Phaco cataract surgery is perhaps one of most frequently performed ophthalmic procedures. In addition to restoring vision, the procedure can assist with refractive and presbyopia correction, facilitate fundus examinations in patients with diabetes, lower IOP in patients with glaucoma or ocular hypertension (OHT), and open the trabecular-iris angle in eyes experiencing angle closure.
Advances in phaco technology have enhanced intraoperative stability, minimized surgical complications, and shortened postoperative recovery times. A remaining challenge is IOP spikes, which can occur even after uneventful phacoemulsification and persist despite typical treatments such as topical and systemic antiglaucoma medications and conventional anterior chamber paracentesis (ACP).
The peak IOP rise typically occurs 8 to 12 hours after cataract surgery. An estimated 1.3% to 10.0% of patients may experience an increase in IOP to above 30 mm Hg more than 24 hours after phacoemulsification.1 IOP spikes are of greatest concern in individuals who have advanced glaucoma because increased IOP may further compromise the optic nerve and cause visual field loss or a total wipeout. Patients with diabetes, OHT, hyperlipidemia, autoimmune disease, anemia, and obstructive sleep apnea are also at risk of optic nerve damage from the IOP spikes.2
This article describes a novel leaky (non–self-sealing) ACP we devised that has been used at our centers for the past several years.
THE TECHNIQUE
Protocol. The leaky ACP technique is implemented when the IOP rises during the first 24 hours after phacoemulsification.3 If IOP is greater than 22 mm Hg, it is rechecked after 20 to 30 minutes to confirm the rise and document its increasing or decreasing trajectory. A leaky ACP is created if the IOP is greater than 25 mm Hg in an eye at moderate to high risk of glaucomatous damage such as one with advanced glaucoma.
Description of the technique. Topical medications—including three rounds of local anesthesia, levofloxacin, and tobramycin administered every minute—are given before the ACP is created.
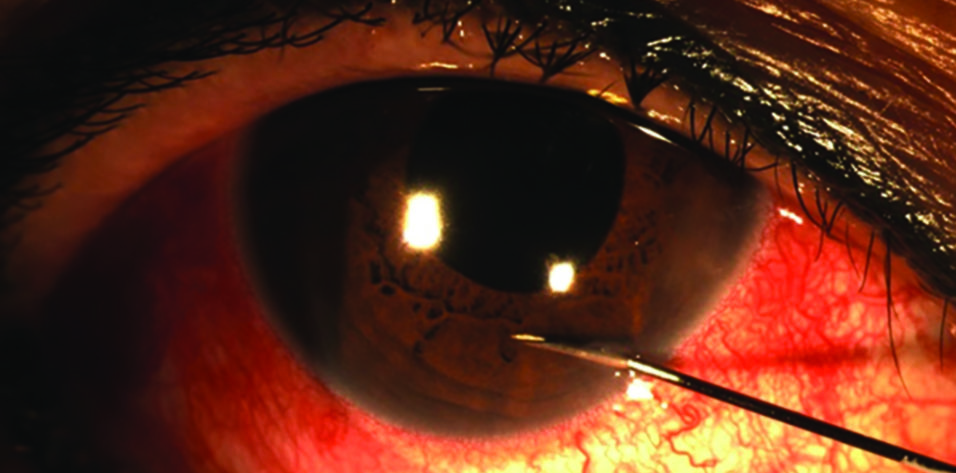
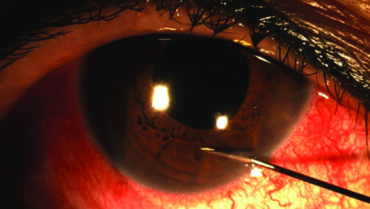
A 30-gauge needle is used if the IOP is 35 mm Hg or less; a 27-gauge needle is used if the IOP is greater than 35 mm Hg. The needle entry for the paracentesis is angled at 90º to the corneal plane (or 45º to the iris plane) via the peripheral inferior cornea (nasally or temporally depending on the hand dominance of the surgeon and whether the right or left eye is being treated). The needle is held in place for about 5 seconds (Figures 1 and 2).
