INTRODUCTION
Myriad IOL technologies are available today. Monofocal, monofocal plus/enhanced monofocal, extended depth of focus (EDOF), multifocal, trifocal, and accommodating are some of the classifications used to describe optical technologies of IOL designs. Understanding the differences between advanced IOL technologies is an important topic of discussion among refractive cataract surgeons. Enhanced monofocal, EDOF, and trifocal IOLs all provide varying impact to near, intermediate, and distance vision as well as varying need for the use of glasses. The use of different nomenclature, however, can get confusing for patients and surgeons alike and complicate how the advantages and disadvantages of each lens type are understood.
To gain insight into how surgeons are using various IOL technologies, what characteristics drive this choice, and what patient types benefit from the various lenses, HOYA Surgical Optics conducted an online survey of 17 well-respected cataract and refractive surgeons from 11 countries (Australia, Austria, Belgium, France, Germany, India, Italy, Japan, South Africa, South Korea, and the United Kingdom) and hosted a roundtable discussion at the ESCRS 2022 meeting in Milan. For the purpose of the online survey and in-person meeting, the company used the following terminology: monofocal (IOLs that provide optimal distance vision), enhanced monofocal (IOLs that provide optimal distance and some intermediate vision), increased range of focus (IROF; IOLs that provide optimal distance and intermediate vision), and full range of focus (FROF; IOLs that provide optimal vision at all distances). Advanced technology IOLs (ATIOLs) encompass IROF, FROF, and toric IOLs.
The survey also assumed the following definitions for mini- and standard monovision, respectively: one eye target at plano and the other eye target at -0.50 to -0.75 D, and one eye target at plano and the other eye target at -1.00 D or more.
This is a summary of the discussion.
IOL DECISION-MAKING
Francesco Carones, MD: Patient demands are at an all-time high. This affects the way in which we select IOLs for our patients today. To summarize the online survey results,1 the distribution of IOL preference has changed over the past 3 years and will continue to change in the next 3 years. Survey respondents reported using monofocal IOLs less frequently and enhanced monofocal more frequently now than 3 years ago. They also pointed to using standard monofocal IOLs even less over the next 3 years, favoring even more frequent use of enhanced monofocal IOLs. Respondents also reported increasing their use of IROF and FROF IOLs.
The ATIOL sector is clearly growing. How does everyone approach the decision-making process? Do you tell patients about the different IOL options during their assessment only when they show interest in an advanced technology IOL, do you generally assume all patients are candidates for advanced technology IOLs until something in their diagnostic assessment indicates differently, or do you generally assume all patients are not candidates for an ATIOL and will only receive one if their assessment demonstrates that they are a good candidate? (The responses from the survey respondents are depicted in Figure 1.)
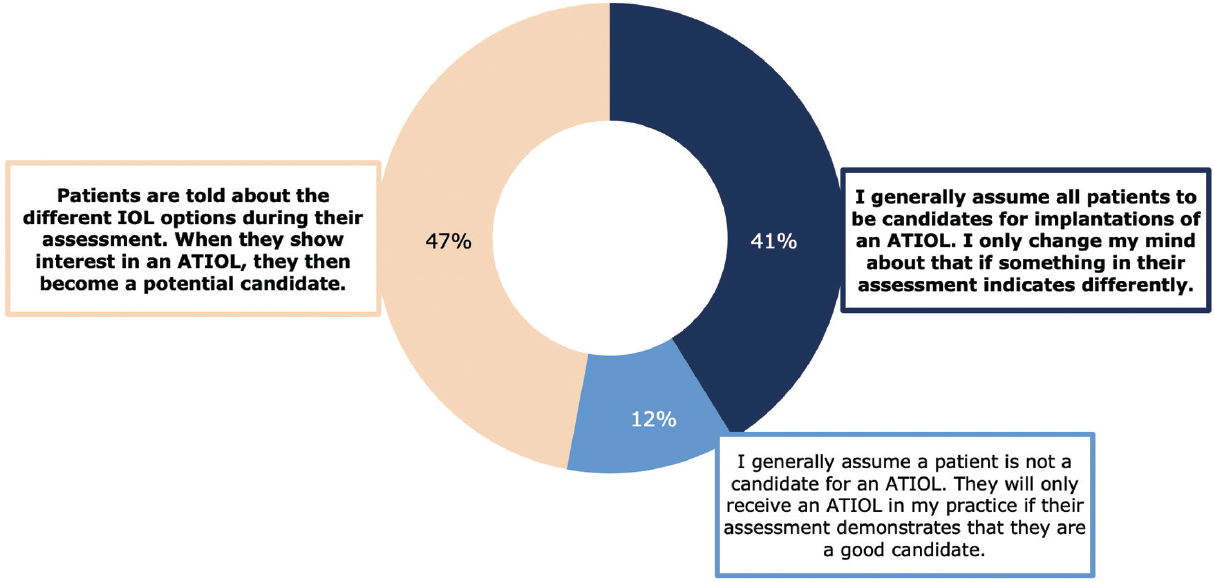
Figure 1. Respondents indicated which sentence best represented the decision-making process used at their practice.1
Mohammed Muhtaseb, FRCOphth: I think of every patient as a candidate for ATIOLs, but I don’t discuss the lens options with patients until after they’ve been examined. If the diagnostic findings show macular degeneration, for example, I no longer consider them a candidate.

