IOP elevation in eyes with primary open-angle glaucoma (POAG) is caused by the alteration of tissue within three structures of the eye: the trabecular meshwork (TM), Schlemm canal, and distal collector channels.1-4 These mechanisms of change within the trabecular outflow pathway increase aqueous outflow resistance. Approximately 50% to 70% of total outflow resistance in glaucomatous eyes occurs within the TM,1,2 and 30% to 50% within Schlemm canal and the collector channels.3,4
MIGS has transformed the way that we approach glaucoma care, and in many cases it is the preferred management strategy for patients with POAG. Various MIGS techniques can be used to target aqueous outflow resistance in one or two structures at best. Goniotomy, trabeculotomy, and trans-TM implants address TM resistance, whereas canaloplasty, viscodilation, and some stenting procedures address Schlemm canal and/or the collector channels.5-8 A standalone procedure targeting all three mechanisms could effectively reduce IOP by removing all sources of aqueous outflow resistance. The OMNI Surgical System (Sight Sciences) allows practitioners to perform two implant-free procedures and target all three points of resistance with one device. And it also allows us to intervene earlier in the disease state because the device’s indications for use are not restricted by disease severity.
RETROSPECTIVE ANAYLSIS
Study design. My colleagues and I recently conducted a study to characterize the reduction in IOP and IOP-lowering medication use following trabeculotomy and viscodilation with the OMNI Surgical System. The procedure was performed as a standalone intervention in eyes with medically uncontrolled mild-moderate open-angle glaucoma (OAG).
