

LASIK is a wonderful technique that has enabled millions of people to enjoy spectacle independence and improved UCVA over the past 20 years. Post-LASIK ectasia is a rare (estimated prevalence, less than 1 in 2,000) but potentially sight-threatening complication. The main risk factor for post-LASIK ectasia is the presence of undetected early forms of subclinical keratoconus.1,2 Therefore, improving the sensitivity and specificity of automated techniques for preoperative screening with corneal topography is a valuable goal in refractive surgery.3-6
Initially, Placido-disc–based detection indices derived from specular anterior corneal topography were judged the most sensitive and specific to detect the earliest forms of subclinical keratoconus.7-9 These indices were based solely on the analysis of the specular reflection of Placido mires on the anterior surface of the cornea. They ignored posterior corneal topography and variations in corneal thickness.
AT A GLANCE
• In refractive cataract surgery, priorities include safety, refractive correction targeting spectacle-free visual function in daytime and nighttime and at all distances, and a fully customized procedure for each patient.
• The concept of the SCORE Analyzer originated from the authors’ aim to provide clinicians with a unique number to rate the ectasia susceptibility of myopic eyes by using linear discriminant analysis.
• Study results confirmed that the combination of Placido, elevation, and tomography data is a more sensitive and specific detector of early subclinical keratoconus than either Placido-disc topography or elevation data alone.
The main risk factor for post-LASIK ectasia is the presence of undetected early forms of subclinical keratoconus; therefore, improving the sensitivity and specificity of automated techniques for preoperative screening with corneal topography is a valuable goal in refractive surgery.
The Orbscan subsequently became one of the corneal topographers most commonly used to screen LASIK candidates. Many surgeons soon found that the information derived from the posterior surface elevation and tomography mapping was both informative and useful to better identify at-risk corneas, as compared with anterior surface topography alone. However, these conclusions were based on limited case series, empirical observations, and subjective interpretations, and some controversy remained regarding the real benefits of mapping the whole cornea.
One reason for this lack of full acceptance could be explained by the fact that, despite the widespread use of Orbscan maps, no quantitative computed indices were available with the instrument’s software. On the other hand, the use of this tool persisted despite the later introduction of topographers that were based on Scheimpflug technology.

Figure 1. Early attempts to configure the GUI for the SCORE Analyzer (2011). At this stage, there was no RADAR map. Thickness profile curves were planned but not yet available. The sample shown here used elements copied/pasted from Pentacam output (A). In a slightly more advanced design (B), the values of three other selected parameters were added in the form of color-scale bars and for the global SCORE value, which is computed from discriminant analysis using a total of 12 indices. This SCORE value would later be used as an eponymous denomination for this software tool.
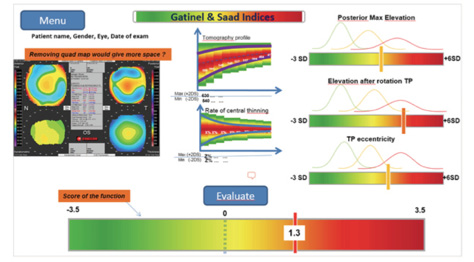
Figure 2. In this later GUI proposal, Gaussian bell curves were added to the bars in order to visually locate the value of the analyzed parameter within its statistical distribution among various groups. The problem was that, in practice, these curves were not as well separated as they appear on the graphs—the green (normal) and orange (forme fruste keratoconus) curves being almost superimposed.
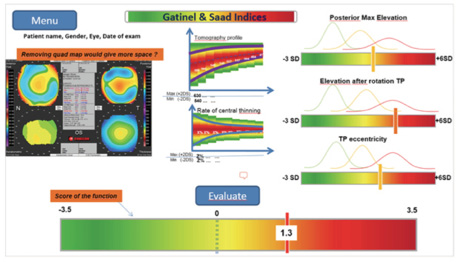
Figure 3. The first handmade conceptual sketch for the RADAR (left), which evolved into the final RADAR map display (right) without significant modifications. This display instantaneously provides the clinician with a colored flag—in this example, a green flag.
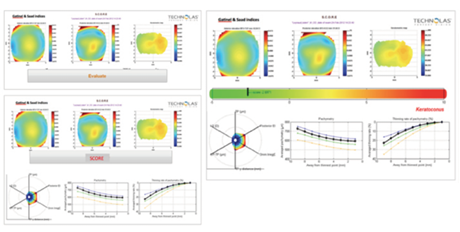
Figure 4. Shown here are the last iterations of the SCOPE Analyzer before the GUI was finalized (see Figure 5), incorporating pachymetry curves, RADAR map, and SCORE bar.
