Determining what postsurgical analyses are important and how to apply them in a clinical setting can be a confusing task. Some surgeons may think, “My patients are happy with their vision, so I do not need to look at my outcomes any further.” Certain preoperative practices may be common—for example, adding or subtracting 0.25 D from the spherical or astigmatic treatment in refractive surgery, targeting non-0.00 D outcomes, or averaging corneal astigmatism measurements before toric IOL implantation or limbal relaxing incision (LRI) creation—but it is of equal importance to keep track of the results postoperatively.
AT A GLANCE
• Outcomes analyses should be performed at the corneal plane and on data collected at least 1 month postoperatively.
• Aggregate analyses for nomogram adjustments should be done on at least 50 cases and should be ongoing as more cases are added to the analysis group.
• A basic astigmatism analysis should include TIA, SIA, DV, and CI polar plots with arithmetic and vector means.
Analyzing surgical outcomes using a systematic approach can lead to validated physician adjustments, which can have multiple variables. In this way, future treatments can be planned with certainty using retrospective analyses of one’s own data.
The basics of any surgical analysis indicate whether the actual target was achieved and how far and in what direction the outcome was from the intended target. All outcomes analyses should be done at the corneal plane for consistency of corneal versus refractive parameters.1
LASER REFRACTIVE SURGERY
Spherical analyses. When spherical outcomes of excimer laser surgery are analyzed, procedures with only a spherical treatment should be grouped. In this way, there is no astigmatic influence on the outcomes, and a consistent treatment baseline can be quantified. If, in Case No. 1, a spherical refractive correction was applied at the corneal plane with the aim of a 0.00 D refractive target, postoperative analysis asks: Was a 0.00 D spherical component achieved postoperatively? This calculation is straightforward and linear, as anything less than 0.00 D is an undercorrection and anything more than 0.00 D is an overcorrection of the sphere.
CASE No. 1
If a -5.50 D of sphere treatment at the corneal plane achieves 1.50 D postoperatively, then there has been a 27% spherical overcorrection (spherical correction index = achieved spherical treatment/planned spherical treatment = 7.00 D/5.50 D = 1.27). Thus, if a retreatment for overcorrection in the same eye is required, the treatment would be scaled back by 27%, assuming the eye will behave in the same manner.
A retrospective aggregate analysis to identify trends can then be used to adjust spherical nomograms by inverting the spherical correction index. It is important to remember to exclude or adjust for any cases in which a monovision strategy was used, targeting a non-0.00 D result, as this will skew the analysis.
Astigmatic analyses. Because astigmatism has a magnitude and an orientation, vectorial calculations are required to determine the success of any surgery treating astigmatism. This requires the use of double-angle vector diagrams (DAVD), which allow trigonometric calculations in a Cartesian plane. In a DAVD, the axes of the astigmatisms are doubled, but the magnitudes remain the same. Once the calculations have been performed, the axes are then halved and displayed on a polar 0° to 180° diagram to simulate how they appear on the eye.1,2
The astigmatism intended to be treated is the target induced astigmatism vector (TIA). This is the amount of astigmatism that can be realistically reduced with surgery, not what you hope to reduce. If the surgery can correct only 2.00 D of astigmatism, then that is the TIA. For example, LRIs can correct up to approximately 2.00 D of astigmatism. If you plan to reduce 4.00 D (TIA) with LRIs, then the analyses will be inaccurate, as this is not achievable; realistically, the target is approximately 2.00 D for the analyses, and therefore 2.00 D likely is the best possible result.
Corneal astigmatism cannot be fully corrected with stock toric IOLs, as toric IOL powers are available in steps of 0.50 or 0.75 D, unless the lens is customizable. For stock toric IOLs, therefore, the target in most cases is not 0.00 D, and any astigmatic analysis should be based on this reality.3 The surgically induced astigmatism vector (SIA) is the vectorial difference (taking into account the direction) between the postoperative and preoperative astigmatism. The SIA can be for corneal or refractive values and, in the case of toric IOLs, may be a hybrid of the two.