Dr. Carones: Are patients such as the one you describe excluded before they meet with you?
Dr. Muhtaseb: My setting might be unique in this group because I perform the diagnostic tests myself. I talk to patients about their options during the assessment. When they show an interest, then they become a candidate.
Raphael Barraquer, MD, PhD: My answer depends on if the patient is older with established cataracts or younger with clear lenses or early cataract and interested in refractive lens exchange. While patients in the latter group are automatically candidates for an advanced technology IOL, this may not be the case for the patients in the former group, depending on their interests and requests. In any case, they all are screened in advance with a refraction and topography of both the anterior and posterior surfaces to assess whether they are good candidates for an IROF or a FROF trifocal IOL.
Erik L. Mertens, MD, PhD: For me, every patient is a candidate for ATIOLs until proven otherwise. An 80-year-old patient with perfect retinas is just as much a candidate as a 65-year-old with perfect retinas. Even if a patient does not show interest in ATIOLs, they are still educated about them.
Ramin Khoramnia, MD, FEBO: Not all patients are suitable for these lenses, but we always educate patients about them. For example, I would tell a patient with geographic atrophy that presbyopia-correcting lenses are available but that they are not a candidate. Otherwise, when the patient hears from a family member or friend about their happiness with a multifocal lens, the patient becomes dissatisfied that they were not informed about these IOL options.
Dylan A. Joseph, MBChB, Dip(ophth), FCOphth, MMEd: The answer to this question really pertains to what style of practice one has. As a refractive surgeon, I want every patient to have an advanced eye assessment. Most patients are not sure what IOL they want until they’ve been through the assessment process. The diagnostic results help me form my opinion as to whether they’re a good candidate or not. But the point is everyone gets the same level of diagnostic testing from the outset. If patients are good candidates for ATIOLs after a thorough evaluation and understanding of their visual needs, we then discuss ATIOLs. My approach to educating patients about lens designs is the same for all—assess patients first, then meet expectations if they are candidates.
Tamer Tandogan, MD: I see patients two times before the operation. The first appointment is to assess whether cataract surgery is indicated. If it is, a second assessment is scheduled, at which time diagnostics are performed. I help patients decide on the type of IOL they want at the second appointment. I think it’s our duty to inform patients about all options, even if they are not candidates for certain IOLs. Otherwise, as Dr. Khoramnia said, patients can come back asking, “Why didn’t you tell me about this option?”
Pascal Rozot, MD: When a patient comes into my clinic and the first thing they express is desire for a premium IOL, I make note of this but do not address the topic right away. I think it is important to first obtain an assessment of their candidacy using specific diagnostic tests. Conversely, some patients don’t know what options are available to them. I consider it my duty to supply them with all the information so that they can make an informed decision. In all cases, patient motivation is at the heart of the choice.
Catherine Albou-Ganem, MD: I inform patients of all options, and they have gone through all the diagnostic exams before seeing me. I prefer FROF IOLs, but not all patients want a lens of this type. I let their desires dictate the IOL choice.
Dr. Mertens: I find it helpful to explain to patients that they can be free of glasses with these and other ATIOLs. I am always surprised that many patients do not know that is possible.
MINI-MONOVISION VERSUS IROF
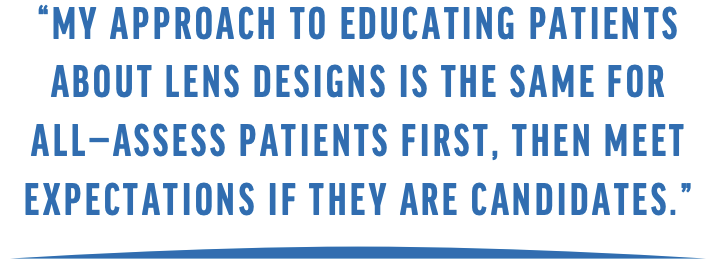
Dr. Carones: Excluding financial costs, the choice between an IROF and a FROF IOL is generally based on what patients value more, spectacle independence or quality of vision. Most of us would agree that a FROF IOL is often best for those who are highly motivated by the former and are willing to tolerate nighttime halos, while an IROF IOL is better suited for patients who are unlikely or unwilling to tolerate nighttime halos. The results from the online study sponsored by HOYA Surgical Optics reflect this thought process (Figure 2).