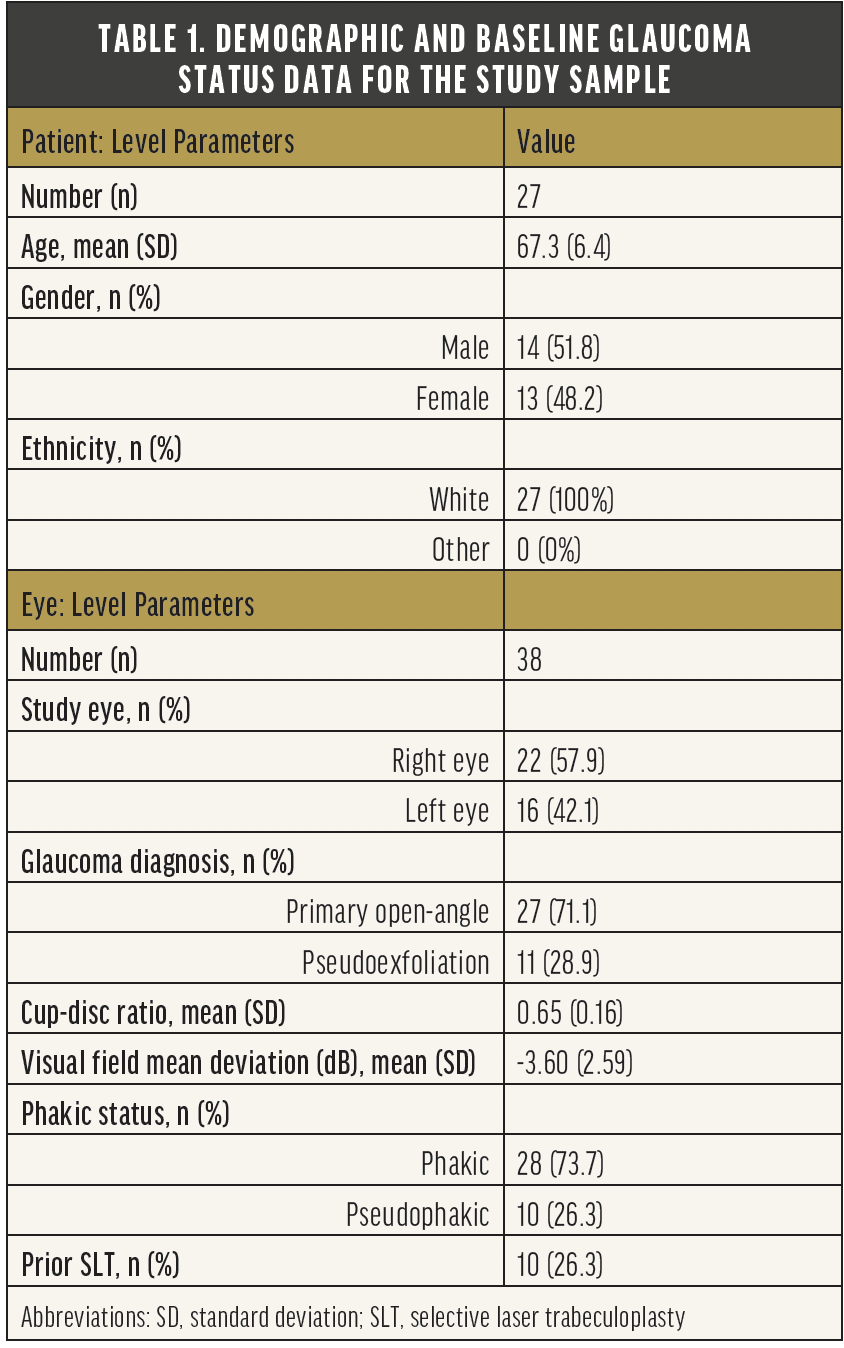
A total of 38 eyes (27 patients) were enrolled in this retrospective analysis (Table 1). Patients were approximately 67 years of age, with similar representation of both genders. Most (71%) had POAG of moderate severity (mean cup-disc ratio 0.65, mean visual field mean deviation -3.6 dB), most (74%) were phakic, and 26% had undergone prior selective laser trabeculoplasty.
Patients consecutively underwent MIGS with the OMNI since I began offering the procedure. IOP, medication use, and safety (intra- and postoperative adverse events and the need for additional surgery) data were collected preoperatively and at every postoperative visit through 12 months of follow-up.
Results. Mean (standard deviation) baseline IOP was 24.6 (3.0) mm Hg. Through 12 months of follow-up, this ranged from 12.6 to 14.7 mm Hg (P < .0001 at all time points), representing mean IOP reductions of 10.2 to 12.0 mm Hg (39.8% to 47.9%). Mean medication use was 1.9 (0.7) at baseline; through 12 months of follow-up, this ranged from 0.0 to 0.4 (P < .0001 at all time points), representing medication reductions of 1.4 to 1.9 per eye (70.6% to 100%). At Month 12, mean IOP was 14.7 mm Hg, a reduction of 10.1 mm Hg (39.8%; P < .0001). Also at that time point, 96.7% of eyes achieved IOP reduction of 20% or more from baseline, and mean medication use was 0.4 medications per eye, representing a reduction of 1.4 medications (70.6%; P < .0001). A total of 83.3% of eyes were using at least one less medication than at baseline, and 63.3% were medication-free (Tables 2 and 3 and Figure).
