
Wollensak et al reported on the first clinical study of CXL for the treatment of keratoconus in 2003.1 Their protocol, known as the Dresden protocol, involves anesthetizing the eye, removing the central 8 to 10 mm of epithelium, soaking the corneal surface with a riboflavin solution for 30 minutes, and then exposing a central 9-mm zone of the cornea to 5.4 J/cm2 UV-A light at an irradiance of 3 mW/cm2 for 30 minutes. CXL has been a mainstay in the treatment of progressive keratoconus and post-LASIK ectasia throughout Europe and Asia for the past 15 years and in the United States for the past 4 years. CXL induces changes in the anterior 250 to 300 µm of the corneal stroma, and a minimum corneal thickness of 400 µm is necessary to protect the corneal endothelium from potential damage.
Several different modifications to the Dresden protocol have shortened the duration of the procedure (accelerated CXL), improved the recovery process and reduced complications (epithelium-on CXL), and improved visual outcomes (customized CXL and CXL combined with topography-guided PRK).
available THERAPeutic indications
The main therapeutic indications for CXL are stabilizing keratoconus and post-LASIK ectasia in adults, stabilizing keratoconus in children and adolescents, and improving visual outcomes in patients with keratoconus.
Stabilizing keratoconus and post-LASIK ectasia in adults. CXL is indicated primarily for the treatment of progressive keratoconus and LASIK-associated ectasia. Documenting disease progression is recommended before performing CXL on adults with keratoconus. Numerous studies using the Dresden protocol found significant flattening of the steepest keratometry reading and improvements in visual acuity and corneal topography after treatment.2 Long-term studies with follow-ups ranging from 4 to 7 years have also shown continued improvements in topographic parameters for up to 7 years after CXL.3 Epithelium-off (epi-off) CXL has been shown to be effective in stabilizing post-LASIK ectasia and improving visual acuity in studies with more than 2 years of follow-up.4
The major drawback of the Dresden protocol for CXL is its long duration. To address this, various accelerated CXL protocols have been developed based on the Bunsen-Roscoe law of reciprocity.5 These accelerated protocols use power settings ranging from 7 to 30 mW/cm2 and a duration of irradiation ranging from 3 to 15 minutes. Although clinical studies have demonstrated that certain protocols for accelerated CXL stabilize the disease and produce significant corneal flattening, they have also reported that the demarcation line was deeper and better defined in eyes treated with an irradiance of 3 or 9 mW/cm2 than with higher energy.6 Long-term comparative studies are required to determine whether accelerated CXL produces results that are comparable to those achieved with the Dresden protocol.
Epi-off CXL is also associated with significant postoperative pain and increased risks of infection and corneal scarring, leading to interest in epithelium-on (epi-on) techniques. Initial studies showed that epi-on CXL is less effective than epi-off CXL. Recent modifications to improve the efficacy of the epi-on technique include the use of supplemental oxygen, high UV-A energy, and modified riboflavin formulations to enhance epithelial penetration (Figure). A phase 3 randomized controlled trial is currently being conducted in the United States to evaluate the safety and efficacy of epi-on CXL with supplemental oxygen.
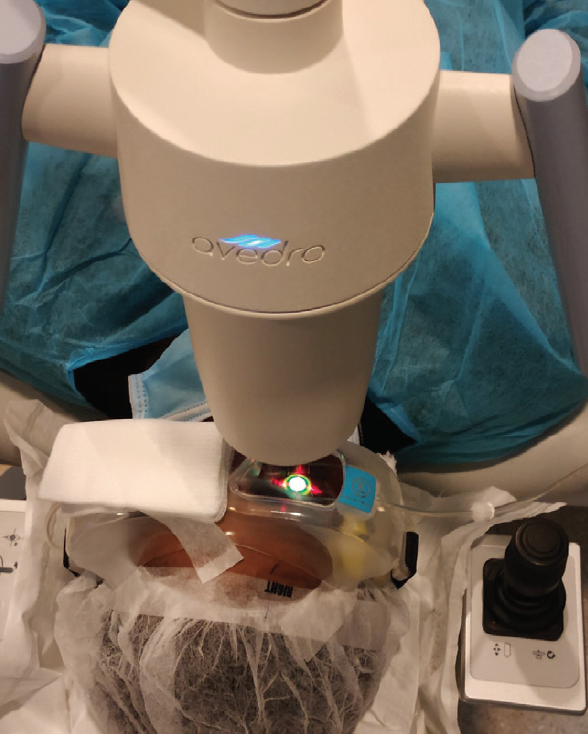
Figure. Epi-on CXL with supplemental oxygen.