Figure 2. Respondents indicated how strongly they agreed with the following statement: Excluding financial costs, the choice as to whether an IROF or a FROF IOL is implanted is generally based on a tradeoff between how motivated the patient is to be spectacle independent versus how willing or likely they are to tolerate a reduced quality of vision.
For patients who are unlikely to tolerate visual symptoms such as nighttime dysphotopsias, which are associated with common FROF designs, but who also desire a greater degree of spectacle independence than afforded by a monofocal IOL, 53% of respondents to the online survey answered that they prefer to implant IROF IOLs with either a mini-monovision strategy (35%) or targeting plano (18%). About one-third (35%) prefer enhanced monofocal IOLs with either a mini-monovision strategy (29%) or targeting plano (6%).1
Dr. Khoramnia: In terms of IOL selection, I spend time getting to know patients so that I can understand what they really want in everyday life. We then decide together what IOL will be best for them. Many patients are happy with slight mini-monovision and an enhanced monofocal IOL. If patients desire spectacle independence for reading, however, then I choose an FROF IOL (ie, trifocal) and counsel the patient about the possibility of photic phenomena and night driving problems. Patients who choose an enhanced monofocal pay significantly less than those who choose a trifocal.
Dr. Barraquer: In my experience, patients achieve the same quality of distance vision with IROF and enhanced monofocal IOLs. Some patients insist on having the best possible vision for certain tasks, and I use that as criteria to choose between these two options. Those choosing a monofocal IOL become natural candidates for mini-monovision.
Dr. Khoramnia: It can be easy to decide what patient gets a FROF IOL when they want full spectacle independence at all costs, but it becomes tricky when they will not accept the side effects. Patients who want spectacle independence but will not tolerate side effects need to know that they will have better quality of vision with an IROF IOL, but might need reading glasses. Patients need to understand that there is no such thing as a so-called free lunch in optics. They must accept either wearing glasses more frequently or photic phenomena. I always tell my patients that we do not yet have fully accommodating IOLs, which might provide the vision of a 20-year-old emmetrope without side effects.
Dr. Rozot: With mini-monovision, patients will not gain a powerful near vision, so you cannot promise spectacle independence.
Navid Ardjomand, MD: Patients are generally dissatisfied with IROF IOLs when they do not achieve spectacle independence but thought they would. For patients that want greater spectacle independence but who will not tolerate side effects, I lean toward a mini-monovision strategy with an enhanced monofocal IOL because patients tend to be happy with their range of vision. They say, “Doctor, I still need reading glasses sometimes, but for normal activities I don’t need them. Thank you very much.” Further, these patients tend to be great advocates for my practice and generate word-of-mouth referrals.
ENHANCED MONOFOCAL IOLS: USAGE AND STRATEGY
Dr. Carones: Is an enhanced monofocal IOL suitable for all cataract patients who would otherwise receive a monofocal, or does it depend on the model?
Dr. Rozot: I think these lenses may be used routinely as a replacement for monofocals, especially for our active patients who participate in sports. I also prefer enhanced monofocal IOLs for patients who undergo combined cataract and glaucoma surgery.
Dr. Carones: I agree.
Dr. Barraquer: There seems to be no downsides currently to an enhanced monofocal IOL. They provide almost the same benefits as standard monofocal IOLs with enhanced performance for medium distances. For me, it only remains to be seen if all enhanced monofocal IOLs will meet the needs of patients desiring best possible distance uncorrected vision, for example frequent night drivers. And perhaps those not caring about using a near correction may still be better candidates for classic monofocal IOLs.
Dr. Ardjomand: I agree, but I am conservative in patients with retinal problems like wet or dry age-related macular degeneration. In these eyes, visual acuity might not be as crisp with an enhanced monofocal IOL compared to a standard monofocal.
EARLY EXPERIENCE WITH THE VIVINEX IMPRESS ENHANCED MONOFOCAL
Dr. Carones: My early experience with the hydrophobic Vivinex Impress enhanced monofocal IOL (HOYA Surgical Optics; Figure 3) is positive. The IOL comes preloaded in the multiSert injector system (HOYA Surgical Optics), which can be used with either a single-handed push or two-handed screw injection (Figure 4). The adjustable insert shield modulates the insertion depth according to surgeon preference; no other IOL delivery system offers this feature.
