In September 2022, a group of eye care providers gathered at the 18th International Myopia Conference (IMC) in Rotterdam, the Netherlands, to discuss the latest innovations and research on myopia management. Select presentations from the Topcon Healthcare symposium at the IMC have been chosen for summarization.
In the first installment of this series, Prof. Joan Pérez-Corral reviews his approach to orthokeratology fittings and discusses how MYAH (Topcon Healthcare) helps guide his treatment approaches. A video of his presentation can be found by scanning the QR code on the next page. Look forward to other installments updating readers about the findings discussed at the 18th IMC throughout 2023.
When considering orthokeratology for myopia control in a pediatric patient, there are seven questions I always consider. I will break down each of them here, sometimes using real-world patient cases to illustrate my point.
1. Is Orthokeratology the Right Approach for This Patient?
Not all pediatric patients in need of myopia control are good candidates for orthokeratology. In my practice, I use MYAH to assess a patient’s overall keratometry and eccentricities to determine whether they are a fit for orthokeratology treatment. In patients with normal corneal anatomy, orthokeratology can be considered if topography and pachymetry evaluations are also within the parameters for safe orthokeratology intervention (Figure 1). In patients with extremely irregular corneal anatomy (eg, possible presence of keratoconus), orthokeratology for myopia control is not advised (Figure 2).
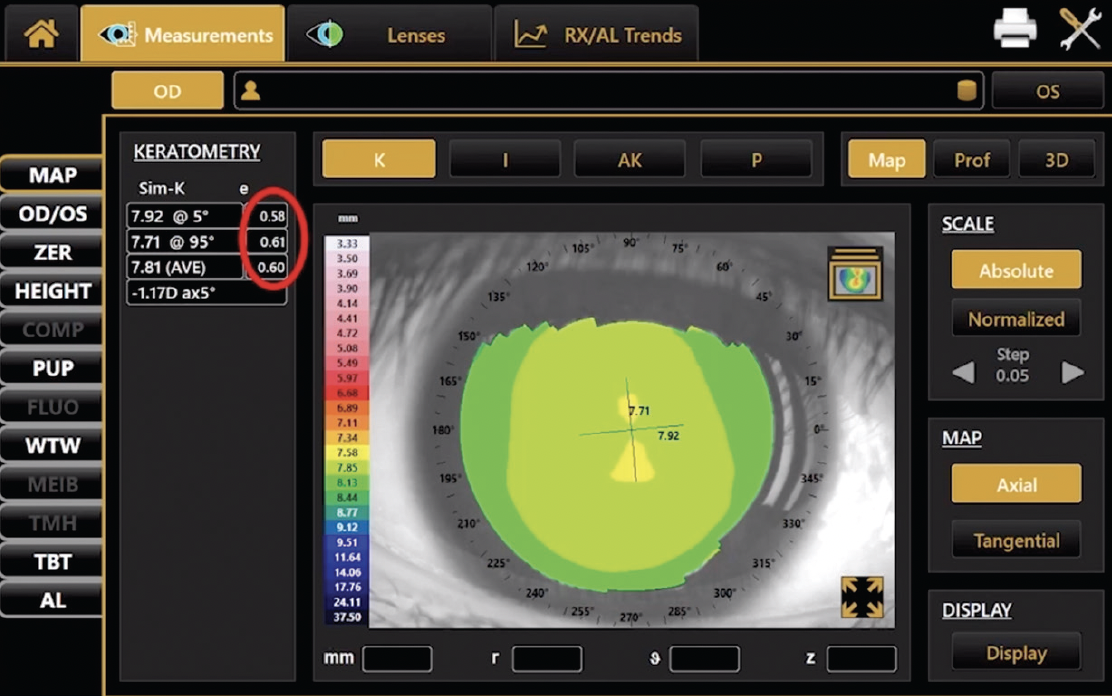
Figure 1. This patient’s normal keratometry, despite high eccentricity values as depicted in the red circle, suggest that orthokeratology may be a therapeutic option for myopia control.
