In this month’s Fundamentals in Five, I am pleased to have Simon D. Chen, MBBS, BSc, FRANZCO, contribute an article on the management of a dropped nucleus. Dr. Chen offers a unique perspective as a fellowship-trained retina specialist who also has a special interest in complex cataract surgery. In this article, Dr. Chen outlines his expert pearls on how to handle this complication of cataract surgery.
—Kavitha R. Sivaraman, MD, Section Editor

A dropped nucleus is one of the most feared complications of cataract surgery and one that all cataract surgeons will encounter if they perform a significant volume of surgery (Figure 1). It is therefore important for ophthalmologists to be aware of the clinical factors associated with an increased risk of a dropped nucleus when assessing patients for cataract surgery. These risk factors include features associated with weak zonules (eg, pseudoexfoliation, previous ocular trauma, previous vitrectomy, high myopia, uveitis, and retinitis pigmentosa) and an increased risk of a posterior capsular tear (eg, small pupil, dense cataract, posterior polar cataract, previous intravitreal injection, less experienced surgeon, and patient with a learning disorder or condition such as dementia who might be more likely to move unexpectedly during surgery).
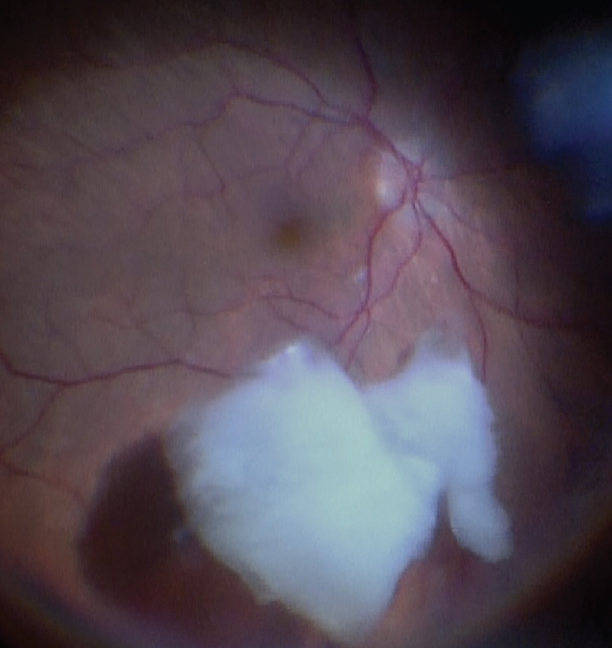
Figure 1. Dropped nucleus.
This article describes fundamental concepts in managing a dropped nucleus to minimize the risk of visual loss due to secondary complications such as retinal detachment (RD), cystoid macular edema, corneal edema, uveitis, and glaucoma.
1. Prepare an Action Plan
When operating on patients at increased risk of a dropped nucleus, prepare an action plan in advance.
Practice drills. Consider running a regular vitreous loss fire drill to familiarize all surgical team members with the necessary adjuncts to manage the complication.1
Smart scheduling. Schedule the surgery on a day when experienced nursing and anesthetic staff who are familiar with the equipment and techniques required to convert the case to an anterior vitrectomy if a dropped nucleus occurs are available. Less experienced surgeons should ensure that a senior, more experienced surgeon is available to assist them if necessary. Check that your preferred retina surgeon is not on leave at the time of surgery.
I schedule difficult cases at the end of an operating list so that I am surgically warmed up and do not have the time pressure of additional cases waiting to be performed. Some surgeons prefer to schedule complex cases near the start of a list when they are feeling most fresh.
Anesthesia. Consider whether periocular or general anesthesia may be more appropriate than topical anesthesia to make the case easier in the event of complications.
Anterior vitrectomy. Ensure that appropriate equipment for an anterior vitrectomy is ready. This includes an anterior vitrectomy cutter, corneal sutures, an appropriately powered backup three-piece IOL for sulcus placement, triamcinolone acetonide, and acetylcholine chloride (Miochol-E, Bausch + Lomb).
Familiarize yourself with the machine settings required for an anterior vitrectomy.
IOL. Determine the power and model of IOL you will use if the posterior capsule is compromised. Familiarize yourself with the loading and insertion of three-piece IOLs and the power changes required for placement in the sulcus versus in the bag.
Patient education. Before proceeding to surgery, inform patients about the possibility of a dropped nucleus and their potential need for a second operation by a retina surgeon. Patients are generally much more accepting of a complication if they have been warned about its possibility beforehand.
2. Don’t Chase the Nucleus
During surgery, it is important to recognize the signs of a torn posterior capsule, zonular weakness, and an impending dropped nucleus as early as possible so that you can avoid actions that might increase vitreoretinal traction. As soon as you suspect the nucleus will drop, pause and collect your thoughts. Actively avoid denial—accept the situation and proceed. The priority at this stage is to minimize vitreoretinal traction because it can lead to an RD.
Maintain infusion and resist the urge to remove the phaco handpiece from the eye because decompression of the anterior chamber can lead to vitreous prolapse. Instead, while maintaining infusion, remove your second instrument and then inject a dispersive OVD to pressurize the anterior chamber and tamponade the vitreous before removing the phaco handpiece.