Figure 3. The Vivinex Impress IOL.

Figure 4. The multiSert injector system.
At the time of this discussion, I have performed cataract surgery and implanted the Vivinex Impress bilaterally in 10 patients. I targeted the second (nondominant) eye for slight myopia of 0.50 D.
I like that the central part of the Vivinex Impress IOL creates the range of vision, but a significant amount of light is still targeted for distance. I think this is the added value compared to competing enhanced monofocal IOL technologies. This feature is especially beneficial for eyes with constricted pupils like we see with glaucoma.
In my small series of patients, the quality of vision the day after surgery is excellent. Most patients can achieve 20/15 or even 20/12 distance vision, which is similar to a monofocal.
Dr. Khoramnia: At the time of the roundtable discussion, I had implanted the Vivinex Impress IOL in 14 eyes of 10 cataract surgery patients. Postoperatively, the mean distance UCVA was 20/20. Patients also gained about 1 line more of intermediate vision than with traditional monofocal IOLs, which is similar to what our patients typically achieve with the Eyhance IOL (Johnson & Johnson Vision). The monocular defocus curve shows that the postoperative visual acuity is 0.2 logMAR up to -1.25 D (Figure 5). An even better range of vision is achieved when testing the binocular defocus curve of patients implanted with Vivinex Impress, as we would expect.2
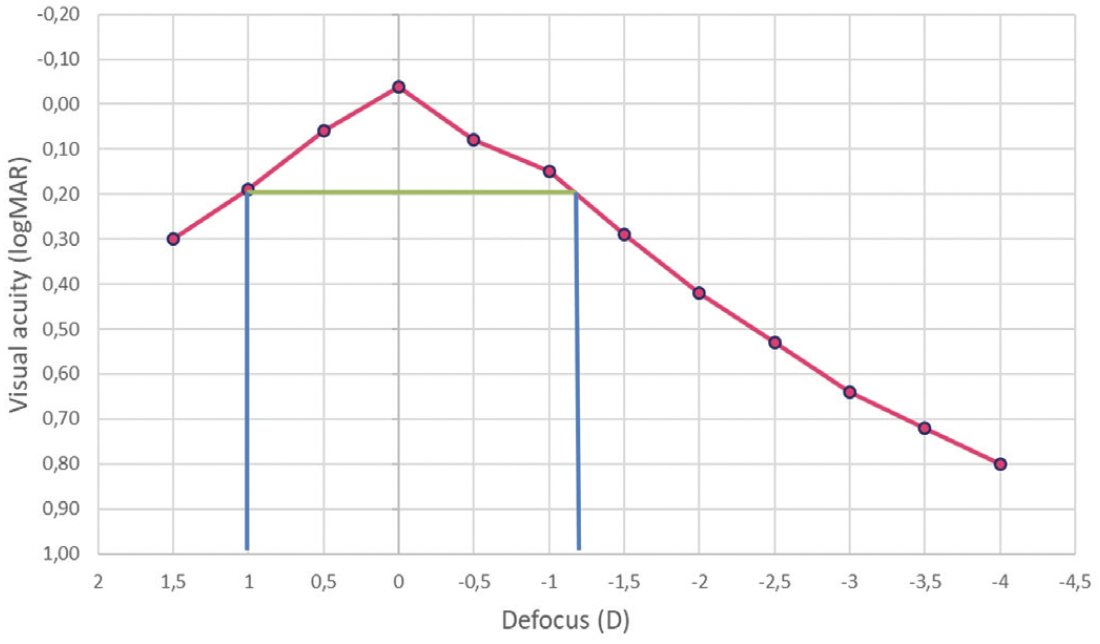
Figure 5. The mean monocular defocus curve of the Vivinex Impress IOL at 3 months postoperative in 14 eyes.2
Dr. Tandogan: I have implanted the Vivinex Impress in 16 patients at the time of this discussion. All patients were happy with their computer vision and reported no visual side effects. Near vision was also fairly good (0.3 logMAR), though most reported needing glasses to read smaller print, as we would expect. We take great care to communicate clearly during the preoperative consultation to manage patients about the range of vision they may achieve.
FROF IOLS
Dr. Carones: Going back to the online survey sponsored by HOYA, 88% of respondents felt that FROF IOLs are the best option to provide patients with the highest chance of spectacle independence. Interestingly, among the FROF IOLs, respondents did not perceive much difference in the level of spectacle independence and quality of vision.1 Do you think there is a difference between the FROF IOLs that you have been using in terms of performance, distance vision, spectacle independence, and visual side effects?