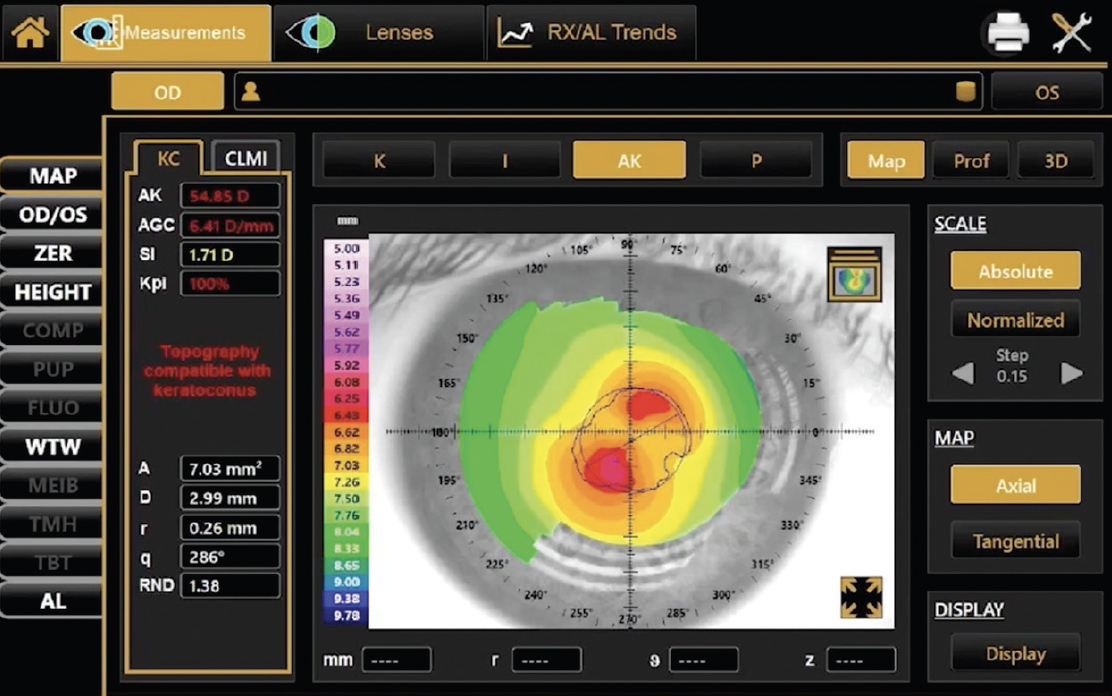
Figure 2. Given this patient’s irregular corneal anatomy, orthokeratology may not be advised. Red text on the MYAH interface suggests that, given this patient’s presentation, keratoconus may be present.
2. Is a Spherical or Toric Lens Needed?
In orthokeratology, we must prioritize the edge of the lens landing on the periphery of the cornea. If corneal peripheral astigmatism is higher than 1.25 D to 1.50 D, a toric lens will be needed. Although clinicians are sometimes able to calculate by hand whether peripheral corneal toricity is greater than central corneal toricity, reliance on modern technology will deliver more exact measurements and save time.
MYAH provides detailed and precise elevation maps that calculate whether a typical orthokeratology contact lens with a central optic zone diameter of 6 mm will fit a patient. If a patient needs a specialty toric lens, MYAH’s measurements of their corneal toricity may inform the specific design of such a lens.
3. What is the Risk of Decentration?
Patients who require fitted lenses may be at risk of lens decentration if they have a corneal shape that allows a lens to shift to a region of depressed cornea. MYAH provides profiles of elevation maps, which are particularly useful at depicting whether a lens will decentrate and, if so, in what direction (Figure 3). I use such data when calculating lens decentration risk, as this information has, in my experience, made my prognoses of directional shift more accurate.
