CASE PRESENTATION
A 22-year-old White man with epilepsy is referred for a refractive surgery evaluation. The patient presents with high hyperopia, amblyopia in the right eye, and esotropia with right eye suppression. His left eye is dominant. He has a corrected distance visual acuity of 20/40 with a refraction of 11.50 D OD and 20/25 with a refraction of 12.25 D OS. Surprisingly, his cycloplegic refraction (12.25 D OD and 12.50 D OS) is not much higher than his manifest refraction. The patient’s uncorrected distance visual acuity is counting fingers OU.
The patient has worn spectacles since the age of 3 years but has no history of occlusion therapy and has never been assessed for strabismus surgery. He has no cosmetic concerns about the esotropia, and he states that he has never experienced diplopia. His spectacles are heavy, and he worries that they will break and possibly injure him in the event of an epileptic seizure. Repeated attempts at contact lens wear over the years have failed. In each instance, the thick lenses caused considerable ocular irritation, and the clarity of his vision fluctuated.

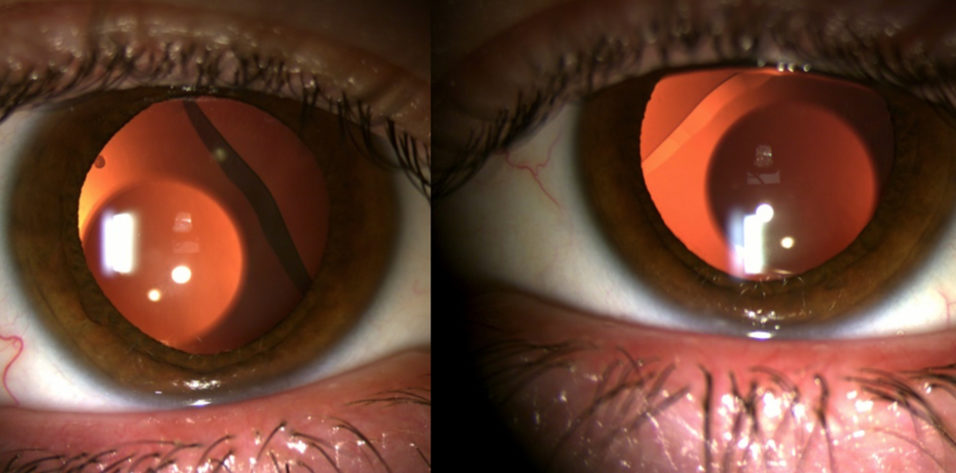
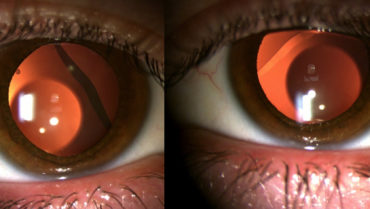
Figure 1. At the patient’s initial visit, imaging of his right (A) and left (B) eyes obtained with the Pentacam finds an anterior chamber depth of 2.79 mm and flat keratometry in each eye.

Figure 2. A-scan data show normal lens thickness. Axial length measurements, however, indicate a short eye, and extrapolated measurements indicate a relatively short posterior segment compared to the anterior segment.
Imaging with the Pentacam (Oculus Optikgeräte) shows crowding of the midperipheral anterior chamber and a depth of 2.79 mm OU (Figure 1). Diagnostic findings typically associated with posterior microphthalmos are absent. The axial length measured with the IOLMaster 700 (Carl Zeiss Meditec), however, is 20.44 mm OD and 20.19 mm OS. Lens thickness is within a normal range in each eye (Figure 2). Keratometry readings in each eye are flat (range, 39.00–40.00 D; Figure 1). The fundus of each eye has a normal appearance on clinical examination and OCT imaging with the Cirrus 6000 (Carl Zeiss Meditec), but the disc area (1.82 mm2) on OCT is below average in the right eye (Figures 3 and 4).

Figure 3. OCT nerve analysis shows relatively normal measurements for a short eye, but the disc area in the right eye is below average.