Dr. Muhtaseb: I think there is a difference, and it largely depends on what patients expect for spectacle independence. Is it standard newspaper print? Small print? N4? N5? Are they reading in good lighting or poor lighting?
Dr. Carones: From my point of view, I have seen a difference, especially with the Vivinex Gemetric (HOYA Surgical Optics). (Editor’s note: For more information on the Vivinex Gemetric, see Vivinex Gemetric: Clinical Performance Study.) In my early experience with the IOL, patients achieve an extra level of spectacle independence for smaller print, and they also get slightly better uncorrected distance visual acuity.
Dr. Rozot: I have vast experience with FROF IOLs. Based on the feedback I have gotten from patients, there’s no relevant difference regarding photic phenomena and spectacle independence. In the clinical real-world setting, it does not make a difference if patients are reading at 33 or 38 centimeters. When I implant a FROF IOL, I tell patients it might take time for them to learn what reading distance works for them.
Dr. Mertens: There might be some difference between older FROF IOL models and newer ones, but the newer ones all provide similar visual outcomes. I have seen a difference between hydrophilic and hydrophobic models, however, and not all FROF IOLs have the same stability in the eye. Some can cause more refractive changes over time.
Dr. Khoramnia: Another thing that sets a lens apart is if it comes in a preloaded injector. I think this is almost mandatory for ATIOLs. In terms of the safety of the implantation, a preloaded lens is much better. Going back to Dr. Mertens’ points, the material matters, and rotational stability matters. The Vivinex Gemetric is made from a glistening-free hydrophobic material, and obviously we know that no better material exists. Additionally, the Vivinex platform is extremely rotationally stable and does not have the drawbacks of a plate-haptic design.
Dr. Joseph: I think where HOYA Surgical Optics has got it right and is a notch above other companies with FROF IOLs is that its FROF lens is available in two designs, the Vivinex Gemetric and Vivinex Gemetric Plus, which have different light distributions weighted to either distance or near vision. The Vivinex Gemetric Plus optimizes light distribution for near, and the Vivinex Gemetric optimizes light for distance. I like to implant the Vivinex Gemetric in the dominant eye and the Vivinex Gemetric Plus in the nondominant. Patients might notice a bit more compromise in distance vision and intermediate vision at 40 cm with the Vivinex Gemetric Plus. Binocularly, however, the result is excellent distance vision and almost a full range of vision from 35 cm to 50 or even 60 cm. I think the Vivinex Gemetric Plus is an interesting concept because my patients don’t have to compromise on their near or distance vision.
Dr. Muhtaseb: In my early experience with the Vivinex Gemetric and Gemetric Plus, patients have been thrilled when I implant the same model of the lens in both eyes.
Dr. Mertens: I’ve found that, at 60 cm, the Vivinex Gemetric is slightly better than the Vivinex Gemetric Plus. On the other hand, the Vivinex Gemetric Plus gives an extra range up to 35 cm. Binocularly, I find a nice summation between 35 and 60 cm. In the series of patients I’ve done, the difference in the intermediate and near sweet spots between the two lenses is marginal.
Dr. Joseph: Thus far, I have used the Vivinex Gemetric lens in both refractive lens exchange patients and cataract patients. I like to target the first plus spherical equivalent postoperatively because patients tend to be happier with the quality of their distance vision. If even slightly myopic after surgery, patients are aware of reduced visual quality. It is essential to hit plano or first plus in my opinion. Of course, refractive lens exchange patients are known to be demanding too, so they need to understand that ATIOLs lose some light.
VIVINEX GEMETRIC TRIFOCAL FAMILY: CLINICAL PERFORMANCE SUMMARY
The Vivinex Gemetric Trifocal IOL, based on HOYA Surgical Optics’ patented technology, is available in two designs, the Vivinex Gemetric and Vivinex Gemetric Plus, that have complementary light distributions. The Vivinex Gemetric is designed to provide excellent distance vision and well-balanced intermediate and near vision, and the Vivinex Gemetric Plus is designed to provide excellent near vision while maintaining good distance and intermediate vision (Figure 1). Both Vivinex Gemetric and Vivinex Gemetric Plus have a near add of 3.50 D and an intermediate add of 1.75 D, and both are available in toric versions.
