
In recent years, with the introduction of better devices for preoperative examination, advances in IOLs, and improved surgical technologies, there have been significant changes in our methods of treating astigmatism. Today, the treatment of astigmatism at the time of cataract surgery is our standard of care.
Approximately 30% of people older than age 40 years demonstrate astigmatism of greater than 1.00 D, which is, in general, our cutoff value for cylinder correction. For multifocal IOLs, our threshold is even lower, at 0.75 D.
Because of the accuracy required, we measure, reproduce, and compare the values generated with different diagnostic instruments on different days. We use the IOLMaster 700 (Carl Zeiss Meditec), the Cassini topographer (Cassini Technologies), the Keratron Scout Topographer (Optikon), and the Sirius (CSO), and we take into account total corneal astigmatism resulting from anterior and posterior analysis of the cornea.
Since we have implemented tear film analysis with LipiView II (Johnson & Johnson Vision) and treatment of dry eye disease in our practice, we also pay attention to this condition in our preoperative evaluation. If there is a problem with the tear film, we explain to patients how large an effect it can have on our measurements and results. We then treat the dry eye disease and repeat the measurements after improvement is noted. This routine has been well tolerated by our patients.
AXIS MARKING
We use the RoboMarker (Surgilūm) to mark the axis of astigmatism preoperatively. This method is economical and precise, and the device requires little maintenance. Our ongoing study using axis marking with the RoboMarker in combination with the Precizon Toric IOL (Ophtec) has shown good results regarding positioning of the IOL in the planned axis postoperatively (Figure).
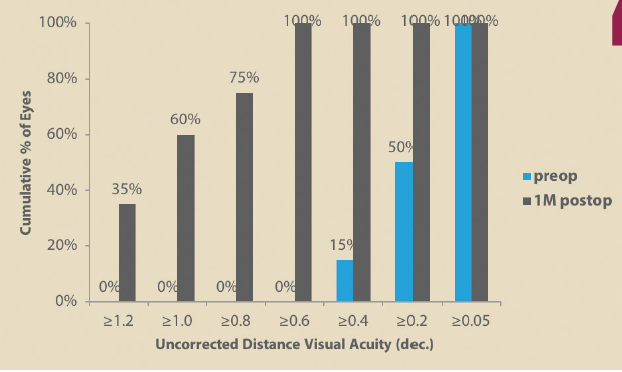
Figure. Uncorrected distance visual acuity in 34 eyes after implantation of a Precizon Toric IOL.
For laser cataract surgery, we use the IntelliAxis-L system (Lensar), which marks the axis of implantation directly within the capsulotomy after compensation for cyclotorsion. No preoperative marking is necessary with this system, enhancing our workflow.
Intraoperatively, other standard practices for us include the use of a capsular tension ring, creation of a capsulotomy with the perfect diameter to overlap the optic, and removal of the OVD from the capsular bag at the end of the case.
LENS CHOICES
Our standard toric monofocal IOL is the AT Torbi (Carl Zeiss Meditec), with its plate-haptic design and bitoric optic. Another toric monofocal IOL we have been using is the Precizon Toric, as mentioned earlier. This lens features an innovative toric optic design with a broader toric surface that makes the lens more tolerant to rotation and misalignment.
In the future, for laser cataract surgery, the Femtis Toric (Oculentis) will be my gold standard choice. This lens will provide the highest rotational stability, as demonstrated in a multicenter study presented in 2018.1
IRREGULAR AND REGULAR ASTIGMATISM
Irregular astigmatism is not always an exclusion criterion for a toric IOL. If, for example, in an eye with keratoconus the central cornea demonstrates a partially regular astigmatism, that patient may experience a great impact on his or her visual acuity with a toric IOL, often as an add-on lens. Or, in a younger patient with a similar presentation, a toric phakic IOL may even be of benefit. In corneas with highly irregular astigmatism and higher-order aberrations, the IC-8 IOL (AcuFocus), with its pinhole optic design, is a good option. We often use it in special cases such as eyes that have had radial keratotomy.
In laser cataract surgery for a patient with correctable regular astigmatism, if no toric IOL is used, relaxing incisions are always performed to maximize our standard of care. In more than 5 years, we have seen no complications with this approach, with significant reductions of astigmatism less than 2.00 D.
CONCLUSION
Today, with good preoperative diagnostic devices, easy pre- or intraoperative axis marking, and modern toric IOLs, astigmatism correction is a highly predictable procedure for reducing astigmatism in most patients.
Find out how I mark the axis of implantation during laser cataract surgery in the Table here.
1. Auffarth G, Breyer D, Dick B, et al. Fixation-stability and visual outcomes of the rhexis-fixated Femtis-IOL after automated femtosecond laser-assisted capsulotomy: interim results of the Femtis multicentre study. Paper presented at: ESCRS Annual Meeting; September 22-26.2018; Vienna, Austria.