Figure 4. On OCT, the macula appears to be healthy, and papillomacular folds are not evident.
The patient’s vision concerns are negatively affecting his emotional well-being. He is unable to study or work comfortably. He loves to play Australian rules football but cannot participate safely owing to his contact lens intolerance, spectacle dependence, and poor UCVA. The patient is highly motivated to reduce his refractive error, but he has been advised several times that refractive surgery is not an option for him. He states that he would be happy to wear contact lenses and to wear less burdensome spectacles occasionally as needed after surgery.
How would you proceed?
—Case prepared by Abi Tenen, MBBS(Hons), FRANZCO

ARTHUR B. CUMMINGS, MB CHB, FCS(SA), MMED(OPHTH), FRCS(EDIN)
The easiest and arguably least risky approach is to advise the patient against refractive surgery. The amount of ametropia is too great for LASIK to correct, the anterior chamber is too shallow to permit the implantation of an EVO ICL (STAAR Surgical), and the patient is too young to be a suitable candidate for refractive lens exchange (RLE), a procedure I prefer to call custom lens replacement (CLR).
The patient, however, is part of a group of individuals who truly deserve a solution, for whom successful refractive surgery would have life-changing benefits, and who have real-world problems with glasses and contact lenses. I would like to help him however I can with a surgical solution to improve his quality of life.
Whatever form of surgical intervention is pursued, the patient will experience significant minification. He needs to experience this preoperatively—if only for a few minutes—with a contact lens trial. He must understand the compromises of losing significant magnification before proceeding to surgery.
As I see it, the patient has two options: (1) the implantation of phakic IOLs and (2) CLR.
The anterior chamber depth (ACD) is slightly less than ideal for the placement of a phakic IOL. The procedure is nevertheless likely to provide many years of improved vision before a reduction in ACD necessitates the removal of both the crystalline lens and the EVO ICL and their replacement with an IOL. Bioptics may be required to achieve emmetropia. The highest-powered ICL model would be implanted, and LASIK would be performed to correct the residual refractive error. The cornea is thick and flat enough to allow a LASIK correction of up to 6.00 D.
I typically would not offer CLR to someone his age. If, however, the patient prefers to move straight to CLR and IOLs, I would respect his wishes given his circumstances and the benefits he could enjoy.
Detailed informed consent is required. Surgery can be considered only once the patient is truly comfortable with the risk-benefit ratios and he has previewed his likely postoperative vision with a contact lens trial.

KARL G. STONECIPHER, MD
In 1991, Ionnis Pallikaris, MD, PhD, happened upon a poster I was presenting at the annual meeting of the Association for Research in Vision and Ophthalmology and later published.1 For me, a burgeoning ophthalmologist, it was a rare opportunity to speak with a true giant in ophthalmology without interruption. I asked him what to do with a patient who is hyperopic and desires refractive surgery. The only options at the time were hyperopic automated lamellar keratoplasty and hexagonal keratotomy, neither of which appealed to me as a new refractive surgeon.
Dr. Pallikaris said that he and Dimitrios Siganos, MD, PhD, had begun to perform a new procedure he termed clear lensectomy for patients with high hyperopia and that they were happy with the results.2 I thought their idea was brilliant and decided to try the procedure myself. Since that time, I have treated patients who have more than 3.00 D of hyperopia with RLE. The only exception occurred during my participation in US FDA clinical trials of LASIK for hyperopia and hyperopic astigmatism.
I published my 15- and 30-year results with RLE in this patient population.3,4 The key points I have learned about the procedure in this group are as follows.
No. 1: Unlike individuals with myopia, patients with hyperopia and hyperopic astigmatism rarely have retinal issues. That said, it is important to work with a strabismus surgeon to ensure that no issues arise postoperatively.
No. 2: Angle kappa and chord mu are issues, so the choice of IOL may be limited. I explain to patients that some of the latest trifocal IOLs may not be suitable for them.
No. 3: Classic pre- and intraoperative techniques for eyes with shallow anterior chambers and short (< 21 mm) axial lengths apply. Whether it is the use of an external Honan balloon or super pinkie rubber ball or the pharmacologic deturgescence of vitreous before surgery, using these tried-and-true measures is prudent.
No. 4: Like everyone else, these patients want great outcomes. There is a popular notion among surgeons that patients with hyperopia are more easygoing and forgiving than other patients, but I respectfully disagree. It is imperative to perform contact lens trials, to explain and compare the options of monovision and premium IOLs, and to discuss potential dysphotopsias before surgery.
I have found RLE in this patient population to be successful. With extended range of vision lenses available in powers as great as 34.00 D with up to 6.00 D of cylinder and monofocal IOLs available in powers as great as 40.00 D without toricity, surgeons’ ability to help patients with hyperopia and hyperopic astigmatism is greater than ever. If the surgical outcome is short of the mark, however, then a LASIK enhancement is an option.