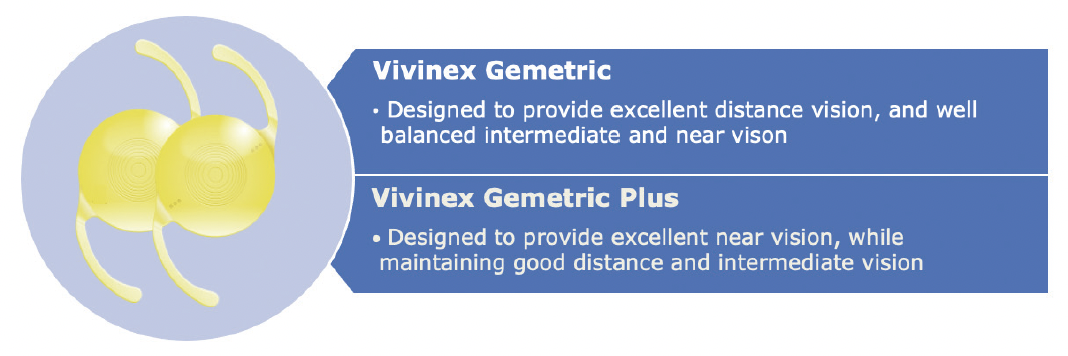
Figure 1. The Vivinex Gemetric and Vivinex Gemetric Plus optics designs.
Simulated optical comparison has shown the complementary MTF curve profiles of the Vivinex Gemetric and Vivinex Gemetric Plus (Figure 2). The light distribution profiles with both IOLs as pupil size increases are shown in Figure 3.
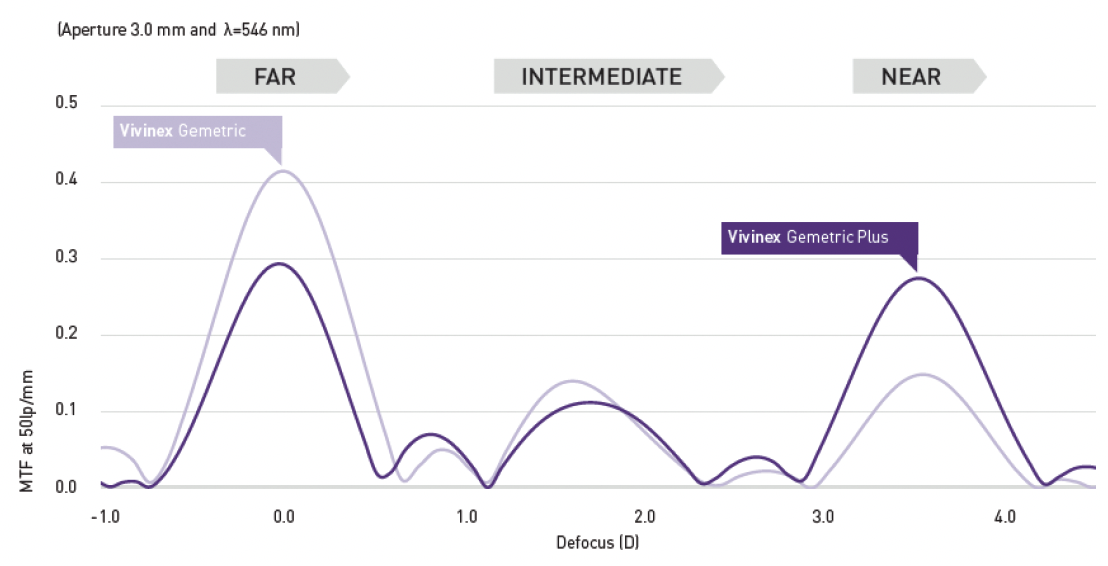
Figure 2. The complementary MTF curve of the Vivinex Gemetric and Vivinex Gemetric Plus IOLs.1
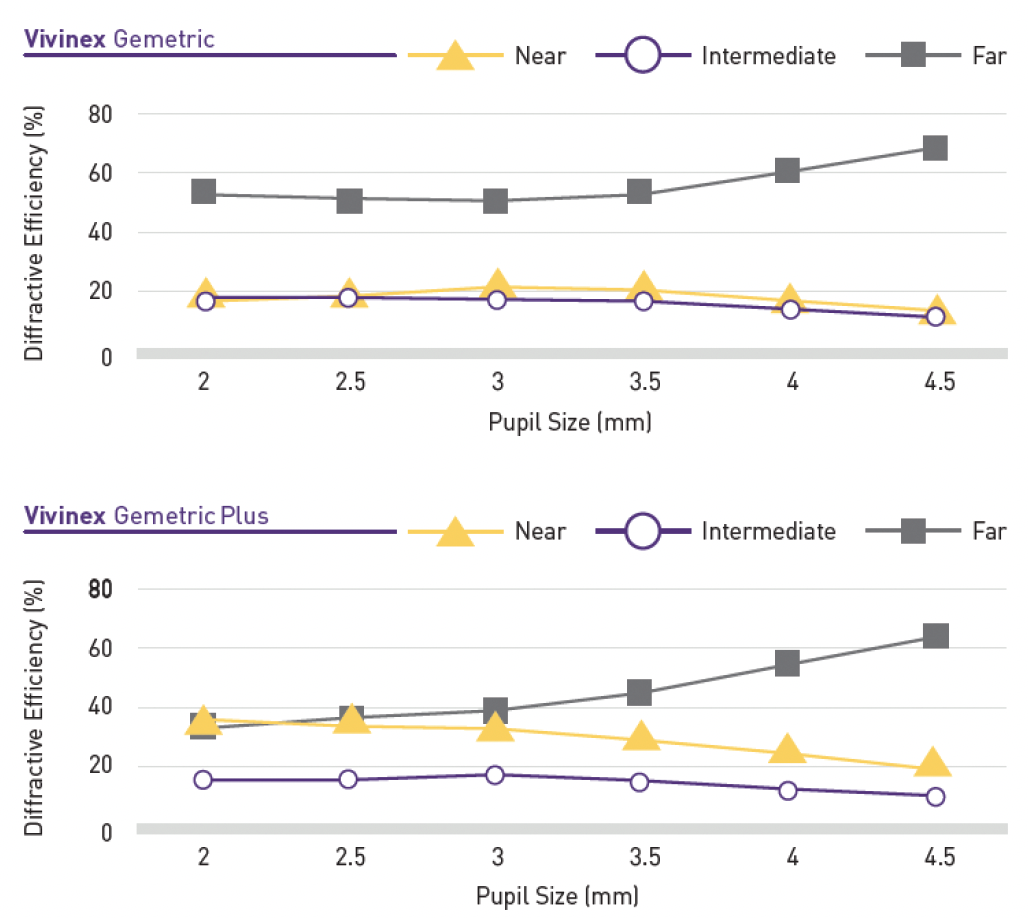
Figure 3. The light distribution profiles of the Vivinex Gemetric and Vivinex Gemetric Plus IOLs.1
Figure 4 shows results are based on final 4- to 6-month data from a randomized trial comparing the three bilateral combinations of Gemetric Trifocal IOLs (T0 to T5). Patients were grouped into three categories: those who received bilateral Vivinex Gemetric IOLs, those who received bilateral Vivinex Gemetric Plus IOLs, and those who received the Vivinex Gemetric in one eye and the Vivinex Gemetric Plus in the other eye (ie, paired group).
Across all groups, the mean visual acuity was better than 0.15 logMAR from distance to 30 cm near (defocus -3.50 D).
While the bilateral Vivinex Gemetric group showed about 0.3 lines better distance acuity than the bilateral Gemetric Plus group (-0.08 vs -0.05 logMAR, respectively), the bilateral Gemetric Plus group showed 0.5 lines better near acuity at -2.50 D compared to the bilateral Gemetric group (0.01 vs 0.06 logMAR, respectively).
The near acuity in the paired Vivinex Gemetric/Gemetric Plus group exactly mirrored the full benefit of the bilateral Gemetric Plus group, but these patients also achieved a boost in distance and intermediate acuity (Figure 4). This suggests pairing the two models may maximize benefits for patients.1
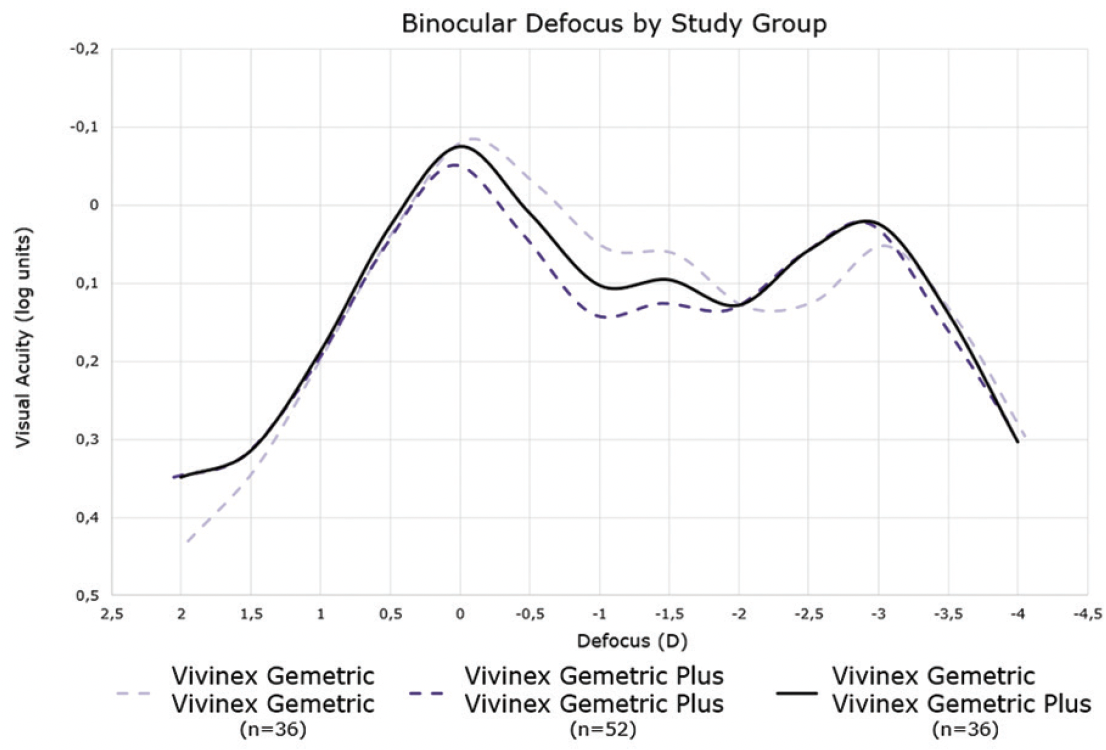