Stabilizing keratoconus in pediatric patients. Keratoconus often progresses more rapidly in children than in adults. It therefore is not necessary to document disease progression before performing CXL on children.7 Studies have shown that an epi-off technique is preferable in pediatric patients because keratometry values worsened over time after epi-on CXL was performed in this population.8
Improving visual outcomes in patients with keratoconus. Many patients lack functional vision after CXL. Refractive procedures have therefore been combined with CXL to improve postoperative visual acuity. Examples of so-called CXL plus procedures include pairing CXL with topography-guided PRK,9 transepithelial phototherapeutic keratectomy,10 intrastromal corneal ring segment implantation,11 and phakic IOL implantation.12
Another procedure aimed at improving visual outcomes is customized CXL. During this epi-on procedure, customized topography-guided UV-A energy is delivered to the cornea, with more energy focused on the cone than the periphery. Initial studies using the Mosaic System (Avedro) showed improvements in visual outcomes and regularization of corneal topography.13,14
FUTURE THERAPIES
Potential future therapeutic applications include CXL for the treatment of infectious keratitis and scleral CXL for axial myopia.
CXL for the treatment of infectious keratitis. The antimicrobial effect of riboflavin photoactivation is being explored as a potential treatment for ophthalmic infectious diseases. For example, CXL and photoactivated chromophore for keratitis (PACK-CXL) have been investigated as a possible treatment for infectious keratitis.15 PACK-CXL makes the cornea more resistant to enzymatic degradation by microbes by stiffening the corneal stroma and thus reducing the progression of corneal melting.16 The procedure is contraindicated in eyes with previous herpes simplex virus infection. PACK-CXL has been shown to be more effective for bacterial than fungal infections.17 The available evidence supports the use of PACK-CXL in the treatment of infectious keratitis, but randomized controlled trials are required.18
Scleral CXL for axial myopia. To date, there is no efficient and effective method of treating progressive myopia. Severe myopia causes progressive thinning and weakening of the sclera, and several studies have shown that impaired collagen crosslinking is an important factor in the weakening process of the myopic sclera.19-21 This finding suggests that techniques that induce collagen crosslinking, such as CXL using riboflavin and UV-A radiation, could also inhibit eye elongation and slow the progression of myopia.22
Early studies showed that the combined use of riboflavin and UV-A light increased the mechanical strength of the sclera in a rabbit model, but treatment also resulted in a significant loss of photoreceptors and retinal pigment epithelium.22 CXL has been shown to stiffen and stabilize collagen-based tissues such as the sclera, but its potential application to the sclera for the treatment of myopia faces several barriers, particularly a potential cytotoxic risk to the retina.23
Conclusion
CXL is evolving with accelerated protocols, epi-on techniques, combined procedures, and customized approaches. A greater degree of customization of treatments with accelerated protocols and epi-on techniques is likely to enable surgeons to achieve better refractive outcomes while maintaining a high level of safety.
Potential future applications of CXL include the treatment of infectious keratitis and progressive myopia. These are exciting applications that require further study to determine their safety and efficacy.
1. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620-627.
2. Wittig-Silva C, Chan E, Islam FM, Wu T, Whiting M, Snibson GR. A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophthalmology. 2014;121(4):812-821.
3. O’Brart DP, Patel P, Lascaratos G, Wagh VK, Tam C, Lee J, et al. Corneal cross-linking to halt the progression of keratoconus and corneal ectasia: seven-year follow-up. Am J Ophthalmol. 2015;160(6):1154-1163.
