
The correction of corneal astigmatism with toric IOLs has become a standard of care and a means to improve refractive outcomes after cataract surgery. However, the results are not always predictable: Surgically induced astigmatism, toric IOL misalignment, corneal astigmatism measurements, and the method of calculation have all been described as factors that might contribute to unexpected residual astigmatism. This article focuses on the latter two.
TWO KEY COMPONENTS OF OPTIMAL CORRECTION
Optimal correction of astigmatism requires two key components: accurate measurement of the cornea and a reliable method to calculate toric IOL power.
Accurate measurement of the cornea. Most devices that measure corneal astigmatism are based on anterior corneal measurement; however, some measure the posterior cornea as well. Also, not all biometry devices measure at the same location, and some have better repeatability and accuracy than others (see The Power of Repeatability).
Being familiar with the measuring devices available at your practice, including their features, strengths, and weaknesses, is therefore invaluable. It is also important to be critical when evaluating your measurements and to try not to cruise on automatic pilot mode. One helpful tip is to rely on validation criteria checklists such as the one available on http://doctor-hill.com/lenstar_haag_streit/lenstar_main.htm. When determining the power and meridian of the corneal astigmatism, the first step is to verify if it is symmetrical regular astigmatism. If so, it is advisable to follow the methodology of Warren E. Hill, MD,1 and to use primary and secondary supporting instruments to verify the steep meridian. The same process also should be repeated for the power difference between the meridians (Figure 1).

Figure 1. The use of primary and secondary supporting instruments is recommended to verify the steep meridian (A). The same process should be repeated for the power difference between the meridians (B).
A reliable method to calculate toric IOL power. In addition to proper and reproducible measurements, the method for calculating the toric IOL power plays a key role in achieving accurate prediction results. Some of the standard toric IOL calculators still use a fixed ratio to determine the toric IOL power at the corneal plane. However, even with a commercial toric IOL calculator that uses an anticipated effective lens position (ELP) to predict the toric IOL power at the corneal plane, our results were not optimal.2-4
A REFINED UNDERSTANDING
Douglas D. Koch, MD, highlighted the role of the posterior cornea in assessing the net corneal astigmatism in 2012,5 questioning the validity of the traditional method to determine the corneal astigmatism. In short, with the traditional method, devices measure only the anterior corneal curvature and assume that the ratio of the front and the back curvature of the cornea is constant. Alternatively, the Baylor toric nomogram, subsequently described by Koch at el,6 is based on a regression analysis derived from direct posterior corneal astigmatism measurements7 and addresses this issue by taking into account the effect of the posterior cornea in the presence of with-the-rule (WTR) and against-the-rule (ATR) corneal astigmatism. The nomogram can be used in conjunction with standard toric IOL calculators.
Since then, a great deal of work has been done to refine our understanding of posterior corneal astigmatism and to improve our precision when incorporating this into toric IOL planning. This includes:
- The use of intraoperative aberrometry;
- The use of standard toric calculators with a nomogram like the Baylor,5 or direct measurements of the posterior cornea;3
- The use of the Barrett toric calculator, which, based on the Universal II formula, takes into account the ELP and includes a mathematical model that calculates the estimated net corneal astigmatism by using anterior corneal–based measurements (the full version of the Barrett toric calculator is currently available on the Lenstar LS 900 [Haag-Streit] and at http://www.ascrs.org/barrett-toric-calculator and http://www.apacrs.org/); and
- The use of standard toric calculators with a correction formula like the Abulafia-Koch.2 This formula was developed based on a vector regression model, in order to convert anterior corneal–based measurements to an estimated net corneal astigmatism, hence it can easily be used as an add-on to any standard toric calculator.
THE CAUSES OF UNEXPECTED OUTCOMES
In a study conducted at Ein-Tal Eye Center, and in collaboration with Drs. Barrett and Koch and Li Wang, MD,7 we evaluated a cohort of 68 eyes and examined the two factors that we thought could contribute to unexpected outcomes with toric IOLs: (1) the method of measuring corneal astigmatism and (2) the method of predicting the required power and axis of a toric IOL.
The purpose of this study was to compare the error in predicted residual astigmatism for different corneal measurement devices and several methods of toric IOL calculation. We found that the Lenstar LS 900 and IOLMaster 500 (Carl Zeiss Meditec) were superior to the Atlas Corneal Topographer (Carl Zeiss Meditec) and that the online and commercial toric IOL calculators adjusted with the Baylor nomogram and the Barrett toric calculator were superior to the online and commercial toric calculators on their own. The most accurate prediction of residual astigmatism was achieved with the Barrett Toric IOL calculator in combination with the Lenstar LS 900 (Figure 2).
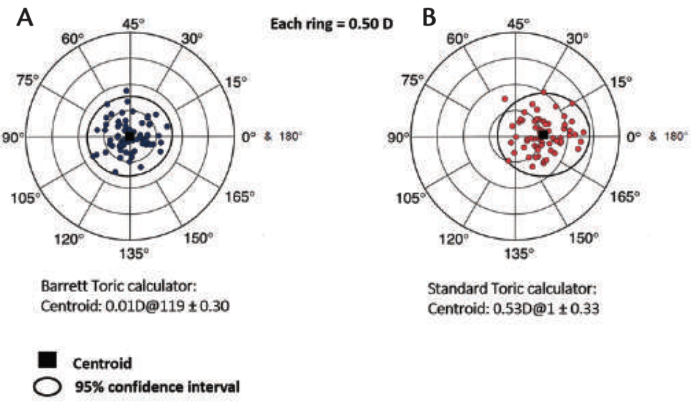
Figure 2. Double-angle plots of errors in predicted residual astigmatism with the Barrett Toric IOL calculator (A) and a standard toric calculator (B) using the Lenstar LS 900 measurements.
