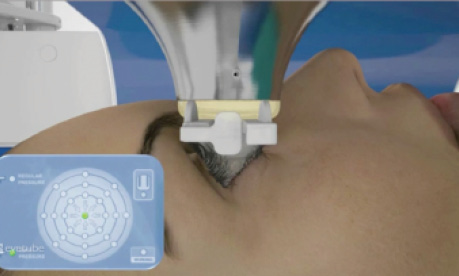
In less than a decade since it was first described in humans,1 laser-assisted cataract surgery (LACS) has become an essential part of many cataract surgeons’ armamentariums. The technology allows surgeons to reliably and reproducibly create clear corneal incisions and capsulotomies and to perform lens fragmentation before opening the patient’s eye.
AT A GLANCE
• Risk levels are increased in eyes with PXF, both intra- and postoperatively, and use of LACS can help to mitigate those risks.
• Cataracts in eyes with PXF should be treated sooner rather than later, in order to avoid having to perform surgery on a very advanced cataract with PXF.
• Because of the laser’s many benefits in cases with PXF, it has the potential to become a standard of care, especially if there are signs of zonular compromise.
In my practice, we routinely use LACS in selected cases, probably accounting for 20% to 25% of total cataract volume. I believe that certain patients clearly stand to benefit from the use of the laser, while for others I am not so sure the costs justify the expense. One example of patients who benefit from LACS is those with pseudoexfoliation (PXF). This article describes why I believe these patients are among the best candidates for LACS and details some of the considerations for its use in these cases.
BENEFITS OF LACS IN PXF
There are several reasons why LACS technology can provide benefits in eyes with PXF. Risk levels are increased in eyes with PXF, both intra- and postoperatively, and use of the laser can help to mitigate those risks.
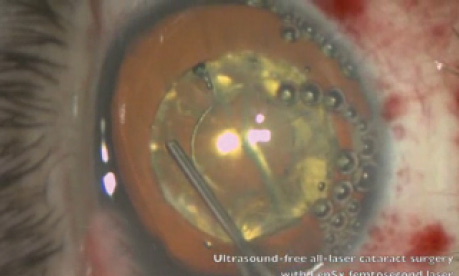
Intraoperative. First, in these eyes, there is often a lack of zonular integrity. The zonules may be lax or partially absent, so anything the surgeon can do to minimize the effect of surgery on the lens position is desirable. When a manual capsulorrhexis is created with forceps, we move the lens laterally and sometimes push it posteriorly, placing stress on the weakened zonules. This is the case even if the maneuvers are performed with great care. With the laser, by contrast, there is almost no displacement of the bag when the capsulotomy is made.
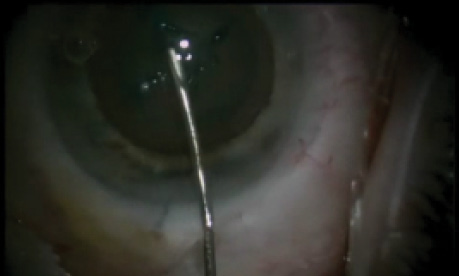
The same is true regarding the phacoemulsification portion of the procedure; we do not want to displace the bag any more than necessary when removing lens particles. Therefore, if we can presoften the lens with laser fragmentation before entering the eye with instruments, lens removal becomes less traumatic. (Editor’s Note: Check out the Watch It Now box on the following page for a sampling of Eyetube videos that demonstrate various laser fragmentation techniques.)
Postoperative. Another advantage of LACS is the ability to customize the size of the laser capsulotomy. Postoperatively, eyes with PXF tend to develop capsular phimosis, or late contraction of the anterior capsule. This causes increased tension on the zonules, and frequently late dislocations of the lens-bag complex are seen. In these cases, the whole lens-bag complex can shift out of position, even though the surgery went well and the IOL was initially beautifully centered in the capsular bag. One effort that can reduce that risk is placement of a capsular tension ring (CTR), which most surgeons do routinely in eyes with PXF. Another, however, is to make the capsulotomy larger than usual. With manual capsulorrhexis, attempting a larger diameter opening may increase the possibility of extension into the periphery. By contrast, with the laser, we can safely customize the capsulotomy to any size that fits within the dilated pupil.
SURGICAL CONSIDERATIONS
One challenge in eyes with PXF may be pupil dilation. In these eyes, getting the pupil dilated well enough to achieve a capsulotomy of even normal size, let alone a larger one as suggested above, can be difficult. If this is encountered, all the normal strategies for pupil dilation, including intracameral injection of phenylephrine 10%, are worth considering.
For the most part, the laser portion of surgery in these eyes is straightforward, as long as the lens is in a normal position and is not unduly tilted due to zonular loss. If the lens is significantly tilted, the surgeon might consider LACS only with caution because of the risk of intraoperative dislocation of the lens capsule. When LACS is performed, there is often exfoliative material on the capsule, but in my hands that has never impaired my ability to cut the capsule with the laser.
INSIST ON THE LASER
Another consideration, not just for LACS but for cataract surgery in the presence of PXF in general, is that these eyes should be treated sooner rather than later. The practice used to be that, in eyes with PXF, surgeons would wait until the latest possible stage for surgery. Unfortunately, there are still many ophthalmologists caring for patients with PXF who will tell them to delay having surgery. Then, when they finally come to us, these patients have very advanced stages of cataract with PXF—making the surgery a much higher-risk situation because now we have a hard cataract to remove with the additional disadvantage of PXF.
This is one more reason, when facing a case like this, why it is advantageous to have the laser: It takes a really hard case and makes it easier. In many cases of PXF, I insist on using the laser, and if the patient cannot afford it, I will pay the cost of the laser out of my own pocket. (In the United States, reimbursement for the tools we use in cataract surgery is set at one bundled rate, so there is no extra payment for use of advanced technology such as the femtosecond laser. The exception to this is for treatment of astigmatism at the time of cataract surgery, in which case there is extra payment for use of the laser as the tool used to make the astigmatism-correcting incisions.)
CONCLUSION
PXF is the one indication for using LACS that I feel most strongly about. I consider it an issue of providing the best quality of care. The laser conveys such a benefit in these cases that I believe it could easily become a standard of care to use LACS in patients with PXF, especially if there are signs of zonular compromise. I hope that my colleagues in Europe and elsewhere agree and that use of LACS in eyes with PXF will soon become a routine practice worldwide.
1. Nagy Z, Takacs A, Filkorn T, et al. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery.
J Refract Surg. 2009;25:1053-1060.
John A. Hovanesian, MD
• Private practice, Harvard Eye Associates, Laguna Beach, California
• Clinical Instructor, UCLA Jules Stein Institute, Los Angeles
• drhovanesian@harvardeye.com
• Financial disclosure: Consultant (Alcon, Abbott Medical Optics, Bausch + Lomb)