The precise placement of any toric IOL is important. For every degree of misalignment, about 3% of the lens’ cylindrical power is lost. A seemingly small rotational error of 3º can cause nearly a 10% loss of cylindrical effect. Luckily today, the art of toric IOL alignment has evolved, and now several tools can help us to further improve postoperative outcomes and fine-tune our surgical processes. Aligning the toric EVO Visian ICL (STAAR Surgical) in the posterior chamber is just as crucial to the final postoperative outcome as toric IOL alignment in the anterior chamber is. The lens is designed with the cylinder component placed within the optic in such a fashion as to allow the long axis of the EVO lens to remain implanted as close to horizontal (0–180º meridian) as possible. Based on the specific EVO/ICL lens ordered, the maximum rotation at the time of implantation will not exceed 22º from the 0º to 180º meridian. There are inherent properties built into the toric EVO Visian ICL that can aid in the alignment process, including two extended toric alignment markings etched onto the optic of the lens (Figure 1).
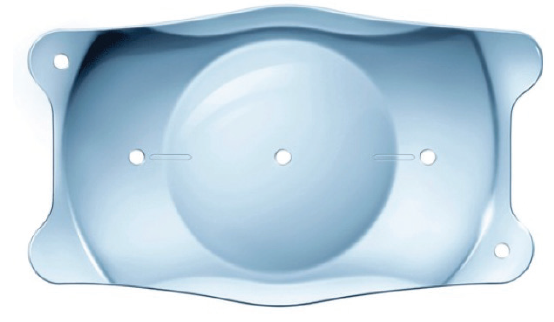
Figure 1. The toric EVO Visian ICL has inherent properties to aid in lens alignment to the 180º meridian.
OBSERVATIONAL CASE SERIES
My colleagues and I recently performed a prospective observational case series on 51 eyes of 51 patients to determine the stability of the toric EVO Visian ICL. The average age of patients was 27 ±4.7 years (range, 19–38 years*), and the average refractive sphere, cylinder, and mean refractive spherical equivalent (MRSE) was -8.07 ±2.22 D (range, -14.87 to -4.50 D), -2.21 ±0.88 D (range, -4.63 to -0.87 D), and -9.18 ±2.39 D (range, -16.31 to -5.12 D), respectively. The mean flat and steep keratometric (K) values were 42.30 ±1.30 D (range, 39.50–45.00 D) and 44.50 ±1.50 D (range, 41.40–48.80 D), respectively. The average anterior chamber depth was 3.34 ±0.26 mm (range, 2.86–4.00 mm*), the average white-to-white was 11.56 ±0.30 mm (range, 10.51 ±12.42 mm), and the average sulcus-to-sulcus was 11.83 ±0.36 mm (range, 10.97–12.55 mm).
We used the 12.1 mm toric EVO Visian ICL in 11 eyes, the 12.6 mm in 37 eyes, and the 13.2 mm in four eyes. In all cases, manual markings were applied with a marker at the slit lamp, and up to 22º of rotation for the proper toric ICL alignment was allowed. This was determined by the toric EVO ICL implant orientation form (Figure 2).
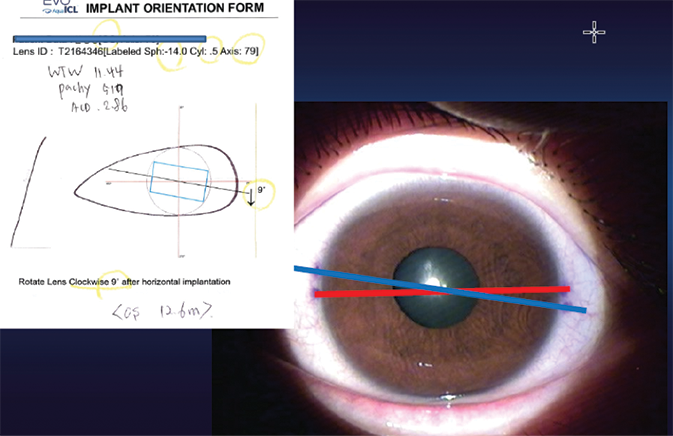
Figure 2. The implant orientation form, which helps the surgeon to properly align the toric EVO Visian ICL in the posterior chamber.
RESULTS
Assessments included 6-month follow-up in all eyes. Retroillumination imaging was used to determine toric lens alignment. Lens vault immediately postoperative and at 3 and 6 months is shown in Figure 3. Both postoperative vaulting and AQD/valuting significantly decreased in a time-dependent manner (P < .001). The results of a multiple regression analysis showed that there was no explanatory variable relevant to the absolute degree of rotation, including postoperative vault.