OGER ZALDIVAR, MD, MBA
My first step would be to enhance the health of the ocular surface to improve the patient’s tolerance of contact lenses. Artificial tears, topical steroids, eyelid exfoliation, and intense pulsed light are some of my preferred approaches. If the effort is unsuccessful, I would proceed with surgery.
My first choice of intervention would be the implantation of a hyperopic ICL to treat the patient’s refractive error.5-7 The ACD in each eye is 2.79 mm, which is toward the lower limit of my comfort level for using an ICL, but the measured iridocorneal angles of each eye are appropriate. A small vault would be targeted, and a 12.6-mm ICL would be selected for each eye.
If an ICL is not elected, I would offer to perform phacoemulsification. Before surgery, I would discuss with the patient the expected loss of near vision, the risks of surgery, and the high likelihood that he will need a LASIK enhancement because of difficulties in accurately performing the IOL calculation.

WHAT I DID: ABI TENEN, MBBS(HONS), FRANZCO
The patient and his father traveled 5 hours to my office for a consultation.
The EVO ICL is approved in Australia for the treatment of hyperopia, but I deemed the central ACD of each eye to be too shallow for the surgical procedure (Figure 1). I was also disinclined to offer RLE because of the patient’s age and the risks associated with a small eye and a short posterior segment (Figure 2). Another factor in my decision to avoid intraocular surgery was the low appetite for risk demonstrated by the patient and his father, who attended the visit to support his son and assist with the decision-making process. Interestingly, the father was a police chief who was involved in the frontline response to the COVID-19 pandemic. I think that the timing of their visit (mid-2020) probably influenced their risk tolerance.
I offered to perform LASIK to reduce the patient’s refractive error but emphasized that he would require spectacles or contact lenses to achieve his best possible BCVA. We had already established that he was happy to wear spectacles and/or contact lenses after surgery if doing so were manageable. He completed a contact lens trial with a refraction of 5.00 D OU and reported being highly satisfied with his visual acuity despite significant residual ametropia. The patient also found the lighter contact lenses easy to tolerate, which was prognostically encouraging because the plan was for him to wear contact lenses after surgery to address his residual hyperopia.
LASIK was performed using the WaveLight FS200 femtosecond laser (Alcon) and the Amaris 1050RS excimer laser (Schwind eye-tech-solutions). One day after surgery, the patient’s UCVA was 20/100 OD and 20/80 OS. His corrected distance visual acuity was 20/32 with a refraction of 6.50 D OD and 20/20 with a refraction of 6.00 D OS. Spectacles had been made in advance with 6.00 D correction OU. The patient wore them successfully until he was ready for a contact lens fitting.
Nearly 2 years after surgery, the patient’s visual acuity is stable, and he is wearing soft contact lenses successfully. He is halfway through the coursework for his university degree, and he works part-time as an auto mechanic.
LASIK is a relatively low-risk procedure. In certain situations, such as the one presented here, it can be performed to improve the quality of life of patients typically considered to be unsuitable candidates by enabling them to wear contact lenses and spectacles.
I thank the panelists for their comments on this challenging case. My goal was to show that, in situations like this one, the decision on how to operate—let alone whether to operate—is not simple. There are various safe and effective ways, however, to achieve an outcome that is desirable to the patient, as demonstrated by the differing approaches presented in the article.
1. Stonecipher KG, Parmley VC, Rowsey JJ, Fowler WC, Nguyen H, Terry M. Refractive corneal surgery with the Draeger rotary microkeratome in human cadaver eyes. J Refract Corneal Surg. 1994;10(1):49-55.
2. Siganos DS, Pallikaris IG. Clear lensectomy and intraocular lens implantation for hyperopia from +7 to +14 diopters. J Refract Surg. 1998;14(2):105-113.
3. Stonecipher K, Polomsky M, Stonecipher M, Stonecipher K, Dunn K. Refractive lensectomy outcomes and complications for myopia and hyperopia: a 15-year retrospective study. Medical Research Archives. 2015;2(5). Accessed June 10, 2022. https://esmed.org/MRA/mra/article/view/422
4. Stonecipher KG. Refractive lensectomy outcomes after 30 years. Paper presented at: OSN New York 2020 Meeting; October 2020; New York.
5. Davidorf JM, Zaldivar R, Oscherow S. Posterior chamber phakic intraocular lens for hyperopia of +4 to +11 diopters. J Refract Surg. 1998;14(3):306-311.
6. Pesando PM, Ghiringhello MP, Di Meglio G, Fanton G. Posterior chamber phakic intraocular lens (ICL) for hyperopia: ten-year follow-up. J Cataract Refract Surg. 2007;33(9):1579-1584.
7. Pérez-Vives C, Domínguez-Vicent A, Ferrer-Blasco T, Madrid-Costa D, Montés-Micó R. Optical quality of hyperopic and myopic phakic intraocular lenses. Indian J Ophthalmol. 2014;62(4):437-441.