The concept of modulating pupil size to improve image quality is not new, but the advent of novel pupil-modulating drops for presbyopia correction has reinvigorated discussion of the topic. A small aperture can increase depth of focus and depth of field.1 The pinhole effect is often observed in the clinical setting during the patient’s visual assessment and refinement of their refraction.
Vuity (pilocarpine HCL ophthalmic solution 1.25%; Allergan) is the first FDA-approved medication for presbyopia that changes the size of the pupil to increase depth of focus for intermediate and near vision ranges while preserving distance vision.2 In addition to the treatment of presbyopia, pupil-modulating eye drop formulations to achieve pupillary contraction and/or constriction with differing mechanisms of action have been used off-label for other conditions. Commonly used pupil-modulating agents include pilocarpine 1% or 2% (parasympathetic stimulants) and brimonidine 0.15% or 0.2% (selective alpha-2 adrenergic receptor agonists). These agents typically have been used for the treatment of pseudophakic positive dysphotopsias, noted most prominently and commonly with a large pupil in mesopic settings. Pupillary constriction is thought to mitigate the sensation of glare and halos often associated with diffractive IOL technologies or a pseudophakic state. Surgeons can consider the off-label use of pupil-modulating drops in such situations to decrease dysphotopsias.
The drops can also be used off-label to increase the range of vision for pseudophakic patients. They can be used to enhance postoperative near vision in those who received an extended depth of focus or low-add multifocal lens but did not achieve the level of near vision they desired. If the drop is successful in fine-tuning their visual demands, spectacle wear or an IOL exchange may be avoided. Similarly, pupil-constricting drops can be used for patients with standard monofocal IOLs who require readers and/or bifocal glasses to improve their depth of field and reduce their spectacle dependence.
The ability of pupil-modulating drops to increase depth of focus and decrease aberrations suggests that they may be useful for the management of several complex corneal conditions. Simulating a pinhole effect and increasing depth of focus with pupil-modulating drops may improve the vision of patients with atypical corneas after refractive surgery procedures, including radial keratotomy (RK), LASIK, PRK, and SMILE, and individuals with ectasia, keratoconus, pellucid marginal degeneration, corneal scars, endothelial dystrophy, or anterior basement membrane dystrophy.
We use pupil-modulating drops off-label in a few specific situations, as described here.
1. IRREGULAR CORNEA AFTER CATARACT SURGERY
Poor quality and range of vision. Patients with irregular corneas and a moderate amount of higher-order aberrations (HOAs) such as corneas with ectasia or keratoconus or even after penetrating keratoplasty are at increased risk of experiencing dysphotopsias after cataract surgery.3 Monofocal IOLs are often preferred for these individuals to reduce their risk of poor postoperative optical quality and suboptimal outcomes. The implantation of diffractive IOL technologies increases the risks of postoperative dissatisfaction and poor image quality.
Therapy with a pupil-modulating drop to create a small pupillary aperture may improve postoperative quality of vision. Further, it can provide a slight increase in near and intermediate vision in a pseudophakic eye if the monofocal IOL is targeted for distance vision. Treatment may also increase range of vision if slight myopia was targeted.
Individuals with a history of laser refractive surgery are often highly motivated to achieve spectacle independence at both distance and near after cataract surgery. Decentered ablations or large degrees of preexisting HOAs secondary to laser surgery can make some of them poor candidates for extended depth of focus or diffractive IOLs. The use of pupil-modulating drops after the implantation of monofocal or monofocal toric IOL technologies may augment patients’ range of vision and help modulate their symptoms due to HOAs or irregular astigmatism.
Residual refractive error. Despite advances in IOL calculations and the use of intraoperative aberrometry, a residual refractive error can still occur. Glasses, contact lenses, or an IOL exchange may be required for individuals with a refractive surprise. The use of a pupil-modulating drop, however, may create enough depth of focus for some of these patients to avoid full-time spectacle correction.
Fluctuating vision. The use of a pupil-modulating drop may benefit patients with moderate to severe ocular surface disease (ie, dry eye disease or anterior basement membrane dystrophy) that is causing vision fluctuations after cataract surgery. These individuals may not be able to tolerate a laser vision correction enhancement or contact lenses postoperatively. Similarly, patients with a history of RK often experience vision fluctuations throughout the day, which can make biometry inaccurate. If patients have a small residual refractive error and/or HOAs after cataract surgery, creating a pinhole effect with a pupil-modulating drop may improve their quality of vision.
Interim measure. The use of a miotic agent after cataract surgery can be a helpful therapeutic option for patients with irregular corneas until a small-aperture IOL becomes available in the United States. The IC-8 IOL (AcuFocus) is currently in FDA trials.4
2. CORNEAL SCARS
We often encounter patients with corneal irregularities, namely corneal scars or haze, that can cause significant light scatter. The scars can be secondary to prior trauma, corneal infection, or prior ocular surgery. When a small aperture is created, stray rays of light passing through an aberrated cornea can be collimated.
A trial of pupil-modulating drops can be helpful if a patient with a corneal scar notes an improvement in vision during a simple pinhole test in the clinic. Reducing the pupil size can reduce light scatter from unfocused peripheral light rays as well as HOAs induced by the corneal scarring. A smaller pupil can also improve the quality of vision for patients, especially if they are unable to wear hard contact lenses and are trying to achieve improved quality of vision with spectacles (Figure 1).
