
The main goal for cataract and refractive surgeons is to provide our patients with excellent surgical outcomes. We create happy patients by supplying them with comfort and a high quality of vision postoperatively. Happy patients then result in more referrals and elevate the reputation of the practice.
Presurgical identification and treatment of dry eye disease (DED) is one of the most essential aspects of setting the stage for good postoperative outcomes. Most patients who present for a cataract evaluation are unaware that they have preexisting DED. The responsibility falls mainly to the surgeon to identify ocular surface disease (OSD) before surgery.
This article presents my top five pearls for managing DED in the presurgical patient.
No. 1: Identify DED. In this population of patients, the classic symptoms of DED will not necessarily be voluntarily disclosed to the surgeon. Patients often attribute their fluctuating vision to the onset of cataract and are unaware of underlying OSD. Most patients coming in for surgical evaluation will have signs of DED, but not necessarily symptoms.1,2 Therefore, it is important for us to look for signs of DED, not symptoms.
For cataract surgeons, it is important to have a set protocol for DED assessment in the preoperative evaluation. The entire office staff and technicians must be aligned on this standardized preoperative testing protocol. At minimum, a thorough slit-lamp examination of the ocular surface, including ocular surface staining and tear breakup time assessment should be done. Whether to go further will be up to the individual practitioner. Some practices use point-of-care testing such as the TearLab Osmolarity System to assess osmolarity and Inflammadry (Quidel) to assess for the presence of the inflammatory marker matrix metalloproteinase-9 (MMP-9) in the tears. Imaging modalities such as meibography and topography can also be helpful.
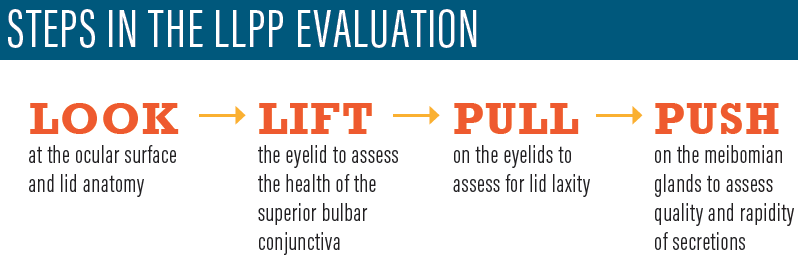
Along with surface vital dye staining, the look, lift, pull, push (LLPP) evaluation can provide a wealth of information about the ocular surface health in a short time. The information generated by these four steps, outlined in Steps in the LLPP Evaluation, will help to guide treatment regimens.
No. 2: Examine the topography. Topography is a great tool to help identify irregular astigmatism, which is a strong indicator of tear film instability in the preoperative patient. Looking at the mire rings for areas of irregularity and dropout can help clue the surgeon in to tear film dysfunction and ocular surface irregularity. Especially if astigmatism management with toric IOLs is planned, DED can significantly throw off the axis and amplitude of the astigmatism. Epitropoulos et al found greater variability in average keratometry values in patients with DED, as defined by high tear osmolarity, than in those with healthy eyes.3
No. 3: Don’t trust the initial biometry. Once OSD and tear film instability are identified in the preoperative patient, be wary of trusting your initial biometry measurements. Especially in planning procedures in which premium IOL technology will be used, it is essential to take the time to treat the tear film irregularity and have the patient return for better measurements at a later time. Studies have also shown that there can be a significant change in the estimated spherical power of the IOL choice in DED patients from before ocular surface treatment to after.3
No. 4: Treat DED aggressively to optimize the ocular surface before surgery. In DED patients, an aggressive multifaceted treatment approach is helpful for achieving a quick turnaround of the ocular surface and tear film. The goal is to be able to get the patient in for surgery without significant delay.
There are three important categories of approach to DED treatment, which are detailed in the sidebar Approaches to DED Treatment. These approaches provide a regenerative microenvironment and antiinflammatory properties to turn the ocular surface around quickly. Whatever cocktail of therapeutics is deemed appropriate for the particular patient in this preoperative setting, an aggressive multifaceted approach is recommended to achieve rapid improvement and prevent significant delay of surgery.
APPROACHES TO DED TREATMENT
Category 1. Treat Ocular Surface Inflammation
A short course of low-potency steroids is a quick way to resolve tear film inflammation rapidly. Lifitegrast ophthalmic solution 5% (Xiidra, Novartis) or one of the available formulations of cyclosporine may also be initiated at this time to provide a long-term solution for postoperative management. Testing for matrix metalloproteinase-9 can be done to identify the presence of inflammatory cytokines. If this point-of-care testing modality is unavailable, conjunctival hyperemia is another indicator of inflammation. If there is concomitant lid margin inflammation and rosacea, a course of oral doxycycline may help quiet the overall inflammatory picture on the ocular surface.
Category 2. Treat Meibomian Gland Dysfunction
Lipid layer dysfunction is an important factor in an unstable tear film. It can lead to fluctuating vision, and it can be a major player in incorrect preoperative biometry measurements and irregular topography. Home application of hot compresses is a good place to start, but by itself this treatment is often ineffective for accomplishing a rapid turnaround in the health of the tear film’s lipid layer. In the preoperative dry eye disease/meibomian gland dysfunction (MGD) patient, I have a low threshold for offering an in-office treatment to help to normalize the lipid layer. This may include thermal pulsation treatment or other in-office procedures that apply heat and encourage evacuation of the meibomian glands to treat MGD.
Category 3. Regenerate the Ocular Surface Epithelium
Significant punctate keratitis of the cornea is another barrier to obtaining clean preoperative measurements. Punctate keratitis can often be reversed with preservative-free lubricants, but sometimes a stronger regenerative therapeutic is required. Autologous serum drops can provide the ocular surface with neurotrophic growth factors that help to reverse microerosions of the corneal and conjunctival surfaces preoperatively. Some national compounding companies can offer quick turnaround times, sending a phlebotomist to the patient’s home and getting the serum back to the patient within a week. The use of in-office self-retaining fresh frozen amniotic membrane can also be helpful, especially for patients with unilateral disease.
No. 5: Educate the patient about DED. One of the most important aspects of managing DED in the preoperative patient is education. Most patients in this setting do not realize that they have underlying OSD. If surgery is initiated and performed without any education on DED, the patient will often blame the surgery for causing postoperative DED.
If the patient is educated beforehand, then the symptoms and signs of DED noted postoperatively will be an expectation rather than a complication of the surgery. Patients should be informed that DED can worsen after cataract surgery, and the most important way to minimize their symptoms postoperatively is to optimize the tear film preoperatively.
Patients appreciate the additional time and effort their surgeon takes to optimize their outcomes, and often their compliance with a therapeutic regimen improves as a result. With thorough education, not only will patient satisfaction be increased, but also postoperative outcomes can be further improved.
1. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
2. Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44(9):1090-1096.
3. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41(8):1672-1677.