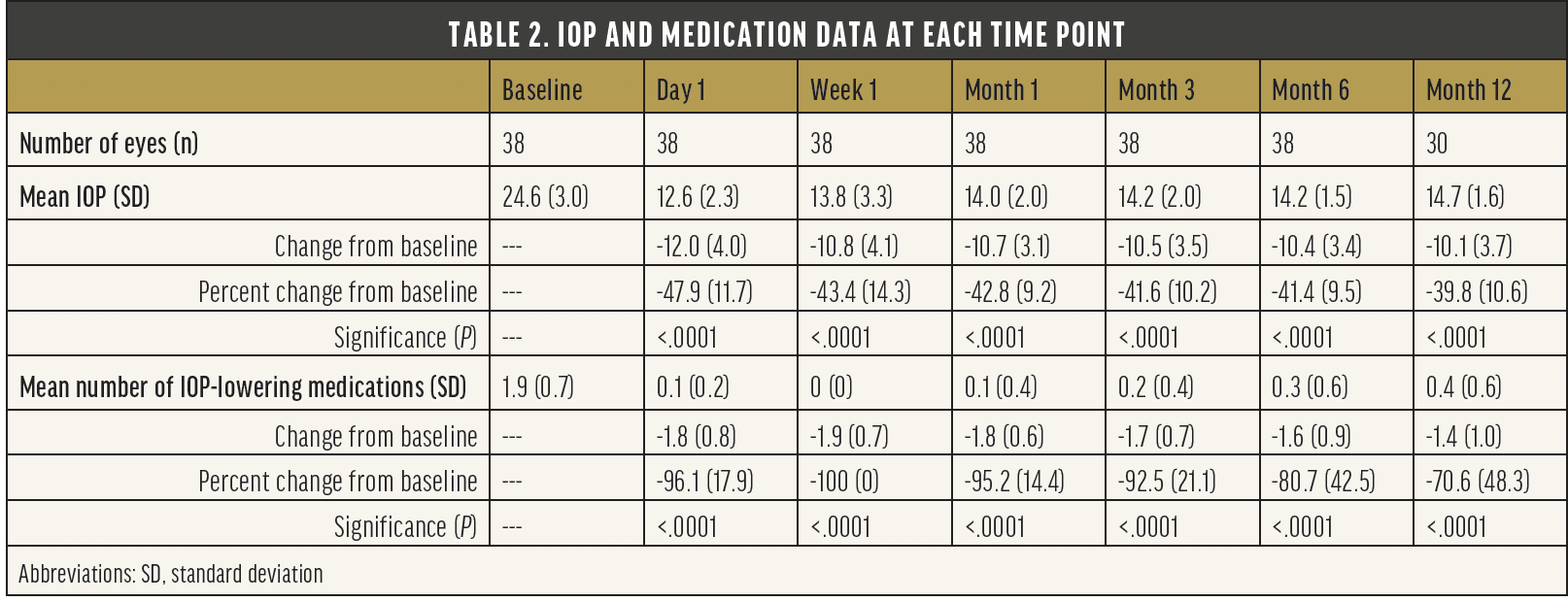
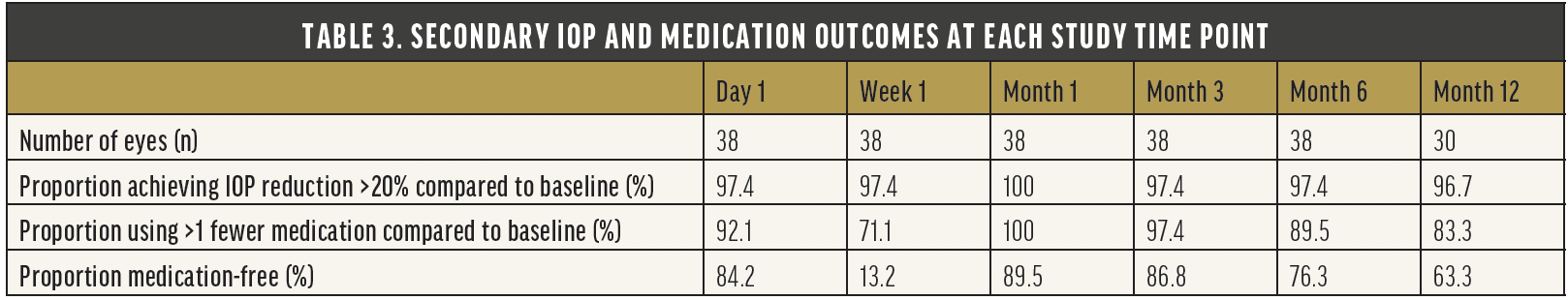
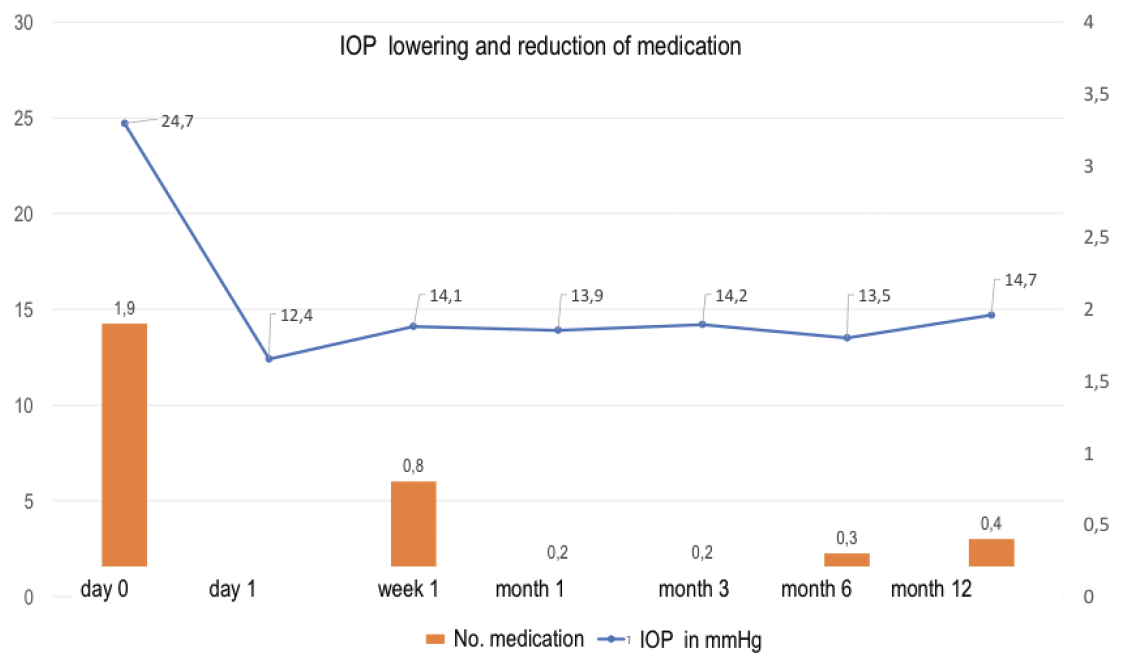
Figure. IOP-lowering effect and reduction of medication with the OMNI Surgical System.
Safety. The most common adverse event in this population of patients undergoing OMNI implantation for better control of IOP was intraoperative hyphema (44.7%); this resolved spontaneously in all cases. A transient lens touch associated with a shallow anterior chamber was seen in one eye (2.6%). No eyes required reoperation during follow-up.
Take-home points. This study confirmed that performing trabeculotomy and viscodilation with the OMNI Surgical System as a standalone procedure provides clinically relevant and statistically significant reductions in both IOP and the IOP medication burden. The study also highlighted the procedure’s excellent safety profile and established that it can be considered in phakic or pseudophakic eyes with mild to moderate OAG that require a safe and effective surgical intervention to achieve IOP reduction, medication reduction, or both.
CONCLUSION