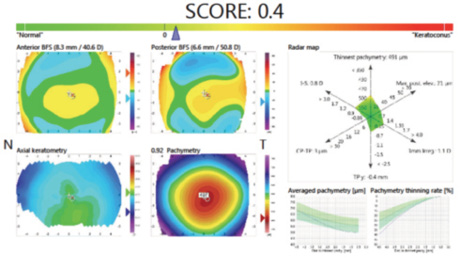
Figure 5. The final SCORE Analyzer GUI was released in 2011. In this example, the SCORE is just barely positive, so the implicit recommendation would be to reconsider the LASIK indication. The RADAR map highlights the borderline values of most indices (especially the thinnest point value), and the pachymetry curves are abnormal.
TOWARD A NEW TOOL
In 2009, we embarked on a project to address the specific challenge of early subclinical detection.11,12 To do this, we would need a clinical decision tool to improve the safety of refractive surgery.
Combining a pertinent clinical model (eyes with low but proven expression of early subclinical keratoconus) with a pertinent statistical method (discriminant analysis), we demonstrated without any ambiguity that posterior elevation and pachymetry values, combined with anterior topography data, provided better sensitivity and specificity for early subclinical keratoconus detection than anterior topography alone.3
CONCEPT OF THE SCORE ANALYZER
The concept of the Screening Corneal Objective Risk of Ectasia (SCORE) Analyzer (Bausch + Lomb Technolas) originated from our aim to provide clinicians with a unique number to rate the ectasia susceptibility of myopic eyes by using linear discriminant analysis. It has been evaluated as described in published and peer-reviewed forums.3,13 Key observations of our study include the following:
• The combination of anterior surface irregularity indices alone can be used with great accuracy only to detect keratoconus; it is insufficient to provide acceptable accuracy for the detection of early subclinical keratoconus.
• Only the combination of different Placido-derived and tomography indices in a discriminant function provided good accuracy (92% specificity and 92.5% sensitivity) in differentiating healthy corneas from those with subclinical keratoconus. The same combination of indices also provided 100% specificity and 97% sensitivity for differentiating between normal and keratoconic corneas.
• The spatial thickness profile indices and maximum posterior corneal elevation were the most important contributors to the discriminant function.
• The indices generated from corneal thickness and curvature over the entire cornea and the calculations of percentage of thickness increase and anterior and posterior curvature variation from the thinnest point to the periphery were able to identify even mild forms of keratoconus undetected by topography.
• Because of overlap in parameters between healthy and pathologic corneas, no single parameter can sufficiently distinguish a healthy cornea from a suspect cornea.
These results confirmed that the combination of Placido, elevation, and tomography data is a more sensitive and specific detector of early subclinical keratoconus than either Placido-disc topography or elevation data alone. Including elevation and tomography data with other measurements, such as corneal biomechanics or wavefront sensing, could further increase the sensitivity and specificity of these tests for early subclinical keratoconus detection.
ALGORITHM FOR ORBSCAN
The development of the SCORE Analyzer required close collaboration with Technolas’ research and development department (later Bausch + Lomb Technolas), headed by Gerhard Youssefi, PhD, and the active participation of Hong Wei Zhang, PhD. They helped to refine the SCORE algorithm and define a new graphical user interface (GUI). These steps were completed between 2010 and 2011.
The SCORE Analyzer concept and its application were presented in various congresses and were awarded three Best Papers Awards (ASCRS 2011, ASCRS 2012, AAO 2012). The CE Mark was obtained in December 2013, and the first official copy of the commercial version of the SCORE Analyzer appeared in February 2014.
CONCEPTION OF THE GUI
We wanted to establish a clear connection between the graphical display of the SCORE Analyzer data and relevant topography elements that were incorporated in the calculation of the algorithm. The final conception of the SCORE Analyzer GUI augments the classic Orbscan quad-map display with three additional graphs: the SCORE bar, which visually locates the SCORE value on a linear color scale bar; the RADAR map display, which is a new visually appealing and efficient map to help the clinician to appreciate the value of six pertinent corneal topography-derived indices; and the averaged pachymetry and pachymetry thinning curves, which provide a meridionally averaged cross-sectional analysis of the corneal thickness profile.
Before the GUI was finalized in 2011, we explored a range of different versions. This creative process wandered in several directions as we imagined various sketch proposals. Some of these are described in the accompanying Evolution of the SCORE GUI on the following page.
POSTRELEASE STUDIES
We recently investigated the efficacy of the SCORE Analyzer in detecting forme fruste keratoconus (FFKC) in Asian eyes in order to validate its usefulness as a risk-assessment system for post-LASIK keratectasia.14
In that study, masked investigators retrospectively evaluated corneal topographies with the Orbscan IIz system and independently tested them with the SCORE Analyzer. Eyes were classified into two groups: the FFKC group, which included clinically and topographically healthy eyes with definite keratoconus in the contralateral eye, and the control group, which included eyes with LASIK performed at least 4 years prior with no resultant keratectasia and normal preoperative topographies.
