Severe Blunt Trauma
A positive outcome for a patient who had been told that nothing could be done.
Allon Barsam, MD, MA, FRCOphth

A few years ago, I treated a 41-year-old man who had suffered severe blunt trauma to one eye many years earlier. The patient experienced severe glare as a result of the trauma, such that he had to wear sunglasses whenever he was outdoors or even in a well-lit room. Also, his vision had decreased progressively since the incident because of the development of a traumatic cataract. Doctors advised the patient that nothing could remedy the glare and that treating the cataract would be too difficult and risky.
Upon seeing another ophthalmologist, however, the patient was referred to my practice.
CLINICAL FINDINGS
An examination found a moderately dense cataract, iridodialysis, and trauma to the sphincter of the iris (Figure 1). The crystalline lens was subluxated, and the equator of the lens was almost bisecting the visual axis.
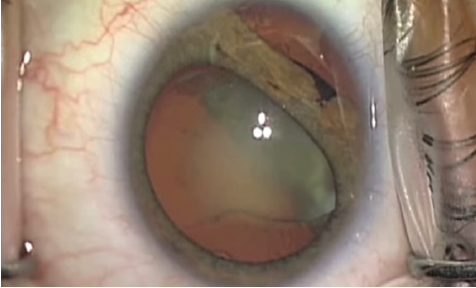
Figure 1. Traumatic cataract, iridodialysis, and trauma to the iris sphincter.
SURGICAL PROCEDURE
After the creation of the main incision, I injected an OVD to tamponade the anterior hyaloid membrane in the region of the zonular defect. A cohesive OVD was then injected, and three iris hooks were placed to keep the iris back and to prevent propagation of the iridodialysis during phacoemulsification.
I used a double-pass technique to create the capsulorhexis, centered on the capsular bag instead of the pupil to ensure optimum size and centration. I sought to preserve as much of the anterior capsular rim as possible to facilitate placement of a capsular tension segment (CTS). I injected an OVD to create a space between the dense cataract and the anterior lens capsule. A CTS was dialed underneath the anterior capsule. Next, a central iris hook was reversed 180º and used to pull the central eyelet of the CTS and ensure the stabilization of the IOL–capsular bag complex.
Phacoemulsification was carried out with low flow settings. I used a stop-and-chop technique to ensure that minimal force was placed on the already weak zonular structures (Figure 2). Using a Simcoe cannula, I performed manual irrigation and aspiration of the epinuclear shell and soft lens matter to ensure that the force exerted on the contents of the capsular bag was gentle. The tension on the CTS was reduced slightly to facilitate the removal of the soft lens matter under the device if required. The CTS was released, the bag was filled with a cohesive OVD, and a capsular tension ring was placed in the capsular bag.
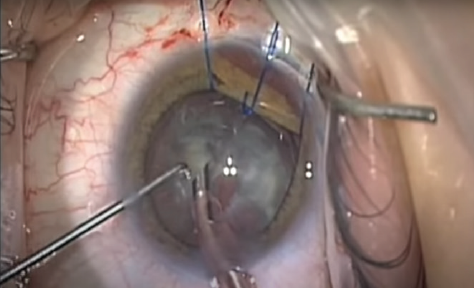
Figure 2. Phacoemulsification was performed with low flow settings using a stop-and-chop technique to limit the force exerted on the weakened zonular structures.
An 8-0 double-ended PTFE suture was placed through the eyelet into the capsular tension segment and docked into a 25-gauge needle. I used micrograspers to facilitate the docking. The suture was passed through the bed of the scleral flap. The needle was straightened, and a second pass was carried out adjacent to the central eyelet. The suture loops were then pulled into the eye, and the CTS was directed into the capsular bag. I applied tension to centralize the capsular bag. I then used a slipknot to allow tension to be titrated later on.
After implanting a one-piece aspheric IOL manufactured by Rayner in the capsular bag (Figure 3), I increased pressure on the CTS to ensure the centration of the IOL–capsular bag complex.
