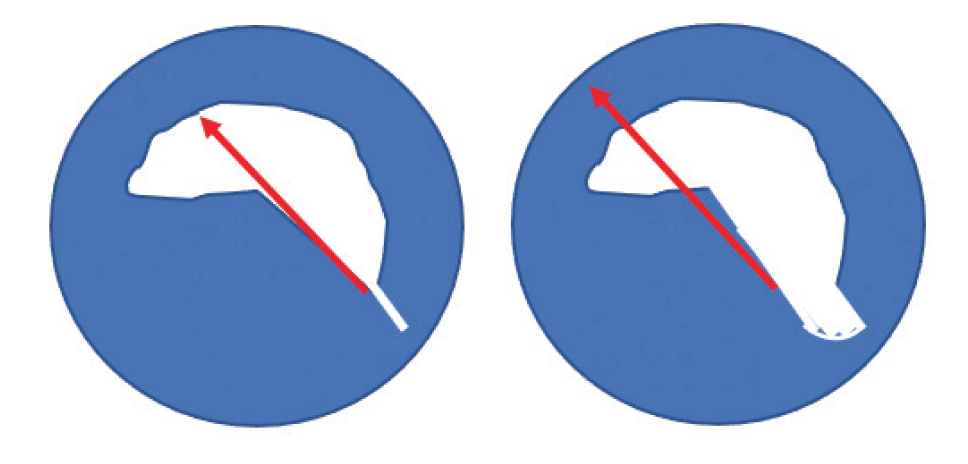
Figure 3. Dr. Little’s rescue maneuver. The red arrows show forceps vector force to rescue an errant capsulorhexis.
If a radial tear cannot be retrieved, the capsulotomy should be completed from the opposite direction, and an attempt is made to encompass the errant edge. If this is not possible, then phacoemulsification must be performed cautiously to prevent the tear from extending across the posterior capsule. My preferred technique is phaco quick chop because it places less stress on the bag and zonules than divide and conquer techniques. Alternatively, the lens can be prolapsed anterior to the bag into the supracapsular position or anterior chamber so that phacoemulsification may be performed under a copious amount of a dispersive OVD. It is usually possible to place a one-piece IOL in the bag despite an anterior capsular tear.
Key Points
- An errant capsulorhexis edge can frequently be rescued with a maneuver described by Brian Little, MA, FRCS, FRCOphth, FHEA.
- Decompressing an intumescent white cataract with a 27- or 30-gauge needle is helpful in preventing the complication commonly referred to as the Argentinian flag sign.
1. Figueiredo DG, Figueiredo J, Figueiredo GB. Brazilian technique for prevention of the Argentinean flag sign in white cataract. J Cataract Refract Surg. 2012;38:1531-1536.
2. Little BC, Smith JH, Packer M. Little capsulorhexis tear-out rescue. J Cataract Refract Surg. 2006;32:1420-1422.