When a significant lens fragment has dropped, resist the temptation to chase and retrieve it. Posterior-assisted levitation using a cyclodialysis spatula or an OVD injected with a cannula passed through the pars plana incision to lift displaced lens fragments into the anterior chamber has been reported, but most retina surgeons strongly advise against using this technique.2 If you have access to a retina surgeon, don’t take the unnecessary risk of generating uncontrolled vitreoretinal traction, which can cause a retinal tear or RD.
Do not continue phacoemulsification in the presence of vitreous. The phaco handpiece cannot cut vitreous gel but will aspirate it, which can lead to vitreoretinal traction that is transmitted to the retina and can greatly increase the risk of a retinal tear.
Create a second paracentesis to perform a bimanual anterior vitrectomy to clear vitreous from the anterior segment. The keratome incision should not be used for either the infusion or the vitrectomy probe. Use the maximum cutting rate available on your machine, with low vacuum and low infusion pressure. Debulk the anterior vitreous behind the posterior capsule to prevent further vitreous prolapse. Pass the vitrectomy probe posteriorly through a posterior capsular tear. The principle is to have the vitrectomy probe pull vitreous posteriorly, not anteriorly, to minimize vitreoretinal traction. Do not worry if additional lens fragments dislocate posteriorly. The retina surgeon can clear them later. Be careful to preserve the remaining lens capsule.
3. Tidy the Anterior Segment
Use diluted intracameral triamcinolone to visualize vitreous strands in the anterior chamber that can be cleared with the vitrectomy probe. After the anterior chamber is clear of vitreous, remove remaining lens material from the capsular bag, sulcus, and anterior chamber. This can be done with a vitrectomy probe, I/A handpiece, or phaco probe if hard nuclear fragments remain. If using the phaco probe, reduce phaco vacuum and aspiration levels and irrigation pressure to minimize the risk of aspirating vitreous. There is some variability of practice patterns, however, and some surgeons advocate against reintroducing the phaco probe or I/A handpiece into the eye when vitreous loss has occurred.
It is important to clear the anterior segment of lens material, OVD, and vitreous to minimize the risk of overnight IOP spikes, corneal edema, corneal endothelial cell loss, and cystoid macular edema during the early postoperative period. These can have a negative impact on the patient’s vision and make subsequent vitrectomy surgery significantly more difficult (Figure 2). A clear cornea makes the retina surgeon’s job easier by allowing clear visualization of the posterior segment.
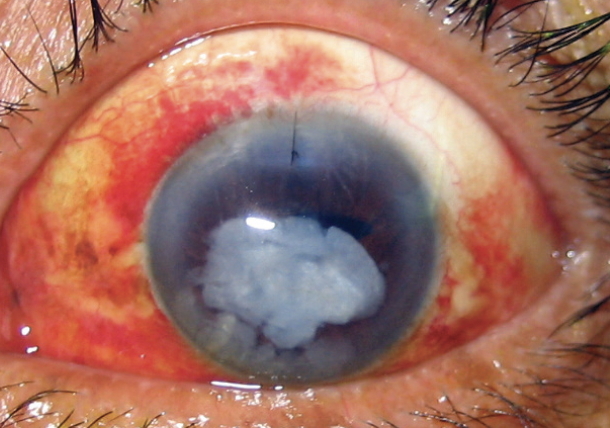
Figure 2. Residual lens fragment in the anterior chamber and corneal edema.
At the end of the case, inject intracameral acetylcholine chloride to constrict the pupil. Look carefully for peaking of the pupil as an indicator of a residual vitreous strand, which can act as a potential entry route for intraocular bacteria if it extends to a corneal incision. Inject intracameral antibiotics to reduce the risk of endophthalmitis.
4. Place an IOL
It is generally best to implant an IOL when safe to do so. If there is sufficient capsular support, implant a three-piece IOL in the sulcus. If the capsulorhexis is intact, optic capture generally leads to a stable, well-centered IOL.
5. Be Proactive in the Early Postoperative Period
Contact your retina surgeon as soon as possible after the case is complete so they can schedule the patient for a vitrectomy.
Initiate intensive treatment with topical steroids and NSAIDs. Postoperative IOP spikes are common following a dropped nucleus, and they often cause corneal edema, which may delay the vitrectomy or make the surgery more difficult. For this reason, I recommend initiating treatment with oral acetazolamide to minimize overnight IOP spikes.
Explain what happened to the patient and advise them that they will see a retina surgeon who may perform another operation. Reassure the patient that retina surgeons regularly perform surgery for dropped nuclei and that outcomes are generally good.
Conclusion
A dropped nucleus during cataract surgery is uncommon, but it can cause sight-threatening complications. Having an appropriate surgical action plan, minimizing vitreoretinal traction, and making an early referral to a retina surgeon can minimize the risk of a poor outcome.
1. Lockington D, Belin M, McGhee CNJ. The need for all cataract surgeons to run a regular vitreous loss fire drill. Eye (Lond). 2017;31(8):1120-1121.
2. Chang DF, Packard RB. Posterior assisted levitation for nucleus retrieval using Viscoat after posterior capsule rupture. J Cataract Refract Surg. 2003;29(10):1860-1865.