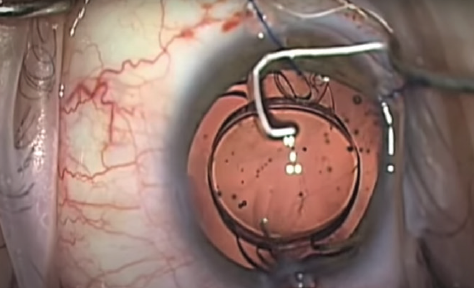
Figure 3. A one-piece aspheric IOL was placed.
I removed the iris hooks and aspirated the OVD, revealing the extent of the iridodialysis (Figure 4). I then injected acetylcholine (Miochol-E, Bausch + Lomb) into the anterior chamber, dispersed it, and placed a cohesive OVD.
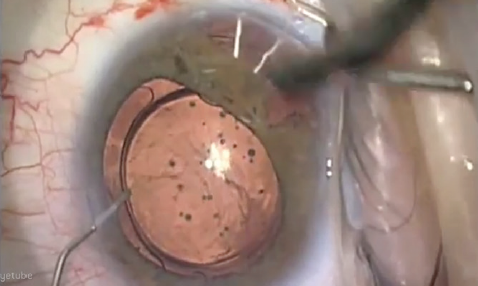
Figure 4. Iridodialysis visible after iris hooks have been removed and OVD aspirated.
Next, I passed a 10-0 double-ended polypropylene suture through the iris roots using the micrograspers for counter traction and a hand-over-hand technique between the micrograspers and the needle holders. I then pulled the suture inside the eye and directed tension to reapproximate the iris root with the scleral wall. The case concluded without incident.
OUTCOME
One month after surgery, the IOL was well centered, and the patient reported a resolution of glare symptoms (Figure 5). UCVA was 20/16. His only complaint was a feeling of imbalance because of the refractive error of -3.00 D in the contralateral eye.
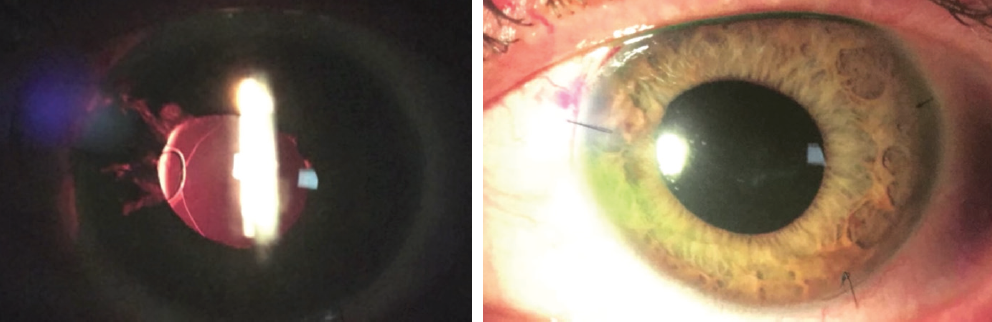
Figure 5. One month after surgery, the IOL is well centered (left and right).
Figures 1-5 courtesy of Allon Barsam, MD, MA, FCROphth
I performed LASIK on that eye to achieve emmetropia. After refractive surgery, UCVA was 20/10, and the patient was extremely satisfied.
The Psychological Toll of Ocular Trauma
A pellet gun injury changed the course of a young boy’s life.
Mark Kontos, MD

Managing patients with ocular trauma is a pretty common occurrence for most ophthalmologists. Most patients fade into the background of our memory. Some don’t though. Some we remember vividly. This case is one of those to remember.
The injury itself was not so unusual, a pellet gun shot to the eye of a 12-year-old boy. It was the aftermath and the consequences of the injury for him that have stayed with me over the years.
