

It’s no surprise that artificial intelligence (AI) is being steadily integrated into almost all areas of medicine. IOL power calculations are no exception. Hill-RBF (Radial Basis Function) is an advanced, self-validating method for IOL power selection that performs this task using AI-based pattern recognition.
PATTERN RECOGNITION
Since the introduction of IOLs, ophthalmology has struggled with accuracy for IOL power selection. This problem is primarily because the physical model does not always correspond to the predicted outcome. Additionally, there are millions of possible measurement combinations. Regrettably, no vergence formula or regression algorithm can consistently solve this problem at a level of accuracy we would all like to see.
On the other hand, Hill-RBF uses pattern recognition, which is independent of the effective lens position. Via this approach, IOL power is accurately calculated regardless of the eye’s axial length (AL) and configuration of the anterior segment. Compared to standard IOL calculation formulas, one additional advantage of Hill-RBF is that data are continuously acquired from 40 high-quality surgical sites worldwide. For each new version, additional information is added, validated, and then re-fit to the AI model, improving its accuracy’s overall breadth and depth.
NEW PREOPERATIVE MEASUREMENTS
Hill-RBF is available to use free of charge at www.RBFcalculator.com. The latest version of the calculator (version 3.0), released in December 2020, uses a highly refined data set that now incorporates the new parameters of lens thickness (LT), white-to-white (WTW), central corneal thickness (CCT), and gender, improving accuracy even for unusual anterior segments. Hill-RBF is also available on the Lenstar and Eyestar (both from Haag-Streit).
IMPROVED ACCURACY
For normal eyes, on average, cataract surgeons are within ±0.50 D of the intended spherical equivalent for 80% of cases. In comparison, some more experienced surgeons obtain an accuracy between 84% and 90% of patients. When the accuracy of the intended refraction is lowered to ±1.00 D, typically 98% of cases are within the range (Figure 1).
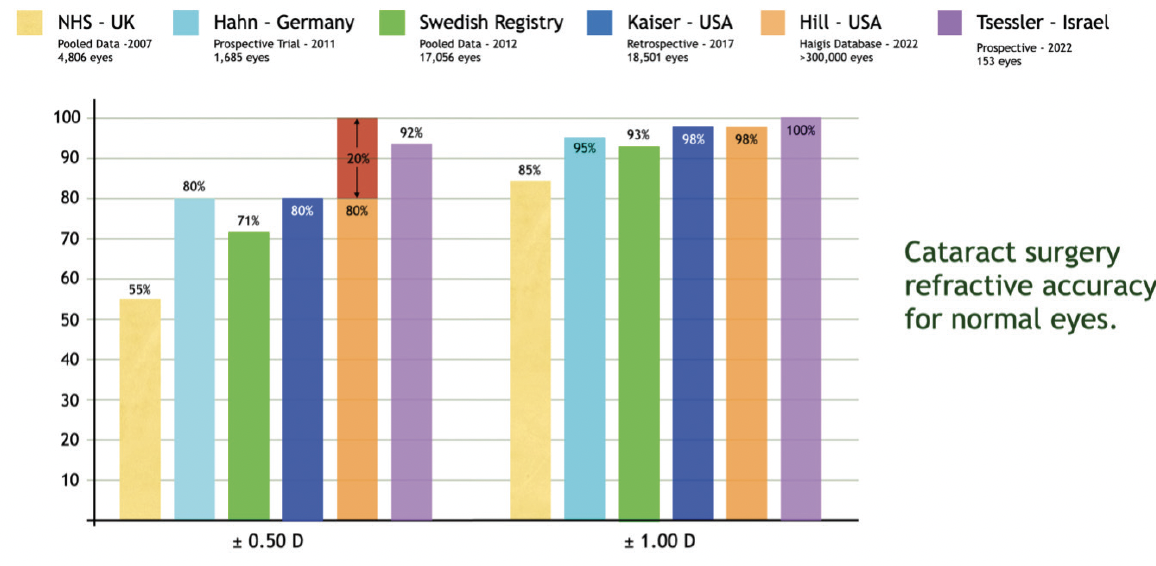
Figure 1. Results from six significant studies show that, on average, cataract surgeons are within ±0.50 D of the intended refraction in 80% of routine cases.1-6
As the size of the AI database increases, not only does the overall accuracy increase, but the number of out-of-bounds cases also decreases. For version 3 of Hill-RBF, the number of out-of-bounds cases for the typical surgeon has now dropped to 2.5%. For version 3, the range of calculation accuracy was also increased for biconvex IOLs up to +34.00 D and meniscus design IOLs down to -5.00 D.