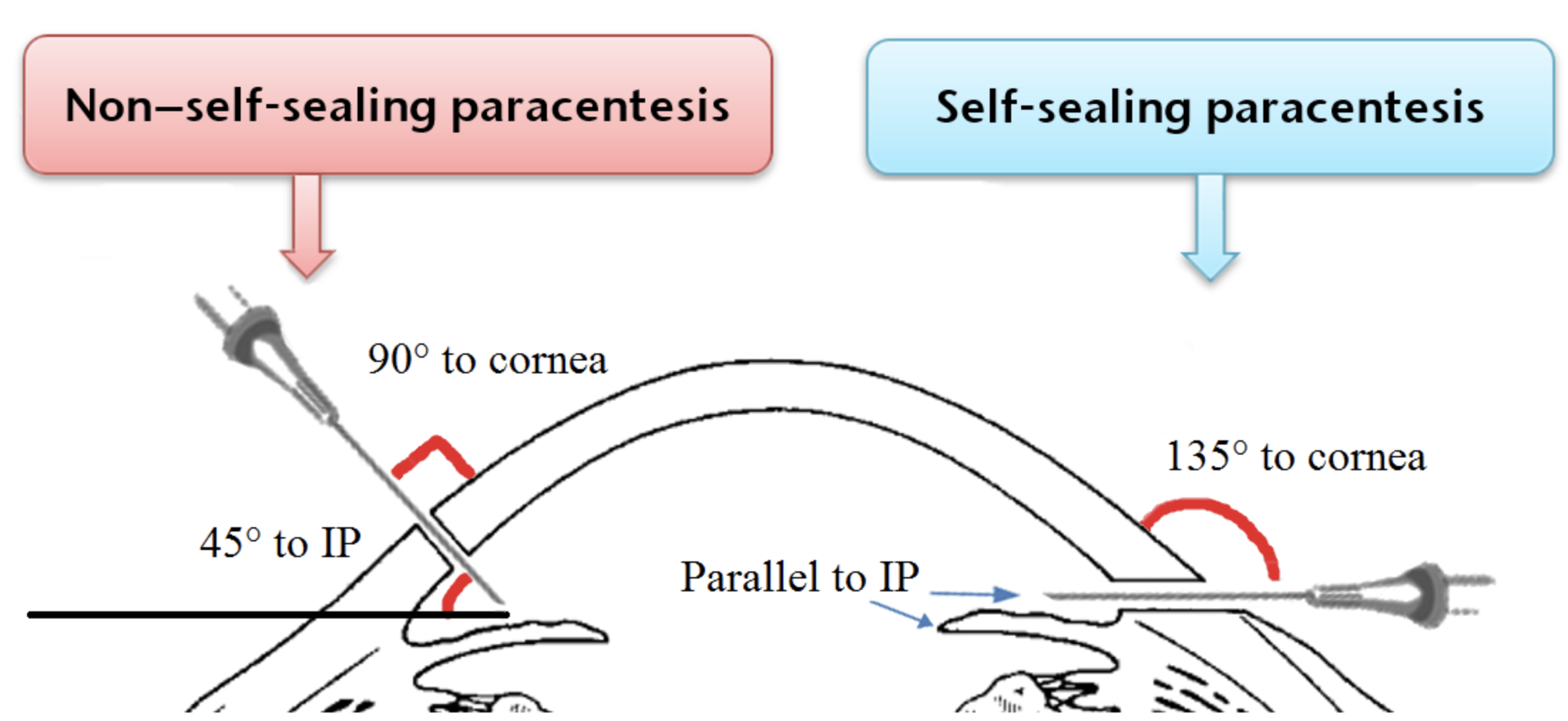
Figure 1. The non–self-sealing ACP is created when a 30- or 27-gauge needle is used to pierce the peripheral cornea at either a 90º angle to the corneal plane or a 45º angle to the iris plane (IP). The self-sealing ACP is done with the needle positioned parallel to the IP.