Comparison of the TIA and SIA reveals whether the astigmatism was over- or undercorrected. This value, known as the correction index (CI), should ideally be 1, as values greater than 1 indicate an overcorrection of astigmatism and those under 1 indicate an undercorrection. The inverse of the CI (TIA/SIA) is the coefficient of adjustment and represents the nomogram adjustment required.1,4 The difference vector (DV) is the amount of astigmatism remaining at the end of the procedure, and, if the target is 0.00 D, this value is the same as the postoperative astigmatism. A summated vector mean of the DVs in a group of eyes can be used to examine an overall trend for error.1,4
Understanding Astigmatism
An easy way to understand astigmatism analysis is to use a golf analogy.1 Think of a golf ball on a putting green (Figure 1). The initial state of the ball on the green is the preoperative astigmatism at the corneal plane, and the target is the hole. The TIA is the intended astigmatic treatment of the procedure. The SIA is the actual path the surgery took after the first putt. The DV is the second putt required to place the ball in the hole. Figure 1 displays a non-0.00 D target, as in scenarios in which a stock toric IOL does not completely neutralize the corneal astigmatism or large amounts of astigmatism are present and the treatment cannot achieve sphericity. If the surgery goes exactly as planned, the postoperative astigmatism will not be 0.00 D because this was not the intention of the surgery. Hence, the hole is not at the origin. If the planned astigmatism treatment were targeting 0.00 D, then the hole would be at the origin of the axes.
The putting green is displayed as a DAVD (Figure 2) to allow the TIA, SIA, and DV vectors to be calculated using basic trigonometry. This can then be applied clinically by halving the angles of all the vectors and astigmatisms that have been calculated. We use the ASSORT software (ASSORT Surgical Management Systems) for these calculations. The TIA allows integrated analysis to be performed by any modality of astigmatism measurement, so we can ascertain the success of the astigmatic treatment using refractive (manifest or wavefront) and corneal (corneal topographic astigmatism [CorT]2 or simulated or manual keratometry) parameters.
1. Croes K. The Alpins Method: A Breakthrough in Astigmatism Analysis. Medical Electronics. September 1998.
2. Alpins N, Ong JKY, Stamatelatos G. New method of quantifying corneal topographic astigmatism that corresponds with manifest refractive cylinder. J Cataract Refract Surg. 2012; 38(11):1978-1988.
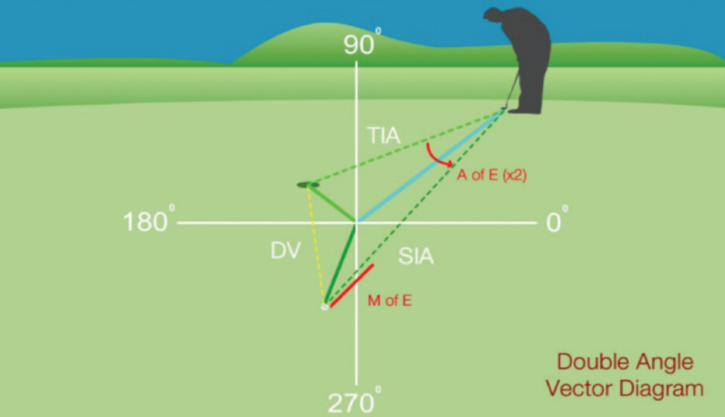
Figure 1. Astigmatism analysis as an analogy to putting in golf. The TIA is the intended treatment (putt), the SIA is the actual treatment, and the DV is the second treatment (putt) needed to achieve the initial astigmatic target.
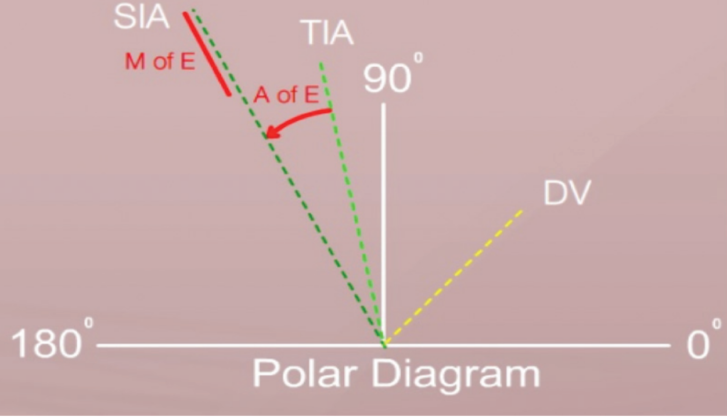
Figure 2. Surgical vectors TIA, SIA, and DV, as they would appear on an eye.
The angle of error (AE) is the angular difference between the SIA and the TIA in degrees. It is positive for a counter-clockwise direction and negative for clockwise. The mean AE should be consistent with the difference of the SIA and TIA vector means.1,4 If the AE is significant in a group analysis of excimer laser refractive surgery, then the systems used for alignment of the patient’s head during wavefront acquisition and treatment should be examined, and technical support for appropriate rotation of the laser beam is advised. With incisional surgery, a significant mean arithmetic AE suggests improvement is needed in the alignment of the treatment with limbal marking or iris registration. The absolute value of the AE provides a guide to the magnitude of the problem.