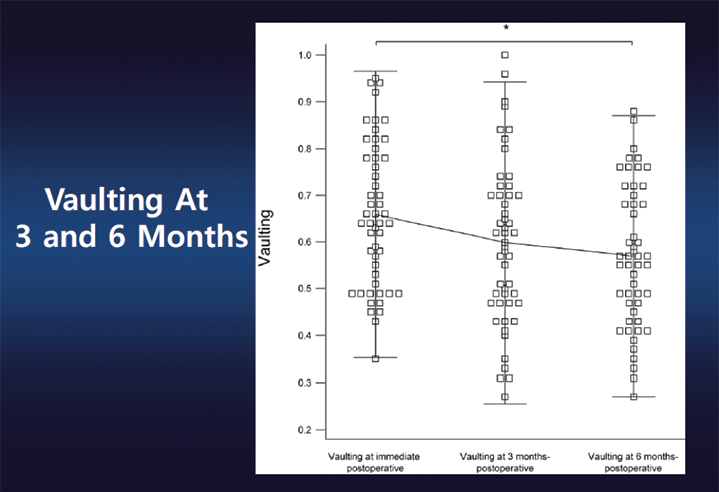
Figure 3. Vaulting of the EVO Visian ICL at 3 and 6 months postoperative.
At 6 months postoperative, 49% of the study population had a distance UCVA of ≥20/12.5, 86% of ≥20/16, 96% of ≥20/20, and 100% of ≥20/25. Also at this time point, 96% had gained at least 1 line of BCVA and 47% had gained at least 2 lines. No eyes lost any lines of BCVA.
When we looked at MRSE, 92% of eyes were within ±0.50 D of intended correction and 98% were within ±1.00 D. When we broke these numbers down more specifically, 98% were between -0.50 and 1.00 D of intended correction, 82% between -0.13 and 0.50 D, and 35% between 0.14 and 0.50 D. Furthermore, 90% of patients had no more than 0.50 D of refractive astigmatism at 6 months postoperative, and 98% had no more than 1.00 D. The majority of patients (59%) had no more than 0.25 D of refractive astigmatism at 6 months postoperative. Figure 4 details the tight spread of the changes in degrees in the angle of the toric EVO Visian ICL positioning from the actual insertion angle to the angles at immediately postoperative and 3 and 6 months postoperative. At our 6-month analysis, neither the lens rotation nor vaulting was associated with the intended angle of implantation; most of the rotations occurred immediately postoperative. Although the angle of the toric ICL showed no significant difference postoperatively (P = .166), the postoperative absolute degree of rotation showed a significant difference (P = .009). A post-hoc comparison demonstrated that the absolute degree of rotation at 3 and 6 months was significantly larger than that noted immediately postoperative (P = .043 vs P = .023, respectively). There was no significant difference between the absolute degree of rotation noted at 3 and 6 months postoperative.
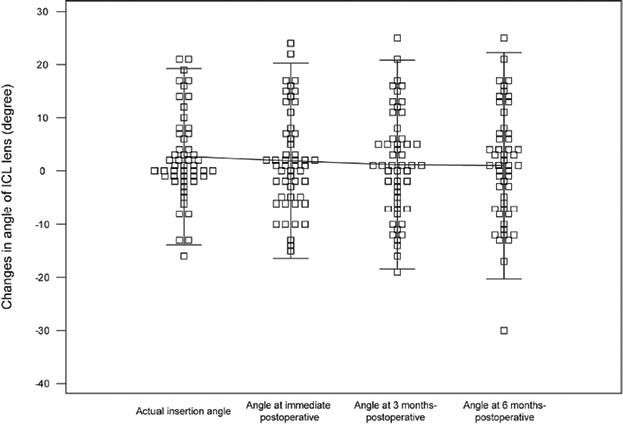
Figure 4. Changes (degrees) in angle of the Visian ICL lens.
We hypothesize that removal of the OVD and final lens positioning may be factors that contributed to rotation. From postoperative day 1 to postoperative month 6, the rotation of the toric EVO Visian ICL was negligible. The delta of the intended versus achieved angulation at 6 months postoperative was 2.79 ±1.83º. Therefore, the intended degree of rotation at implantation had no correlation with rotational stability. Further, rotational stability had no correlation with postoperative vault.
CONCLUSION
Our study indicated that implantation of the EVO Visian ICL, within 22º of the 0º to 180º meridian provides excellent visual results and rotational stability. We believe that this procedure is a safe, predictable, efficacious method of astigmatism correction in patients who are indicated for a phakic IOL. This option can provide patients with stable refractive outcomes, and it is our procedure of choice in the majority of our patients.