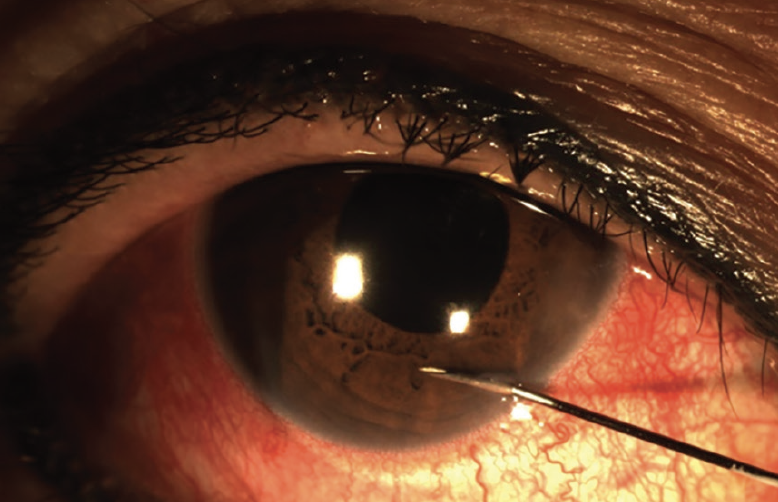
Figure 2. Slit-lamp photograph shows the creation of a non–self-sealing ACP with a 30-gauge needle.
The angulation of the needle for the leaky ACP differs from that used for a conventional ACP. In the latter technique, the needle entry is parallel to the iris plane, which creates a longer channel that seals much sooner. Our modified approach creates a relatively shorter channel that takes longer to seal, allowing a continuous outflow of aqueous to lower IOP during the early postoperative period. It usually takes about 4 to 8 hours and 12 to 36 hours for leaky ACPs to close when created with a 30-gauge and a 27-gauge needle, respectively. (See below for a demonstration of the leaky ACP technique.)
After the needle is removed, the IOP usually decreases to approximately 5 to 15 mm Hg. Topical medications are then administered, including three rounds of levofloxacin and tobramycin instilled every minute. The dual antibiotics cover both Gram-negative and Gram-positive bacteria.
The IOP is rechecked within 10 minutes of the creation of the ACP and then again at 30 and 60 minutes. A second leaky ACP is created at a different location if the IOP remains high. Otherwise, the eye is examined at the slit lamp, and the patient is discharged with instructions to follow a standard postoperative regimen for phacoemulsification and antiglaucoma medications as appropriate.
Risks. The risks associated with the leaky ACP technique are few. They include trauma to the iris or corneal endothelium, infection, a flat anterior chamber, and hypotony. The only contraindication for this technique may be a shallow anterior chamber, but this is an unusual finding after phacoemulsification.
The amount of aqueous drainage can be titrated according to the level of IOP rise by adjusting the size of the needle used during ACP. The unique angulation of the leaky ACP creates a positive-pressure outflow channel. This in combination with the use of a single-use, small-caliber needle reduces the risk of infection.
During the past few years, we have used the leaky ACP technique in hundreds of cases at our clinics and hospitals in Hong Kong and elsewhere in China. We have not encountered infection or a significant complication from the procedure. We did, however, have a few instances of a shallow anterior chamber when the procedure was performed with a 27-gauge needle. A normal depth was restored in each instance after a few hours or less of pressure eye patching.
CONCLUSION
IOP spikes after phaco cataract surgery are not uncommon and they can cause devastating damage, especially in at-risk patients. The leaky ACP technique can protect patients against persistent IOP spikes. It can also be used in patients with ocular conditions such as uveitic glaucoma, steroid-induced OHT, and high IOP from trauma when a quick and sustainable reduction in IOP is desirable.
1. Hildebrand GD, Wickremasinghe SS, Tranos PG, , Harris ML, Little BC. Efficacy of anterior chamber decompression in controlling early intraocular pressure spikes after uneventful phacoemulsification. J Cataract Refract Surg. 2003;29(6):1087-1092.
2. Tranos P, Bhar G, Little B. Postoperative intraocular pressure spikes: the need to treat. Eye (Lond). 2004;18(7):673-679.
3. Lam D, Lee J, Leung E, Liu S, Yuan J, Ratra V. Non–self-sealing (leaky) anterior chamber paracentesis: a new technique in managing postphacoemulsification intraocular pressure rise in glaucoma and normal eyes. Asia Pac J Ophthalmol (Phila). 2018;7(5):284-287.