Compared to other MIGS procedures, the combination of viscodilation and titrable trabeculotomy with the OMNI Surgical System addresses all three sources of physiological outflow resistance in a standalone procedure, which could result in longer-lasting IOP reduction.
1. Grant WM. Experimental aqueous perfusion in enucleated human eyes. Arch Ophthalmol. 1963;69:783-801.
2. Maepea O, Bill A. Pressures in the juxtacanalicular tissue and Schlemm’s canal in monkeys. Exp Eye Res. 1992;54:879-883.
3. Allingham RR, de Kater AW, Ethier CR. Schlemm’s canal and primary open angle glaucoma: correlation between Schlemm’s canal dimensions and outflow facility. Exp Eye Res. 1996;62:101-109.
4. Battista SA, Lu Z, Hofmann S, Freddo T, Overby DR, Gong H. Reduction of the available area for aqueous humor outflow and increase in meshwork herniations into collector channels following acute IOP elevation in bovine eyes. Invest Ophthalmol Vis Sci. 2008;49:5346-5352.
5. Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clinical Ophthalmology. 2016;10:189-206.
6. Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS ONE. 2017;12:e0183142.
7. Pillunat LE, Erb C, Junemann AG, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11:1583-1600.
8. Chen DZ, Sng CCA. Safety and efficacy of microinvasive glaucoma surgery. J Ophthalmol. 2017;3182935.

