Anyone with an interest in ophthalmology over the past decade or so has heard of MIGS. Its impact, though broad, is well understood. Despite that the category of minimally invasive surgeries has evolved and grown, the central premise remains true: achieve modest IOP reduction with a safe procedure associated with minimal postoperative recovery and rapid visual recovery.
One factor that may drive the next evolution in MIGS is that performing these surgeries is no longer the sole purview of subspeciality trained glaucoma surgeons, and that is in fact the best possible scenario for patients. At a fundamental level, more cataract and refractive surgeons performing MIGS, even in standalone settings, represents a wider pool of experience from which best-practices in clinical practices, and such things as patient selection, can be delineated.
Blake K. Williamson, MD, MPH, MS, joined an episode of IJC dedicated to taking a deeper look at this changing paradigm.
The 30,000-Foot View
MIGS is associated with several positive outcomes. The library of studies demonstrating postoperative IOPs in the mid-teens in eyes with mild to moderate open-angle glaucoma is deep and convincing. Evidence of safety, pertaining to the class and to its members, is overwhelming.
Other endpoints, technically considered secondary in clinical studies, may be just as important. For instance, a few studies to date have pointed to the potential to forestall the necessity for incisional glaucoma procedures if MIGS is performed earlier in the disease course. There is also emerging evidence that some MIGS procedures are associated with greater preservation of visual field compared to drops.
From the patient perspective, the more-than-likely reduction in drop burden after a MIGS procedure may promote the health of the ocular surface. According to Dr. Williamson, drop burden reduction is even more meaningful when the impact on how that affects quality of life is considered.
“I think that what shocks me when I'm talking to my refractive buddies is that many patients are every bit as happy to get off medications as they are to get out of glasses,” Dr. Williamson said. “We always celebrate getting [patients] out of readers, getting [patients] out of contacts. But patients absolutely love being able to reduce their medication burden.”
MIGS is “the right thing to do for our patients,” Dr. Williamson added. But the real reason he incorporates MIGS in both combined and standalone settings into his surgical armamentarium?
“Happier patients,” he said.
Redefining a “Successful” Outcome
The importance given to potential IOP reduction, and then magnitude of reduction after that, is in some respects understandable, given their utility for clinical trials, clinical practice, and for regulatory purposes. In MIGS surgeries in the real world, however, those endpoints may underrepresent the true impact. Indeed, achieving the target pressure after an uncomplicated MIGS procedure is a laudable endpoint, as is reduction of medications. But there is still more to the story of how success is defined, according to Dr. Williamson.
“Yes, that's a home run, but sometimes all you need is a single or double. I think that preventing further surgery, I think that's a success. Let's say that their pressure doesn't get any worse, and at least you're not having to add medications and you're preventing that incisional surgery for later. You're kicking the can down the road, saving some real estate. That's success too. While it's nice to present studies that show 30 to 35% IOP reductions and reductions in medication burden, I think it's also important to highlight that that's not the only way to create what we call success with MIGS surgery.”
Summing up his message to his fellow front of the eye surgeons, Dr. Williamson suggested to “consider the alternative, and the alternative is inertia, doing nothing, adding more drops, waiting for field loss, and boy, that doesn’t sound good if it were my family.”
Study Data
Dr. Williamson reviewed data from two different MIGS devices that he said typify what he sees in real-world practice.
The first was a review of 12-month outcomes after the STREAMLINE Surgical System (New World Medical) in Hispanic patients with mild to moderate POAG. Dr. Williamson said that what he appreciated was that the baseline IOP of ~16 was indicative of the patients in his own practice (Figure 3).1 The second was a study in which Dr. Williamson served as lead author: 24-month data from the ROMEO study, an effort to understand longer-term outcomes with the OMNI Surgical System as a standalone procedure or combined with cataract surgery. Of note, the study reported IOP response stratified by baseline IOP: >18 mm Hg vs ≤18 mm Hg (Figure 4).2 Intergroup difference was less important than providing clinicians a framework for understanding outcomes in patient types representative of individuals who walk through clinic doors each and every day.
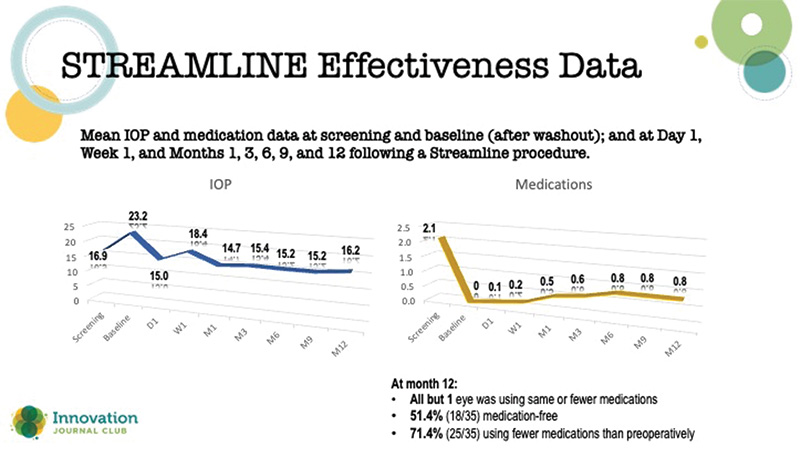
Figure 3. Results from a 12-month study of STREAMLINE.
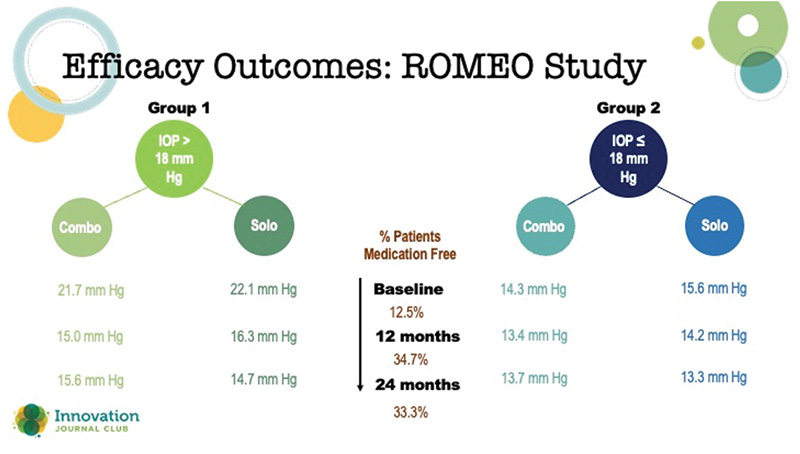
Figure 4. Two-year data from the ROMEO Study with the OMNI.
1. Lazcano-Gomez G, Antzoulatos GL, Kahook MY. Combined Phacoemulsification and STREAMLINE surgical system canal of schlemm transluminal dilation in eyes of Hispanic patients with mild to moderate glaucoma. Clin Ophthalmol. 2023;17:1911-1918.
2. Williamson BK, Vold SD, Campbell A, et al. Canaloplasty and trabeculotomy with the OMNI system in patients with open-angle glaucoma: two-year results from the ROMEO Study. Clin Ophthalmol. 2023;17:1057-1066.


