
After performing CXL for the past 9 years at the Bochner Eye Institute in Toronto, the procedure of choice for my colleagues and me has evolved to the combination of topography-guided PRK (TG-PRK) and CXL.1,2 CXL alone can stabilize an ectatic cornea, but improvement in BCVA is often limited.3 CXL can only flatten a steep area of the cornea; it cannot steepen a flat area. Consequently, the procedure is not as effective at regularizing the corneal surface and improving BCVA as the combined procedure.
AT A GLANCE
• The combination of topography-guided PRK and CXL can reduce irregular astigmatism, improve BCVA, and prevent corneal ectasia.
• The combined procedure has produced excellent outcomes in patients with keratoconus, pellucid marginal degeneration, and ectasia after laser vision correction.
Combining TG-PRK with CXL allows us to customize the treatment of patients with keratoconus, pellucid marginal degeneration, and ectasia after LASIK or PRK.4,5 The combined approach can decrease irregular astigmatism, improve BCVA, and reduce progressive ectasia. Using anterior surface curvature maps, we program the excimer laser to flatten steep areas and steepen flat areas to improve the regularity of the cornea’s anterior surface. Next, we perform CXL to stabilize the cornea and prevent progressive ectasia.
THE PROCEDURE IN DETAIL
Preoperatively, we obtain eight consecutive topographic maps, digitally enter the data into the computer of the excimer laser system, and review the information. Outliers are removed, and an average of the remaining curvature maps is obtained.
We perform a PTK using a 50-µm ablation with an 8.3-mm optical zone. Next, we proceed with TG-PRK, while limiting stromal tissue removal to 50 µm. Although we prefer optical zones of 6.5 and 6 mm, if the dioptric difference across the cornea is high, we may need to reduce the size to 5.5 or 5 mm to limit tissue removal. Applying sterile ice on a sponge to the cornea enhances patient comfort.
We administer a pledget soaked in mitomycin C for 1 minute. Next, we perform CXL using riboflavin drops and UV-A light with an energy level of 12 mW/cm2 for 10 minutes, applied in a pulse mode of 10 seconds on and 10 seconds off. The pulsed application of UV-A light increases oxygenation of the cornea during CXL,6 which, in our experience, improves the effect of CXL and reduces the chance of corneal haze.
LESSONS LEARNED
Performing TG-PRK and CXL for the management of ectatic diseases has taught us 10 major lessons.3,4

It is critical to make an accurate diagnosis of keratoconus. We never want to subject patients without the disease to TG-PRK or CXL. Pseudokeratoconus can be seen in the presence of a poorly captured topographic image, epithelial basement membrane dystrophy (Figure 1), superficial punctate keratitis, and any whorl-like keratopathy such as that which is secondary to drug deposition from amiodarone.
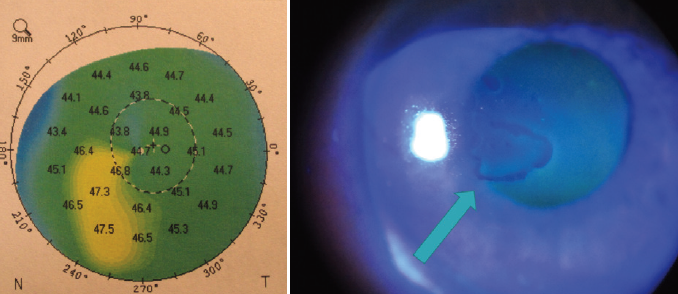
Figure 1. In this eye, epithelial basement membrane dystrophy created a topographic pattern of pseudokeratoconus.

Patient selection is important. The best candidate for TG-PRK has clear corneas, reduced BCVA, a minimum corneal thickness greater than 450 µm, topographic changes that extend into the pupillary zone, and less than a 10.00 D difference across the cornea.

We prefer bilateral treatments in patients less than 25 years of age who present with unilateral keratoconus. The incidence of bilateral keratoconus is 90%. The development of keratoconus in the so-called normal eye can be quick, with a loss of BCVA that is often difficult to reverse. Early treatment preserves the shape of the normal cornea.

