
Cataracts are a part of the normal aging process. Patients with diabetes, however, tend to develop cataracts at a younger age than their nondiabetic counterparts. Often, these patients are still busy raising their families, working full time, and driving at night when they begin to develop the signs and symptoms of cataracts. Those with poor HbA1c control and end-stage organ damage (eg, kidney, cardiac, or peripheral vascular disease) may experience even earlier cataract formation. These patients can also have some degree of ocular ischemia or other forms of retinal pathology including diabetic retinopathy and diabetic macular edema (DME) that the surgeon will have to address before cataract surgery.
BACKGROUND AND CHARACTERISTICS
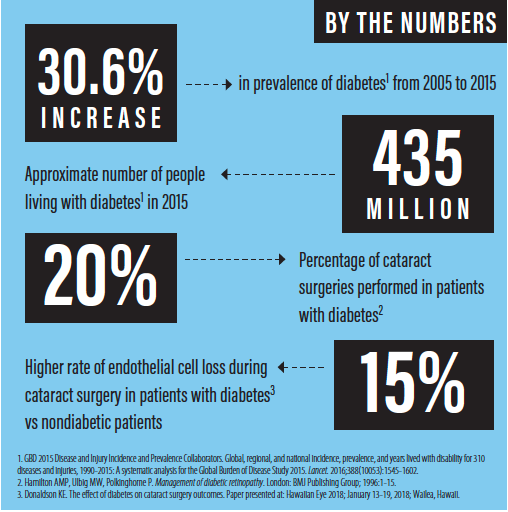
Diabetes mellitus is one of the most prevalent and morbid chronic diseases, affecting millions of individuals worldwide. The Global Burden of Disease study reported that the prevalence of diabetes rose 30.6% from 2005 to 2015—from about 333 million people to 435 million worldwide.1 Three large-scale population-based studies have shown an increased association between diabetes and cataract.2-4 An increased incidence of late-onset type 2 diabetes has also been noted.5 Overall, it is estimated that up to 20% of cataract surgeries are performed in patients with diabetes.6
Anterior segment changes in patients with diabetes who present for cataract surgery can include increased epithelial fragility, reduced corneal sensitivity, altered epithelial and endothelial barrier functions, and impaired corneal wound healing.7 Further, accumulation of glycogen can lead to miosis and poor pupillary dilation during cataract surgery.8
Patients with diabetes tend to have smaller pupils, and a small pupil can lead to longer surgery and potential complications such as vitreous loss or endothelial cell damage. The surgeon should also be aware that these eyes may have previously undergone laser procedures, vitrectomy, or intravitreal injections. Eyes with previous vitrectomy can have weakened zonules, which is yet another potential risk factor for increased complications during cataract surgery. Although the incidence is rare, it is important to note that a history of intravitreal injection can be associated with damage to the posterior capsule, leading to an increased risk of dropped lens material.
MY PROTOCOL
For all patients with diabetes, I perform macular OCT to rule out maculopathy. If maculopathy is identified, it should be discussed with the patient and possibly treated before cataract surgery. I also plan to take these cases just a little more slowly than normal, placing capsular tension rings or iris hooks to improve visualization if pupil size is limited. I may place a Malyugin Ring (MicroSurgical Technology) to achieve pupillary expansion.
In patients with poor red reflex, I often use trypan blue dye to enhance visualization. Another adjunctive tool that can facilitate surgery in patients with diabetes is intraoperative phenylephrine and ketorolac ophthalmic solution 1%/0.3% (Omidria, Omeros) to maintain pupil size. I often use laser cataract surgery in these patients to decrease the energy needed for phacoemulsification.
I have found the miLoop (IanTech) to be a helpful tool in patients with diabetes, particularly in those with very dense cataracts. This microinterventional device uses a nitinol filament to ensnare and dissect nuclei of any grade without causing capsular stress. The miLoop helps me to reduce the amount of energy used in grooving during phacoemulsification, and it lessens the need for manipulation of the lens in eyes with weakened zonules.
ENDOTHELIAL IMPLICATIONS
Although this does not receive much attention, individuals with diabetes have on average lower endothelial cell counts than nondiabetic individuals.9 Earlier this year, I presented the results of a study in which my colleagues and I found that the rate of endothelial cell loss during cataract surgery was statistically significantly higher in patients with diabetes (15%) than in nondiabetic patients.10 This study included 70 patients with diabetes and 70 without, tightly matching them for as many variables as possible, including age, density of cataract, axial length, anterior chamber depth, and preoperative endothelial cell density.
Because patients with diabetes may have delayed healing after cataract surgery—in part owing to endothelial cell loss—surgeons should discuss this possibility with patients before surgery. If you anticipate a problem, it is always better to communicate beforehand.
In uncomplicated cases, patients should be maintained on a topical NSAID for 1 month postoperatively, with longer duration if there is a history of DME. These are high-risk patients, so it is important that they be adequately treated. If the patient is not recovering as expected, postoperative macular OCT should be considered to rule out DME.
CONCLUSION
Rates of both diabetes and cataract are rising with the increasing age of the population. As noted earlier, it is estimated that about 20% of cataract surgeries are performed in patients with diabetes. These individuals present surgeons with a host of additional considerations regarding their surgery and the complications that can arise. Fortunately, we have access to a growing array of surgical tools, techniques, and medications to help ensure that patients with diabetes can enjoy successful, complication-free outcomes and good functional vision.
1. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-1602.
2. Klein BEK, Klein R, Wang Q, Moss SE. Older-onset diabetes and lens opacities. The Beaver Dam Eye Study. Ophthalmic Epidemiol. 1995;2:49-55.
3. Rowe NG, Mitchell PG, Cumming RG, Wans JJ. Diabetes, fasting blood glucose and age-related cataract: The Blue Mountains Eye Study. Ophthalmic Epidemiol. 2000;7:103-114.
4. Mukesh BN, Le A, Dimitrov PN, et al. Development of cataract and associated risk factors: the Visual Impairment Project. Arch Ophthalmol. 2006;124:79-85.
5. Klein BEK, Klein R, Moss SE. Incidence of cataract surgery in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Am J Ophthalmol. 1995;119:295-300.
6. Hamilton AMP, Ulbig MW, Polkinghorne P. Management of Diabetic Retinopathy. London: BMJ Publishing Group; 1996:1-15.
7. Sanchez-Thorin JC. The cornea in diabetes mellitus. Int Ophthalmol Clin. 1998;38:19-36.
8. Yanoff M, Fine BS, Berkow JW. Diabetic lacy vacuolation of iris pigment epithelium; a histopathologic report. Am J Ophthalmol. 1970;69(2):201-210.
9. He X, Diakonis VF, Alavi Y, Yesilirmak N, Waren D, Donaldson K. Endothelial cell loss in diabetic and nondiabetic eyes after cataract surgery. Cornea. 2017;38(8):948-951.
10. Donaldson KE. The effect of diabetes on cataract surgery outcomes. Paper presented at: Hawaiian Eye 2018; January 13-19, 2018; Wailea, Hawaii.