INCISIONAL SURGERY
Procedures involving incisions, such as cataract surgery, LRIs, and astigmatic keratotomy, predominantly affect or correct corneal astigmatism. The astigmatic outcomes of incisional surgery can be effectively analyzed using parameters such as AE, flattening effect (FE), and SIA.
In these types of surgery, any spherical change would be due to the incisions, so a spherical equivalent analysis would be expected to show no change between preoperative and postoperative. We associate this with corneal coupling, which describes the influence of any astigmatic correction on the corneal sphere. With corneal incisions, there is 100% coupling—that is, the effect of the incision at the treatment meridian is the same in magnitude but opposite in effect 90° away (see the section Corneal Coupling below).
CASE No. 2
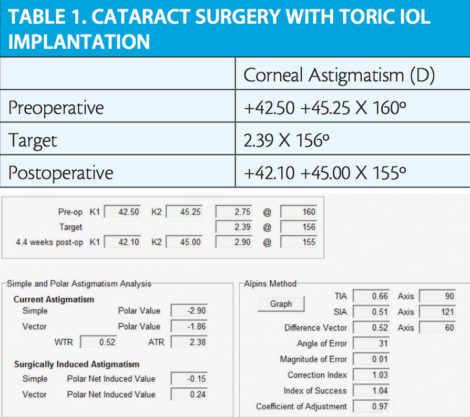
Figure 1. Astigmatism analysis of a primary phaco incision in cataract surgery.
REFRACTIVE ASTIGMATIC SURPRISES
Refractive surprises after toric IOL implantation can occur for several reasons.3 It is important to perform astigmatic analysis to gauge what can be done to correct for unexpected refractive cylinder postoperatively.
Our first approach with refractive astigmatic surprises is to measure the corneal astigmatism postoperatively and determine if the phaco incision behaved as planned. If the postoperative corneal astigmatism is significantly different in magnitude and/or orientation from what was planned preoperatively, we must determine why the incision behaved in an unexpected manner—ie, perhaps more corneal fibers than usual were torn during IOL insertion. In Case No. 2 (Table 1 and Figure 1), the target corneal astigmatism achieved (2.90 X 155°) as a result of the phaco incision (0.66 D placed at 180°; hence the TIA is 90° away) was close to the expected result (2.39 X 156°). Figure 1 displays the astigmatic analysis with a CI of 1.03 and a magnitude of error (ME) of 0.01 D, using the ASSORT Toric IOL Calculator (ASSORT Surgical Management Systems; www.assort.com). Hence, any refractive astigmatism surprise as a result of the incision is removed from the equation.
Toric IOL refractive surprises. The ASSORT software can be used to analyze and address refractive surprises. To calculate the minimum refractive cylinder after toric IOL rotation, the axial length and surgeon-personalized IOL constants are used. This is invaluable, as a postoperative refractive surprise can occur despite the toric IOL being aligned exactly as planned. I (author NA) examine all of my cataract surgeries on postoperative days 1 and 9. If I find a refractive astigmatic surprise at the 9-day visit, and the toric calculator indicates that rotation would significantly improve the refractive outcome, I plan to rotate the IOL within 4 weeks of the initial procedure to avoid restriction of rotation of the IOL by the lens capsule.
The astigmatic effect of misalignment of toric IOLs has been overstated in many articles.5,6 The relationship between misalignment of the IOL and reduction of astigmatic effect is sigmoidal and trigonometric, not linear. By vectorial calculation, a 15° axis misalignment causes a 13.4% loss of effect (SIA cos 2 X AE), not 45% as commonly stated. The frequently cited loss of 3% of correction for every 1° of misalignment is only a scalar comparison of astigmatism magnitudes postoperatively versus preoperatively, which, for toric IOLs, is postoperative cylinder versus preoperative corneal astigmatism.
It is important to note in what context this is being stated. There is limited analytical value in comparing postoperative and preoperative astigmatism, apart from observing whether the astigmatism has decreased and by how much.