4. Richoz O, Mavrakanas N, Pajic B, Hafezi F. Corneal collagen cross-linking for ectasia after LASIK and photorefractive keratectomy: long-term results. Ophthalmology. 2013;120(7):1354-1359.
5. Bunsen R RH. Photochemische untersuchungen. Poggendorff’s Annalen. 1855;96:373-394.
6. Shetty R, Pahuja NK, Nuijts RM, et al. Current protocols of corneal collagen cross-linking: visual, refractive, and tomographic outcomes. Am J Ophthalmol. 2015;160:243-249.
7. Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents. J Refract Surg. 2012;28(11):753-758.
8. Buzzonetti L, Petrocelli G. Transepithelial corneal cross-linking in pediatric patients: early results. J Refract Surg. 2012;28(11):763-7.
9. Kanellopoulos AJ, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens Protocol). J Refract Surg. 2014;30(5):342-346.
10. Kymionis GD, Grentzelos MA, Kounis GA, Diakonis VF, Limnopoulou AN, Panagopoulou SI. Combined transepithelial phototherapeutic keratectomy and corneal collagen cross-linking for progressive keratoconus. Ophthalmology. 2012;119(9):1777-1784.
11. Ertan A, Karacal H, Kamburoglu G. Refractive and topographic results of transepithelial cross-linking treatment in eyes with intacs. Cornea. 2009;28(7):719-723.
12 Fadlallah A, Dirani A, El Rami H, Cherfane G, Jarade E. Safety and visual outcome of Visian Toric ICL implantation after corneal collagen cross-linking in keratoconus. J Refract Surg. 2013;29(2):84-89.
13. Roberts CJ, Dupps WJ Jr. Biomechanics of corneal ectasia and biomechanical treatments. J Cataract Refract Surg. 2014;40:991-998.
14. Seiler TG, Fischinger I, Koller T, Zapp D, Frueh BE, Seiler T. Customized corneal cross-linking: one-year results. Am J Ophthalmol. 2016;166:14-21.
15. Tabibian D, Richoz O, Hafezi F. PACK-CXL: corneal cross-linking for treatment of infectious keratitis. J Ophthalmic Vis Res. 2015;10(1):77-80.
16. Spoerl E, Wollensak G, Seiler T. Increased resistance of crosslinked cornea against enzymatic digestion. Curr Eye Res. 2004;29(1):35-40.
17. Price MO, Tenkman LR, Schrier A, Fairchild KM, Trokel SL, Price FW Jr. Photoactivated riboflavin treatment of infectious keratitis using collagen cross-linking technology. J Refract Surg. 2012;28(10):706-713.
18. Alió JL, Abbouda A, Valle DD, Del Castillo JM, Fernandez JA. Corneal cross linking and infectious keratitis: a systematic review with a meta-analysis of reported cases. J Ophthalmic Inflamm Infect. 2013;3(1):47.
19. Iseli HP, Körber N, Koch C, et al. Scleral cross-linking by riboflavin and blue light application in young rabbits: damage threshold and eye growth inhibition. Graefes Arch Clin Exp Ophthalmol. 2016;254:109-122.
20. Dotan A, Kremer I, Gal-Or O, et al. Scleral cross-linking using riboflavin and ultraviolet-A radiation for prevention of axial myopia in a rabbit model. J Vis Exp. 2016;(110):e53201.
21. McBrien NA, Norton TT. Prevention of collagen crosslinking increases form-deprivation myopia in tree shrew. Exp Eye Res. 1994;59(4):475-486.
22. Wollensak G, Iomdina E, Dittert DD, Salamatina O, Stoltenburg G. Cross-linking of scleral collagen in the rabbit using riboflavin and UVA. Acta Ophthalmol Scand. 2005;83(4):477-482.
23. Elsheikh A, Phillips J. Is scleral cross-linking a feasible treatment for myopia control? Ophthalmic Physiol Opt. 2013;33:385-389.