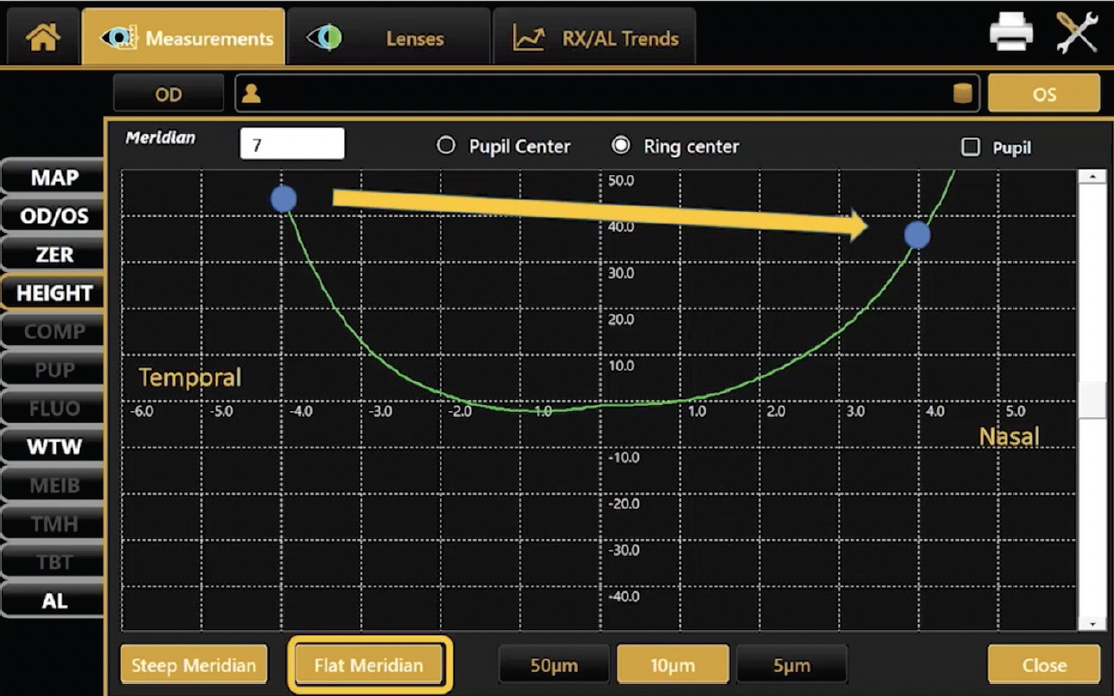
Figure 3. Profiles of patient elevation maps help providers calculate risk of decentration.
4. Will the Orthokeratology Lens Cover Enough Cornea?
Orthokeratology lenses must cover 90% to 95% of the cornea, so ensuring a correct measurement of corneal diameter is key to success. While topographers are generally accurate in measuring corneal diameter, some platforms have difficulty differentiating the border between the limbus and the cornea in patients with blue or green eyes. MYAH’s software and interface accounts for this challenge, increasing my confidence that corneal diameter measurements are accurate in all patients.
5. Will the Optical Treated Zone Cover the Pupil in Variously Lit Environments?
Assessments using MYAH deliver pupil diameters in scotopic, mesopic, and photopic conditions. We must ensure that adult patients’ pupils are covered by the optical treated zone of an orthokeratology lens in all lit environments. In pediatric patients, pupil diameter in mesopic and photopic conditions is also important, as we need to ensure that the treated optical zone still aligns with the pupil after its diameter changes or if it becomes decentered.
6. Do Baseline and Follow-Up Axial Length Measurements Indicate That Treatment is Working?
Axial length measurements can be used to assess the efficacy of orthokeratology for myopia control. MYAH captures baseline axial length data as well as measurements from each visit and depicts those data on a line chart that illustrates all longitudinal data points. Clinicians need to compare the axial length measurements during the course of treatment with on-board growth curves, which will inform whether a new treatment strategy is needed.
Watch it Now
Joan Pérez-Corral, DO, PhD, FIAOMC, shares insights into orthokeratology lens fitting with topography and biometry as part of the 18th International Myopia Conference. Prof. Pérez-Corral highlights the advantages of MYAH (Topcon Healthcare) and outlines seven important considerations for orthokeratology for myopia control.
7. How Can I Best Ensure My Patients Will Use Proper Follow-Up Protocols?
Our efforts as clinicians are limited if pediatric patients and their parents are not compliant with the prescribed treatment. Educating parents about their child’s axial length relative to other children their age can be key to driving home the point that intervention is required. Parents commonly see age-based height and weight graphs for their children in primary care settings. MYAH allows providers to print similar charts for parents depicting typical axial length growth with age. Pointing out where a patient ought to appear on the growth curves and where the patient actually appears on the graph is sufficient for most parents to know that intervention is needed and that follow-up is necessary.
CONCLUSION
Pediatric orthokeratology challenges even the most experienced providers, and clinicians need all the help they can get. Rely on technology such as MYAH to more closely customize therapy and maximize facetime with patients.
Not all products, services or offers are approved or offered in every market, and products vary from one country to another. Contact your local distributor for country-specific information and availability.


