

Middle segment surgery includes a broad spectrum of anterior segment surgical and reconstructive procedures. These cases present unique challenges and great variety, requiring the ophthalmologist to anticipate diverse surgical scenarios. Preparation is key. Surgical technique is tailored to each specific case. A comprehensive examination of both the anterior and posterior segments is essential to devising a primary surgical strategy and alternative approaches.
Complex procedures such as traumatic cataract with zonulopathy, IOL exchange in the setting of an open capsule, repositioning of a subluxated IOL, and/or secondary IOL placement with scleral fixation require safety, accuracy, and reproducibility. Understanding how to handle vitreous prolapse, clear the area of potential vitreous traction, and visualize the middle segment for safe fixation of an IOL is paramount. Fortunately, simulation models are available to practice techniques such as pars plana–assisted anterior vitrectomy and scleral fixation. This preparation can give the surgeon experience and muscle memory to have a deliberate technique and add confidence to perform safe and accurate surgery.
The preoperative clinical examination is a crucial step in assessing a patient’s visual potential and preparing for surgery. When possible, reviewing medical records, including prior operative reports, allows the surgeon to understand the specifics of the IOL type, previous visual potential, and comorbid conditions such as corneal edema, glaucoma, and/or retinal pathology. Dilation should be deferred until a relative afferent pupillary defect and iris defects are assessed and documented. These patients often have iatrogenic iris trauma, sphincter damage, or transillumination defects due to IOL chafe, which can result in debilitating glare. Careful documentation of their visual acuity and visual potential (using a retinal acuity meter) as well as glare testing can assist in setting realistic expectations for overall visual function postoperatively. Reviewing the patient’s IOP history and current measurements can help identify a potential risk of glaucomatous damage to the optic nerve, affecting the prognosis and subsequent counseling. Additionally, patients should be assessed while the patient is in both an upright and supine position to anticipate if a posterior approach is necessary to retrieve the subluxated IOL. All patients should undergo endothelial cell density testing/pachymetry, retinal nerve fiber layer measurements, and macular OCT testing preoperatively to determine comorbid conditions. Lastly, continued postoperative monitoring for corneal edema, uncontrolled IOP, and retinal tears or edema is critical to long-term success in these challenging cases.
SLIT-LAMP EXAMINATION
A methodical approach to the slit-lamp examination is advisable. The lids and fornices should be evaluated for signs of exposure or lagophthalmos. The conjunctiva and sclera should be carefully inspected for the presence of scleral buckles, filtering tubes, and trabeculectomy, which may affect the incisional approach and fixation method. The health of the conjunctiva often dictates the choice of new or existing IOL fixation techniques. For example, flanged techniques and Hoffman pockets, which spare conjunctiva, are ideal when this tissue is scarred or requires preservation for future filtering procedures. Areas of scleral thinning should be documented and avoided during the placement of trocars and sclerotomies. The integrity of the limbus and ocular surface is assessed for compromise, which influences decisions on surface lamellar (deep anterior lamellar keratoplasty, penetrating keratoplasty) or internal lamellar corneal transplantation (ultrathin Descemet stripping endothelial keratoplasty, pre-Descemet endothelial keratoplasty, or Descemet membrane endothelial keratoplasty) transplantation. Significant ocular surface disease or keratitis should be evaluated and treated before surgical intervention to improve the overall visual prognosis. Dense corneal scarring and the presence of microcystic edema and bullae also change the consideration of graft type and may give rise to challenging intraoperative views. Gonioscopy is performed to determine the extent of angle damage and recession, peripheral anterior synechiae, and cyclodialysis clefts and the integrity and pigmentation of the trabecular meshwork. The presence of endothelial compromise and angle damage is common in this patient population. Proper counseling regarding the potential need for additional surgical intervention is necessary to set realistic postoperative expectations.