A total of 128 Orbscan results for 128 Asian patients were analyzed. There were 24 FFKC eyes and 104 controls. In the FFKC group, SCORE was negative in seven eyes (false negative), and in the control group two were positive (false positive). Sensitivity in detecting FFKC in Asian eyes was 70.83%, and specificity was 98.08%. This implies that the SCORE Analyzer would unlikely wrongly identify healthy eyes and unnecessarily exclude them from LASIK.
The SCORE Analyzer algorithm, which was developed and validated using the eyes of white individuals, was found to be valid and consistent in Asian eyes, showing good sensitivity and specificity in FFKC detection. The authors concluded that the algorithm was useful in objectively identifying eyes at risk of post-LASIK keratectasia.
In another recent study, Reinstein et al assessed the
effectiveness of a keratoconus-detection algorithm derived from epithelial thickness maps of the fellow eye from a series of patients with unilateral keratoconus and compared this algorithm to the SCORE Analyzer and to the D score derived from a Schleimpflug device (Pentacam; Oculus).5 The study included 10 patients with moderate to advanced keratoconus in one eye but a clinically and algorithmically topographically healthy fellow eye.
Five of the 10 fellow eyes were classified as keratoconic by the algorithm derived from epithelial thickness mapping. Five of nine fellow eyes were classified as keratoconic by the SCORE model. For the five fellow eyes with available Pentacam analyses, none was classified by the Scheimpflug D score as keratoconic.
CONCLUSION
Retrospective analysis of eyes with post-LASIK ectasia for which Orbscan measurements were performed preoperatively (before the SCORE was created) is an objective
method to evaluate the efficiency of the SCORE algorithm. A multicenter study using this methodology is ongoing, and we hope that the results will further confirm the efficacy of the SCORE Analyzer as a means to prevent corneal
ectasia.
1. Binder PS, Trattler WB. Evaluation of a risk factor scoring system for corneal ectasia after LASIK in eyes with normal topography. J Refract Surg. 2010;26(4):241-250.
2. Randleman JB, Trattler WB, Stulting RD. Validation of the ectasia risk score system for preoperative laser in situ keratomileusis screening. Am J Ophthalmol. 2008;145(5):813-818.
3. Saad A, Gatinel D. Topographic and tomographic properties of forme fruste keratoconus corneas. Invest Ophthalmol Vis Sci. 2010;51(11):5546-5555.
4. Saad A, Gatinel D. Evaluation of total and corneal wavefront high order aberrations for the detection of forme fruste keratoconus. Invest Ophthalmol Vis Sci. 2012;53(6):2978-2992.
5. Reinstein DZ, Archer TJ, Urs R, et al. Detection of keratoconus in clinically and algorithmically topographically normal fellow eyes using epithelial thickness analysis. J Refract Surg. 2015;31(11):736-744.
6. Buhren J, Kook D, Yoon G, Kohnen T. Detection of subclinical keratoconus by using corneal anterior and posterior surface aberrations and thickness spatial profiles. Invest Ophthalmol Vis Sci. 2010;51(7):3424-3432.
7. Rabinowitz YS, Rasheed K. KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg. 1999;25(10):1327-1335.
8. Rabinowitz YS, McDonnell PJ. Computer-assisted corneal topography in keratoconus. Refract Corneal Surg. 1989;5(6):400-408.
9. Rabinowitz YS, Nesburn AB, McDonnell PJ. Videokeratography of the fellow eye in unilateral keratoconus. Ophthalmology. 1993;100(2):181-186.
10. Yaylali V, Kaufman SC, Thompson HW. Corneal thickness measurements with the Orbscan Topography System and ultrasonic pachymetry. J Cataract Refract Surg. 1997;23(9):1345-1350.
11. Klyce SD. Chasing the suspect: keratoconus. Br J Ophthalmol. 2009;93(7):845-847.
12. Mahon L, Kent D. Can true monocular keratoconus occur? Clin Exp Optom. 2004;87(2):126.
13. Saad A, Hodge C, Lawless M, Gatinel D. Retrospective testing of a new method for detecting ectasia-susceptible corneas. J Cataract Refract Surg. 2011;37(10):1907-1908.
14. Chan C, Ang M, Saad A, et al. Validation of an objective scoring system for forme fruste keratoconus detection and post-LASIK ectasia risk assessment in Asian eyes. Cornea. 2015;34(9):996-1004.
Damien Gatinel, MD
• Assistant Professor and Head, Anterior Segment and Refractive Surgery Department, Rothschild Ophthalmology Foundation, Paris
• Director, CEROC, Paris
• Member, CRST Europe Editorial Board
• gatinel@gmail.com
• Financial disclosure: Consultant (Bausch + Lomb Technolas)
Alain Saad, MD
• Fellow, Anterior Segment and Refractive Surgery Department, Rothschild Ophthalmology Foundation, Paris
• Vice-director, CEROC, Paris • dralainsaad@gmail.com
• Financial disclosure: Consultant (Bausch + Lomb Technolas)