The best accuracy for version 3 is when all eight variables have been entered: AL, keratometry (K), ACD, LT, CCT, WTW, target spherical equivalent, and gender. The calculation also can be carried out with slightly less accuracy if the LT, CCT, and gender are omitted.
ACCURACY VALIDATION
In a retrospective multicenter study of 459 consecutive patients of IOL power calculation performed with Hill-RBF, a ±0.50 D accuracy was achieved in 91% of all eyes (AL, 20.97–29.10 mm), 92.2% of normal eyes (AL, >22.5 mm and <25.0 mm), 98.4% in eyes with axial myopia (AL, >25.0 mm), and 84.5% in eyes with axial hyperopia (AL, <22.5 mm). The mean absolute error for each group was 0.29, 0.30, 0.20, and 0.32 D, respectively.
BOUNDARY MODEL ACCURACY PREDICTION
After entering the required measurements by biometry, a target spherical equivalent, and some basic information about the IOL, including its lens constant, Hill-RBF will accurately determine the recommended IOL power. A feature unique to this calculation method is that it will also predict the postoperative refractive accuracy. This is possible due to the ability to sample the accuracy edge of six pair-wise boundary models, such as AL versus ACD or central corneal power versus the target spherical equivalent (Figure 2). For Hill-RBF, the ±0.50 D accuracy edge is set at a 90% level. If all preoperative measurements fall within each of the six pair-wise boundary models, the calculation is termed in-bounds. However, if any preoperative measurements fall outside one or more boundary models, the user is flagged, and an out-of-bounds calculation is indicated. An in-bounds indication suggests a 90% chance of sufficient data for a ±0.50 D accuracy. A quick way to be outside one of the boundary models is to select an unusual target spherical equivalent, such as +3.50 D. It is doubtful that there are an adequate number of cases within the AI database with an observed, highly hyperopic refractive outcome.
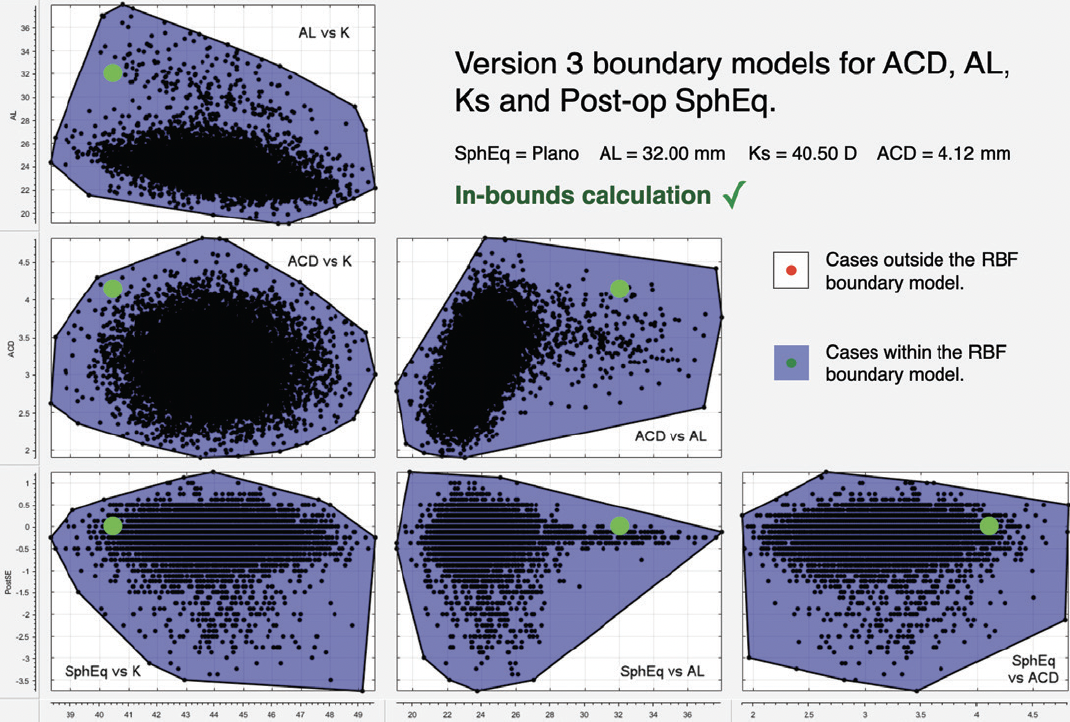
Figure 2. Graphic illustrating the concept of boundary models. The data for this case represents a highly unusual eye with extreme axial myopia, flat keratometry, and a very deep anterior chamber. Despite these highly unusual preoperative measurements, the calculation with Hill-RBF version 3.0 would still be in-bounds and have a 90% chance of being within ±0.50 D of the target spherical equivalent.