Next, an assessment of the status of the crystalline lens in the case of a complex cataract with zonulopathy or IOL type should be as detailed as possible. In the case of a crystalline lens in an eye with zonulopathy, documentation of an asymmetric anterior chamber, extent of zonule loss, vitreous prolapse, and phacodonesis is helpful. When describing a subluxated or malpositioned IOL, the type of IOL (one- or three-piece acrylic), capsule or sulcus placement, capsule integrity (fibrosis, phimosis, or dead bag), anterior capsular opening, posterior capsule status, Soemmering ring, and extent of pseudophacodonesis can facilitate surgical planning. As mentioned earlier, evaluating the patient in both the supine and upright position allows the surgeon to determine the best access to the subluxated IOL.
DILATED EXAMINATION
A dilated examination is crucial to evaluate the macula, periphery, vitreous status, and vessels. Additionally, determining the extent of zonular weakness is easier in the dilated state. In the event that the pupil does not dilate well, ultrasound biomicroscopy (UBM) can help identify the location of the existing IOL.
In a phakic eye, the clock hours and specific locations of zonular laxity should be documented. The observation of signs such as lens tilt and higher-order aberrations, such as coma during aberrometry, suggests zonular impairment. Conventionally, a threshold of 3 or 4 clock hours of zonular compromise warrants consideration of additional zonular support for tension redistribution. For greater zonular weakness, supplementary scleral fixation methods may be required to achieve long-term lens stability. These may include the placement of a modified capsular tension ring (Morcher Cionni Ring, FCI Ophthalmics) or one or more capsular tension segments (Morcher Ahmed Segment, FCI Ophthalmics) in addition to a standard capsular tension ring.
In pseudophakic patients, the level of zonular weakness, integrity of the capsule, and the severity of lens subluxation are critical to deciding between attempted lens repositioning with scleral fixation or a lens exchange.
ADDITIONAL DETAILED INSPECTIONS
The iris. Conditions such as dyscoria, iridodonesis, and aniridia are often associated with middle segment trauma but may be congenital. These conditions can be categorized as structural or functional anomalies. Structural anomalies range from minor focal traumatic iridectomy to a complete loss of iris tissue. It is critical to document the extent of iris tissue loss because this information greatly influences decisions on reconstruction. Iris defects of less than 3 clock hours may be suitable for primary reconstruction, whereas an iris prosthesis (prosthetic iris or iris segment within the capsule) is generally required for larger defects to achieve satisfactory functional and aesthetic outcomes. Functional anomalies, such as damage to the iris sphincter, manifest as varying degrees of pupillary mydriasis, which can be either diffuse or localized. Management strategies for these defects often include partial or total pupillary cerclage. Occasionally, intraoperatively, the residual iris tissue may be “unfurled” despite looking fragmented at the slit lamp, which may permit direct closure more easily than initially anticipated.
Vitreous prolapse. Vitreous is often encountered in the anterior chamber in cases of ocular trauma, especially those with accompanying zonular damage. The extent and location of vitreous prolapse, including the clock hours affected, must be documented to facilitate effective surgical planning. Corneal endothelial integrity should be carefully evaluated in the presence of vitreous in the anterior chamber because wicks of vitreous may dramatically reduce the endothelial cell count over time, increasing the risk of postoperative corneal decompensation. When the presence of vitreous is suspected but not visible at the slit lamp, an intraoperative injection of preservative-free triamcinolone acetonide or washed triamcinolone acetonide (Kenalog, Bristol-Myers Squibb) dilution of 1:10 with balanced salt solution can assist with visualization and removal. It is important to note that OVDs can block the uptake of washed Kenalog, and vitreous and an OVD may look similar in the anterior chamber, thus requiring careful differentiation at the time of surgery. The surgeon can remove the OVD with a vitrector and then stain the vitreous to get a better understanding of the extent of vitreous prolapse.
The capsule. The status of the anterior and posterior capsules is assessed. The areas and extent of tears, fibrosis, and iridocapsular synechiae are identified. It must also be determined whether enough capsular tissue remains to support an IOL. Optic capture with a three-piece IOL, involving haptics in the sulcus and the optic captured posterior to the anterior and/or posterior capsule, may be possible in some cases, mitigating the need for more complex lens fixation techniques. There should be adequate equatorial zonular support and an anterior and/or posterior capsular opening of 5.0 to 4.8 mm for the best results (Figure).