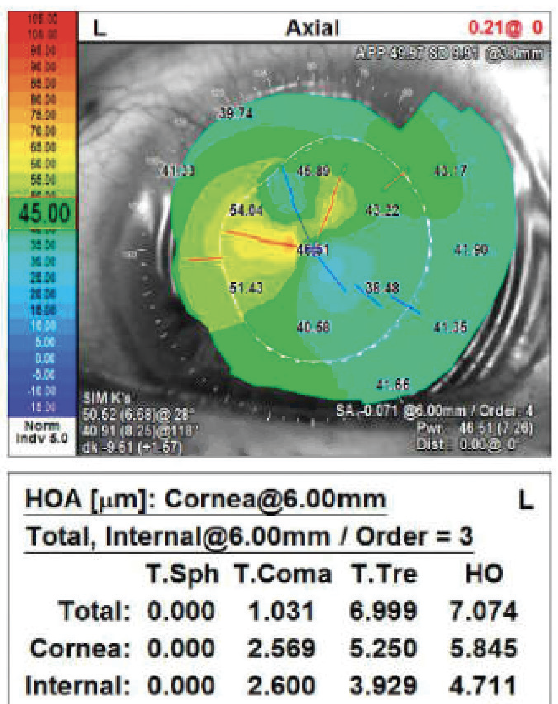
Figure 1. Topography of a patient with high irregular astigmatism from a paracentral corneal scar secondary to a prior keratitis episode. An off-label trial of a pupil-modulating drop demonstrated improvement in the patient’s glare symptoms with glasses.
3. POOR QUALITY OF VISION IN MESOPIC AND SCOTOPIC LIGHTING CONDITIONS AFTER REFRACTIVE SURGERY
Patients may experience glare and halos after undergoing RK, LASIK, PRK, or the implantation of a phakic IOL (Evo Visian ICL, STAAR Surgical). Spherical aberration often increases after refractive surgery, and a large pupil can amplify the effect.
The administration of a pupil-modulating drop can decrease the amount of spherical aberration induced by a large pupil and thereby improve nighttime quality of vision (Figure 2).
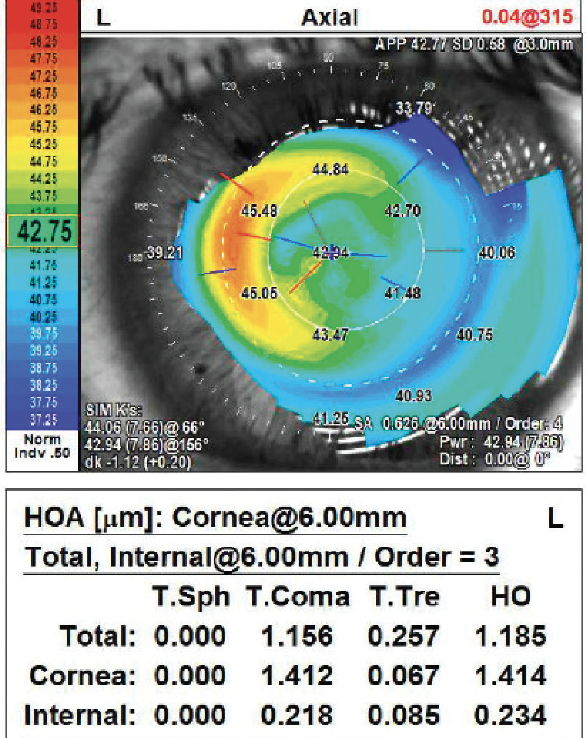
Figure 2. Topography of a patient 1 month after a PRK enhancement for a hyperopic refractive surprise after SMILE. Note the increased HOA values. Pinhole testing in the clinic demonstrated an improvement in acuity and sensation of blur around objects. An off-label trial of a pupil-modulating drop improved the patient’s quality of distance and near vision in the interim as his refraction stabilized.
CONCLUSION
The number of pupil-modulating drops on the US market is set to increase in the next few years. Many of these agents are being developed for presbyopia correction, but clinicians have an opportunity to use the products off label for the benefit of patients with dysphotopsias and irregular corneas.
The advantages of a pupil-modulating drop in the situations described here are that the therapy is noninvasive and can be customized and titrated to enhance the patient’s quality of vision.
1. Shajari M, Mackert MJ, Langer J, et al. Safety and efficacy of a small-aperture capsular bag-fixated intraocular lens in eyes with severe corneal irregularities. J Cataract Refract Surg. 2020;46(2):188-192.
2. Jackson MA, Giyanani J, Shabaik Y, et al. In vitro and in-eye comparison of commercial pilocarpine ophthalmic solution and an optimized, reformulated pilocarpine for presbyopia treatment. Ophthalmol Ther. Published online March 2, 2022. doi:10.1007/s40123-022-00482-2
3. Langer J, Shajari M, Kreutzer T, Priglinger S, Mayer WJ, Mackert MJ. Predictability of refractive outcome of a small-aperture intraocular lens in eyes with irregular corneal astigmatism. J Refract Surg. 2021;37(5):312-317.
4. Grabner G, Ang RE, Vilupuru S. The small-aperture IC-8 Intraocular lens: a new concept for added depth of focus in cataract patients. Am J Ophthalmol. 2015;160(6):1176-1184.e1.