The Hill-RBF method has been optimized using Lenstar data. Aside from the online calculator, Hill-RBF is also available within the Lenstar and the Eyestar biometers. The online calculator may also be used with biometry data from other devices. By using this free calculator, surgeons can improve their confidence with IOL power calculation parameters for eyes with both in- and out-of-bound measurements. Additionally, Hill-RBF enables surgeons to identify unusual cases at a glance when an out-of-bounds indication appears. When this happens, a meaningful preoperative conversation begins with the patient to alert them that some unique aspect of their eye(s) may preclude a predictable result.
CONCLUSION
Ophthalmology is experiencing a convergence of technologies for IOL power selection that are helping all of us achieve better outcomes. Many methods now produce excellent results. However, the method with the greatest sensitivity and flexibility will end up as the leader. Haag-Streit has been firmly committed to ongoing research in this area for more than a decade (Figure 3).
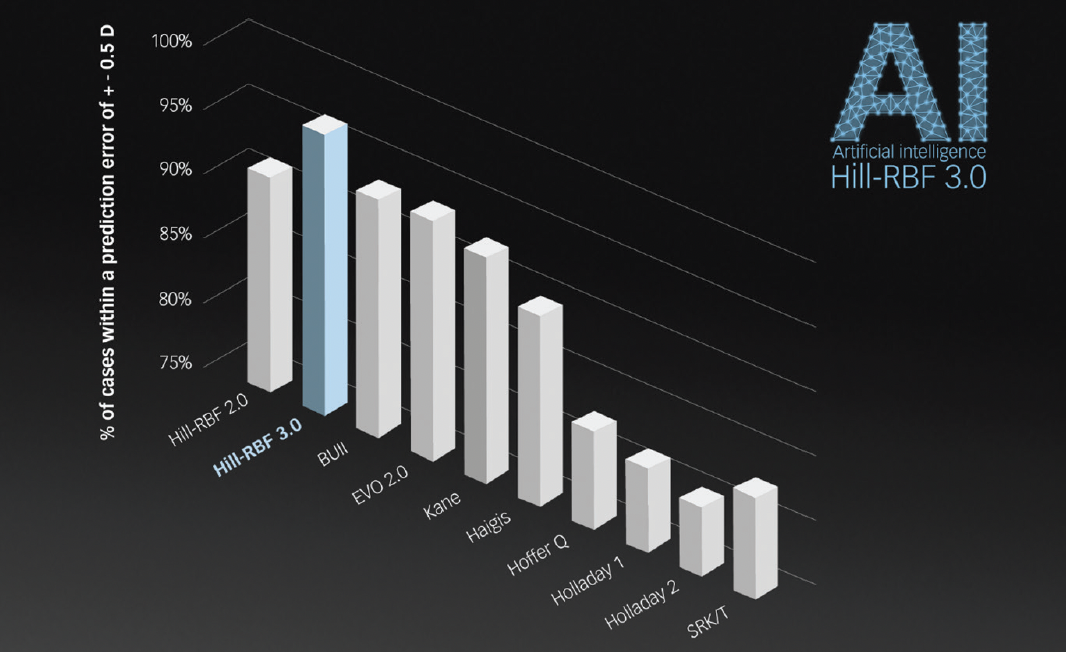
Figure 3. Results of a recent study of 153 eyes by Adi Abulafia, MD, and colleagues showed that Hill-RBF 3.0 performed significantly better than its predecessor. It further showed best prediction in the comparison. (Tsessler M, Cohen S, Wang L, Koch DD, Zadok D, Abulafia A. Evaluating the prediction accuracy of the Hill-RBF 3.0 formula using a heteroscedastic statistical method. J Cataract Refract Surg. 2022;48(1):37-43.)