Using the ASSORT Toric IOL Calculator, when there has been a 1.50 D refractive astigmatic surprise, the angle of rotation may reduce the refractive astigmatism by 0.25 or 0.50 D, in which case one must look at the ME. This will indicate whether a correctly toric-powered IOL has been implanted. If the ME is 0.75 D or greater, then the toric IOL implanted was not optimal, and an IOL exchange or excimer laser corneal surgery is warranted to correct for the surprise. If the IOL is exchanged, then the appropriate IOL can be determined using the toric IOL calculator.3
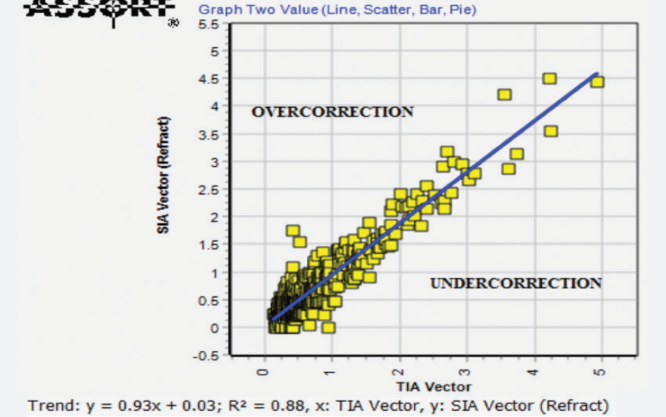
Figure 2. Achieved (SIA) versus attempted (TIA) scatterplot with trend line.
AGGREGATE ASTIGMATIC ANALYSES
The analysis of astigmatism involves just two key parameters: (1) Was the astigmatism over- or undercorrected, and (2) was it in- or off-line compared with the planned treatment?
Simple subtraction analysis. Astigmatism analysis in its most basic form is a comparison between the postoperative and preoperative magnitudes of astigmatism without reference to axis or meridian. This simple subtraction determines that an increase (positive value) or a decrease (negative value) in the existing astigmatism of the eye has resulted from surgery.
Vectorial analysis. Systematic laser or surgical technique errors can be revealed by aggregate analysis. Two types of analysis are relevant: (1) arithmetic means of the astigmatism magnitude without consideration of the orientation and (2) summated vector mean incorporating magnitude and orientation. The greater the difference between the two, the less indication of any overall trend and the more likely that any changes occurred due to random events.
AGGREGRATE ANALYSIS REPORTS
Laser refractive surgery. Scatterplots of SIA versus TIA are common in the literature and easy to understand (Figure 2): Above the unity line is an overcorrection, and below is an undercorrection.7 An AE frequency graph, displayed at intervals of 10°, clearly shows any trend of off-axis treatments.7
Surgical vector diagrams show TIA, SIA, DV, and CI vectors or geometric means. Figure 3 displays the calculated index values at their meridian of treatment (the axis of the TIA) to determine trends of surgical performance. The geometric mean of 0.89 indicates that the astigmatic treatments for the group analyzed was undercorrected by 11%. Outliers are also easily identifiable, and we recommend verifying that correct data were entered (ie, there was no reversal of flat or steep meridian on data entry).7
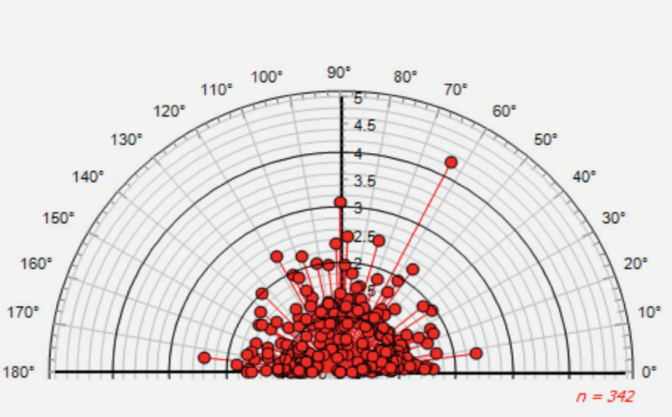
Figure 3. Surgical vector diagram of the correction index; geometric mean = 0.89.
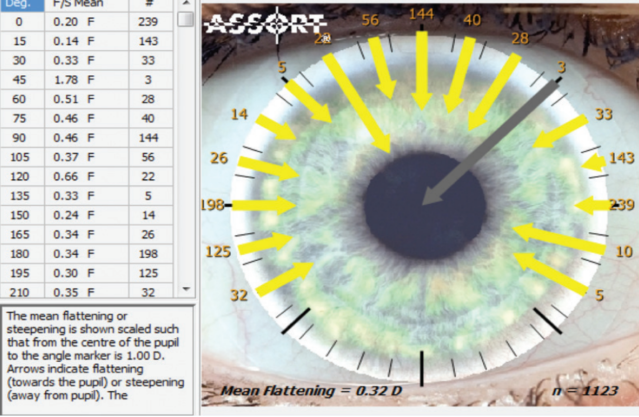
Figure 4. Flattening effect of phaco incisions by corneal parameters for left and right eyes.