Figure 4. The 4- to 6-month results in patients who received bilateral Vivinex Gemetric IOLs, bilateral Vivinex Gemetric Plus IOLs, or the Vivinex Gemetric in one eye and the Vivinex Gemetric Plus in the other.1
IROF VERSUS FROF IOLS
Dr. Carones: Are IROF IOLs a viable alternative to using a bilateral FROF IOL in patients who demand spectacle independence?
Dr. Khoramnia: With an IROF IOL, oftentimes reading glasses have to be accepted by the patient. If you miss the target, then you will also not get a good result. Whenever I have a patient who asks for the maximum spectacle independence, I always go for a FROF IOL, but the patient has to accept the side effects.
Dr. Mertens: IROF IOLs cause side effects, too, and they decrease stereopsis. I do not understand why anyone would choose that option when implanting a FROF IOL in both eyes results in good vision at distance, intermediate, and near.
Dr. Carones: It could be a viable alternative in patients who would not do well with a diffractive technology, like glaucoma patients for instance. Otherwise, I agree that the optimal choice is a FROF IOL.
Dr. Muhtaseb: IROF IOLs might also be suitable for post-LASIK patients who have no surgical history—they don’t know if they were hyperopic or myopic, and their corneal topography is in the middle. It could also be an option for patients with drusen or small partial thickness macular holes. It won’t provide the same vision as a FROF IOL, but it is a viable option.
Dr. Rozot: It depends on the psychology of the patient. Patients must be counseled about the vision they can expect to have with certain IOLs. I like to ask them, “What do you want after surgery?” When their answer is to be free from glasses, I hammer home that a FROF IOL will provide them with spectacle independence but at the cost of some halos and glare. One of my staff members has a FROF IOL, so I usually ask them to talk to patients about the technology. That has been convincing. If patients express intolerance of visual disturbances such as halos and glare, I will implant a monofocal IOL. I do not like to give my patients too many options because they can experience choice paralysis.