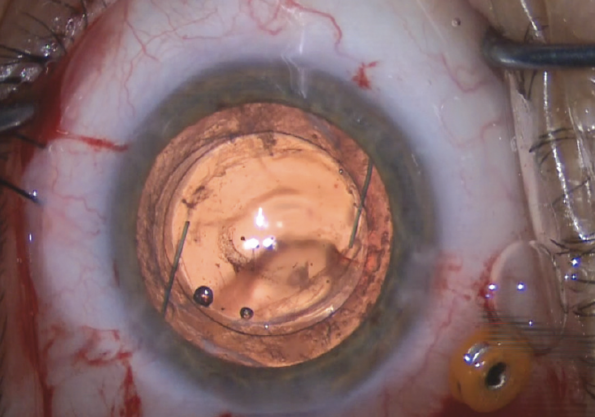
Figure. Optic capture of a three-piece IOL. A three-piece IOL with haptics in the sulcus and the optic captured posterior to both the anterior and posterior capsules. A pars plana–assisted anterior vitrectomy was performed before the placement of the IOL.
(Figure courtesy of Nicole Fram, MD)
IMAGING TECHNIQUES
Anterior segment OCT. This imaging technique is invaluable for detailed assessments of regional pachymetry, epithelial thickness, anterior chamber depth, lens tilt, and lens vault, particularly in eyes with uveitis-glaucoma-hyphema syndrome. The noninvasive measurement of these parameters provides crucial data for surgical planning and diagnosis.
Biometry. Despite the complexities associated with anterior segment reconstruction, accurate biometry remains a cornerstone of optimizing refractive outcomes in eyes with reasonable visual potential. Targeting a slightly myopic (-1.00 to -2.00 D) outcome can provide patients with functional vision and accommodate potential adjustments for future corneal transplants depending on the level of corneal edema. McMillin et al1 found that, in patients undergoing an IOL exchange with intrascleral haptic fixation, the arithmetic refractive prediction error was generally hyperopic. The suggested targeted myopia to achieve emmetropia was -0.75 D.
Endothelial cell count. Knowing the endothelial cell density is crucial for preoperative counseling. A low count (cell count of 800–1,000) combined with increased pachymetry and the presence of bullae or microcystic edema may change decision-making to include an endothelial keratoplasty at the time of surgery. A reasonable endothelial cell count (cell count of 1,200 or more) and a clear cornea/graft may warrant observation, where early failure or edema may prompt the employment of stimulatory topical medications such as Rho kinase inhibitors to harness the residual endothelial regeneration potential. Endothelial cell density also aids in counseling the patient on the possibility of lamellar keratoplasty in the future.
Clinical photography. Often underutilized, clinical photography is a remarkably useful tool for preoperative planning. It aids in determining the dimensions of the surgical approach, particularly decisions regarding sutured or flanged techniques and incision placement. This can enhance the precision and efficacy of surgical intervention and reduce complications (such as accidental planning of a scleral fixation technique where a bleb might preclude access).
B-scan ultrasonography. Visual assessment of the retina can be hindered by media opacity. In such instances, B-scan ultrasonography is instrumental in assessing retinal integrity and ruling out shallow or funnel-shaped retinal detachments.
UBM. UBM is invaluable for detailed examinations of anterior ocular trauma; delineation of traumatic iris and implantation cyst anatomy; and assessments of angle structures and damage (including recession extent), a Soemmering ring, and the location and tilt of IOLs. When compared to anterior segment OCT, the advantage of UBM is its ability to visualize structures posterior to the iris, such as the ciliary body and lens.
1. McMillin J, Wang L, Wang MY, et al. Accuracy of intraocular lens calculation formulas for flanged intrascleral intraocular lens fixation with double-needle technique.