Incisional procedures. Mean flattening and steepening can be calculated from the individual effect of each cataract procedure, as shown in Figure 4. The arrows pointing toward the pupil center indicate flattening of the cornea, with the grey arrow being outside the scale of 0.00 to 1.00 D. This display of incisional surgery relates to right and left eyes, with the numbers around the limbus indicating the number of procedures performed at those meridia.
The phaco incision can be moved around the eye in each case to operate at the steepest corneal meridian, thus using the primary phaco incision to reduce some of the corneal astigmatism at the time of cataract surgery. The amount of flattening or steepening caused by incisions at the intended meridian should be calculated, as this is one of two components of the SIA—not the total SIA, unless the AE is 0.
Note that the amount of flattening is greater when the incision is placed vertically (toward 90°) versus horizontally (180°). This is because vertical incisions are closer to the center of the cornea and thus have more effect.
CORNEAL COUPLING
Corneal coupling should be analyzed to determine the effect of an astigmatic treatment on the spherical component. This is known as coupling adjustment.8
For ablations. The expectation with ablations is that flattening at the treatment meridian will result in no effect at the meridian 90° away. Hence, there is a change in spherical equivalent and a coupling ratio of 0%. When assessing the coupling adjustment clinically, we first determine the effect of any spherical treatment and remove this from our calculations to determine purely the effect of the astigmatic component. Any nomogram adjustments are based on aggregate analyses, so that, if a coupling adjustment of 0.30 is reported, then the magnitude of the cylinder is multiplied by 0.30 and the spherical treatment is reduced by this amount. If the coupling adjustment is negative, then the spherical treatment is increased. (A coupling calculator is available at www.assort.com.)
For incisions. The expectation with arcuate incisions is that flattening at the treatment meridian will lead to an equal amount of steepening 90° away. Thus, the spherical equivalent is unchanged, and the coupling ratio is 100%. If aggregate analysis shows any spherical effect, then the type of incision used should be carefully considered; a straight or tangential incision will produce a hyperopic shift, as there is a radial component to the incision.
SUMMARY
Outcomes analyses should be performed at the corneal plane and on data collected at least 1 month postoperatively. Aggregate analyses for nomogram adjustments should be done on at least 50 cases and should be ongoing as more cases are added to the analysis group. Nomograms should be adjusted any time new equipment or new techniques are adopted. A parallel astigmatic analysis using both refractive and objective corneal parameters is recommended. A basic astigmatism analysis should include TIA, SIA, DV, and CI polar plots together with arithmetic and vector means.
1. Alpins NA. Astigmatism analysis by the Alpins method. J Cataract Refract Surg. 2001;27:31-49.
2. Alpins NA. New method of targeting vectors to treat astigmatism. J Cataract Refract Surg. 1997;23(1):65-75.
3. Alpins N, Ong JKY, Stamatelatos G. Refractive surprise after toric intraocular lens implantation: graph analysis. J Cataract Refract Surg. 2014;40(2):283-294.
4. Alpins NA. A new method of analyzing vectors for changes in astigmatism. J Cataract Refract Surg. 1993;19:524-533.
5. Optoelectronic test bench shows effect of toric IOL rotation on image quality. Ocular Surgery News. February 19, 2014. http://www.healio.com/ophthalmology/cataract-surgery/news/online/%7B941221bb-c41d-4a9b-b6ed-63441a58fa10%7D/optoelectronic-test-bench-shows-effect-of-toric-iol-rotation-on-image-quality. Accessed January 20, 2015.
6. Roach L. Toric IOLs: Four Options for Addressing Residual Astigmatism. EyeNet. April 2012. http://www.aao.org/publications/eyenet/201204/cataract.cfm. Accessed January 29, 2015.
7. Reinstein DZ, Archer TJ, Randleman JB. JRS Standard for Reporting Astigmatism Outcomes of Refractive Surgery. J Refract Surg. 2014;30:654-659.
8. Alpins N, Ong JKY, Stamatelatos G. Corneal coupling of astigmatism applied to incisional and ablative surgery. J Cataract Refract Surg. 2014;40:1813-1827.
Noel Alpins, FRANZCO, FRCOphth, FACS
– Medical Director, NewVision Clinics, Melbourne, Australia
– CEO, ASSORT Surgical Management Systems
– alpins@newvisionclinics.com.au
– Financial disclosure: Employed by company (ASSORT Surgical Management Systems)
George Stamatelatos, BSc Optom
– Senior Optometrist, NewVision Clinics, Melbourne, Australia
– george@newvisionclinics.com.au
– Financial disclosure: Employed by company (ASSORT Surgical Management Systems)