Dr. Mertens: Managing expectations and informed consent are both key. In my experience, patients respect your confidence level, and I am confident that I can give patients spectacle independence with a FROF IOL. When you tell them they will be spectacle independent for most if not all tasks, they feel confident in their decision.
Dr. Carones: One thing I would like to know is do you talk about the neural adaptation process with your patients ahead of surgery?
Dr. Mertens: About 90% of patients adapt to their new visual system perfectly fine. I tell patients that 90% of patients who see halos at 1 month adapt by 3 months. I think it’s just a matter of how you set expectations.
CONCLUSION
Dr. Carones: IOL selection can be a daunting task, but the key lies within proper preoperative examinations, patient education, and counseling. We have many great lens technologies to consider, and the clear choice for achieving the greatest likelihood of spectacle independence is a FROF IOL.
Our collective early experience with the Vivinex Gemetric IOL indicates that the lens is poised to be among the leading IOLs in this category by offering two complementary profiles to meet the individual spectacle independence needs of patients.
1. Data on file. DoF-MKT-22-09, HOYA Surgical Optics. 2022.
2. Study Report, University Hospital Heidelberg. Vivinex Impress. Report on file. September 2022.
023-03-15_HSOE_XY1-G_XY1-GT_XY1_GP_XY1-GPT_XY1-EM_SUPP_EN
HOYA, Vivinex, Gemetric, Vivinex Impress, and multiSert are trademarks of the HOYA Corporation or its affiliates.
©2023 HOYA Surgical Optics GmbH All rights reserved.
hoyasurgicaloptics.com