Patients with stable keratoconus at any age may benefit from treatment to improve BCVA. The combined procedure may allow them to switch from rigid gas permeable (RGP) contact lenses to glasses or soft contact lenses.

Keratoconus patients with cataracts may benefit from TG-PRK prior to cataract surgery to decrease their irregular astigmatism. Treatment may obviate their need for RGP lenses postoperatively and enhance their BCVA (Figure 2). Cataract surgery can then be performed with the insertion of a toric IOL to address the more regular pattern of astigmatism.
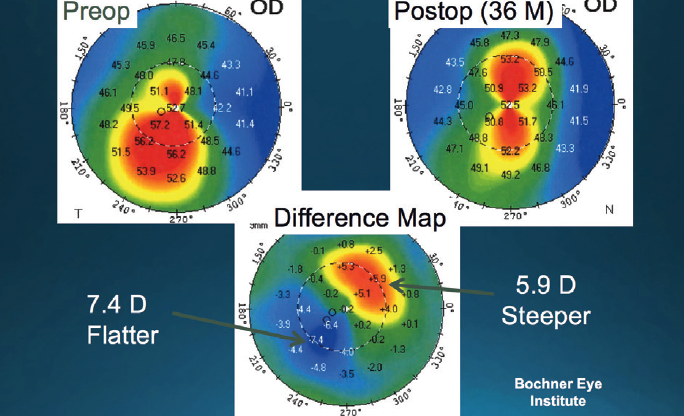
Figure 2. TG-PRK and CXL performed prior to cataract surgery steepened the superior cornea by 5.90 D and flattened the inferior cornea by 7.40 D. Cataract surgery was then performed and a toric IOL implanted.

We should not assume that the keratoconus of all patients who are over the age of 40 is stable. Annual follow-up topography is important to rule out progressive ectasia.

Tissue removal with TG-PRK, limited to 50 µm, does not appear to increase the risk of ectasia when combined with CXL, at least in the short term. At our center, we have performed TG-PRK combined with CXL for the past 5 years and have seen only one case of progressive ectasia, which was successfully treated by repeat CXL.

The complications of TG-PRK and CXL are generally minimal. The most common risk is corneal haze, which is generally mild, peaks at 2 to 4 months, and typically decreases over time. We have noticed a decrease in the incidence of haze when mitomycin C is applied after TG-PRK and CXL is performed in pulse mode.

Our optical zone preference for TG-PRK is 6.5 or 6 mm. We have found that smaller zones are associated with a lower chance of regularizing the cornea and improving BCVA.

TG-PRK and CXL can be successful in patients 9 to 15 years of age, with a low incidence of progressive ectasia. In 96 eyes of 52 patients, after an average follow-up of 28 months (range, 6–40 months), only one eye required repeat treatment.3,4
LISTEN UP
Gary Wörtz, MD, interviews William Trattler, MD, about his experiencewith CXL and the importance of early treatment.
Listen here.
CONCLUSION
In addition to young patients with progressive disease, TG-PRK plus CXL may be offered to older individuals who have stable corneas; in these cases, the goal is to reduce irregular astigmatism to allow wear of soft contact lenses or glasses.
1. Stein RM. Innovators lecture: topography-guided PRK and corneal crosslinking. Presented at: ASCRS/ASOA Congress & Symposium; May, 9, 2016; New Orleans, Louisiana.
2. Stein RM. Topography-guided PRK and CXL. Paper presented at: ASCRS/ASOA Congress & Symposium; May 6, 2016; New Orleans, Louisiana.
3. Stein RM. Topography-guided PRK. Cataract & Refractive Surgery Today. July 2014;14(7):79-81. http://bit.ly/2stein0317. Accessed February 9, 2017.
4. Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891-895.
5. Stein RM, Stein RL. Corneal collagan crosslinking: a major breakthrough in the management of keratoconus, pellucid marginal degeneration, and ectasia after LASIK. Ophthalmology Rounds, University of Toronto. 2011;9(1).
6. Mazzotta C, Traversi C, Paradiso AL, et al. Pulsed light accelerated crosslinking versus continuous light accelerated crosslinking: one-year results. J Ophthalmol. 2014;2014:604731.