In an additional study, we found that standard toric IOL calculators with anterior corneal-based keratometry adjusted by the Abulafia-Koch formula had significantly reduced errors in the prediction of residual astigmatism in toric IOL calculations to a level similar to that of the Barrett toric calculator without adjustments (Figure 3).8
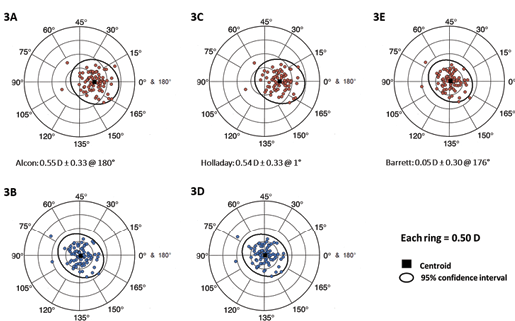
Figure 3. Double-angle plots of errors in predicted residual astigmatism using the IOLMaster 500. The Alcon toric calculator with no adjustments (A) and adjusted by the Abulafia-Koch formula (B); the Holladay toric calculator with no adjustments (C) and adjusted by the Abulafia-Koch formula (D); the Barrett toric calculator with no adjustments (E).
A subsequent study compared the accuracy of direct corneal astigmatism measurements with the Pentacam (Oculus) and a commercial toric calculator to the IOLMaster 500 with the Barrett toric calculator.3 Results in the 99 enrolled eyes showed that the Barrett toric calculator had a lower median absolute and centroid prediction error than direct measurements of the net corneal astigmatic power (Figure 4). These results suggest that using direct measurements of the posterior cornea with this device may not be accurate enough at this stage and should be addressed with caution.
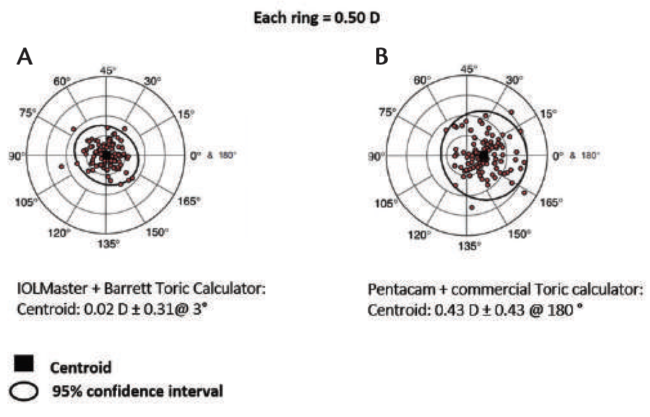
Figure 4. Comparison of the Barrett Toric calculator to direct corneal astigmatism measurements: IOLMaster 500 and Barrett toric calculator (A) vs Pentacam and commercial toric calculator (B).
THE POWER OF REPEATABILITY
1. Belkin A. Repeatability of corneal astigmatism measurements. Paper presented at: the ESCRS Annual Meeting; September 5-9, 2015; Barcelona, Spain.
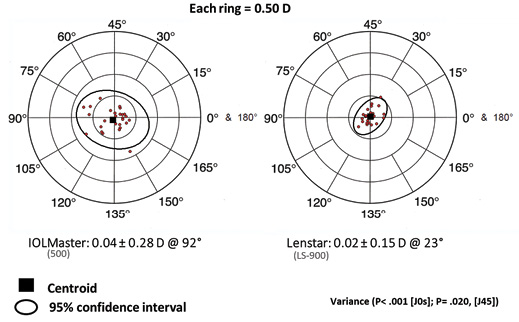
Figure 1. The absolute astigmatism power difference with the IOLMaster 500 and the Lenstar LS 900.
CONCLUSION
Today, my preferred method for preforming routine toric IOL calculation is to use high-quality corneal astigmatism measurements with several measuring devices combined with either the Barrett Toric calculator or a standard toric IOL calculator that takes into account the ELP with the Abulafia-Koch formula adjustments.
1. Hill WE. The preoperative management of corneal astigmatism. Paper presented at: the American Academy of Ophthalmology annual meeting; October 16, 2016; Chicago.
2. Abulafia A, Koch DD, Wang L, et al. New regression formula for toric intraocular lens calculations. J Cataract Refract Surg. 2016;42:663-671.
3. Abulafia A, Hill WE, Franchina M, Barrett GD. Comparison of methods to predict residual astigmatism after intraocular lens implantation. J Refract Surg. 2015;31:699-707.
4. Abulafia A, Barrett GD, Kleinmann G, et al. Prediction of refractive outcomes with toric intraocular lens implantation. J Cataract Refract Surg. 2015;41:936-944.
5. Koch DD. Corneal optics for IOL selection: Cracking the code. Paper presented at: the ASCRS annual meeting; April 20-24, 2012; Chicago.
6. Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: Effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39:1803-1809.
7. Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080-2087.
8. Abulafia A, Barrett GD, Kleinmann G, et al. Prediction of refractive outcomes with toric intraocular lens implantation. J Cataract Refract Surg. 2015;41:936-944.