I was called to the emergency room on a summer afternoon to see an eye injury to a boy who had been accidentally shot with a pellet gun in the left eye at close range by his best friend (a member of a prominent family in our community). It was clear on examination that the injury was severe and that the eye would not likely recover useful vision. As I was talking to the mother, who was visibly distraught, I realized we were acquainted. She was a single mother who worked at our country club. After several heroic attempts to save the eye by me, our cornea surgeon, and our retina surgeon, the eye was eventually removed, and a prosthesis was placed with very good cosmetic results. Unfortunately, this did not result in a happy ending for the young man.
Initially, things seemed to go well, and he seemed to be adjusting to the new situation. One day, however, his mom took me aside and said he was struggling in school and had become socially withdrawn. Before the injury, he was a smart, outgoing kid who was very athletic and had been very popular in school. After the event, the injury resulted in a subsequent lawsuit that caused him to lose his best friend and many of their common friends. He was no longer able to play organized sports because of his eye injury and the associated loss of binocularity. His dreams of playing football in high school and being in the military had vanished.
I started to notice the changes over time as well and felt he was at risk for depression and its consequences. He did not have a father figure in his life, so I tried to do what I could to help without being too intrusive. I was able to get one of the professional golfers at the club to help, and we got the boy involved in golfing and the snowboarding camp at our ski mountain.
Over the next couple of years, he seemed to be managing as well as could be expected, and I was no longer in close contact with his family. His mother had left her job at the club, and I was seeing him only for yearly examinations. When he missed an appointment, I contacted his mother. Unfortunately, the news was not good. He had dropped out of school and had developed a significant drug addiction. After several unsuccessful rehabilitation attempts, he left home and moved to Portland, Oregon. She lost all contact with him and had become very depressed over the situation. I too, was saddened by the course his life was taking.
It was hard not to think that the trajectory of his life would have been much different had that pellet just grazed his face instead of doing the damage it did to his eye. He was a happy, well-adjusted young man with a life full of possibilities. That all changed the day he lost his eye. And I remember it like it was yesterday.
Traumatic Subluxated In–the-Bag IOL
Managing a complex case using the Jacob Paperclip Capsule Stabilizer.
Soosan Jacob, MS, FRCS, DNB

An interesting case that has stuck with me over the years is that of a middle-aged man who presented after sustaining ocular trauma from a shuttlecock while playing badminton. The patient had undergone cataract surgery a few years earlier. On examination, he had zonulodialysis and a subluxated in-the-bag IOL.
The traditional choice of treatment for this patient would have been to use sutured CTSs or a capsular tension ring to fixate the bag to the sclera. At the time, however, I was developing a new technique for sutureless transscleral fixation of the capsular bag—the glued capsular hook technique. The many disadvantages associated with suture fixation included increased surgical time, more complex and difficult surgery, difficulty with centration and adjustability, and the long-term possibility of suture-related complications. I therefore decided to use the glued capsular hook technique technique in this patient. Fortunately, the surgery was easy to perform, and the results were excellent.
The Technique
Sutureless fibrin glue–assisted transscleral fixation of the capsular bag entails passing a modified capsular hook into the plane between the anterior capsule and the posterior surface of the iris through a sclerotomy created under a lamellar scleral flap and using the hook to engage the rim of the capsulorhexis. The haptic of the capsular hook then passes out through the sclerotomy and onto the scleral surface, at which point the haptic is trimmed and tucked into a 26-gauge limbus-parallel intrascleral Scharioth tunnel. The scleral flap and the conjunctiva are closed with fibrin glue, providing transscleral centration and stabilization of the bag and obviating the need for other stabilization techniques postoperatively. Intraoperatively, if required, capsular bag support can be increased by the translimbal placement of capsular hooks that are removed after IOL implantation.
After first using this technique in this patient, I designed a modified version of the capsular hook: the Jacob Paperclip Capsule Stabilizer (Morcher; Figure 6).
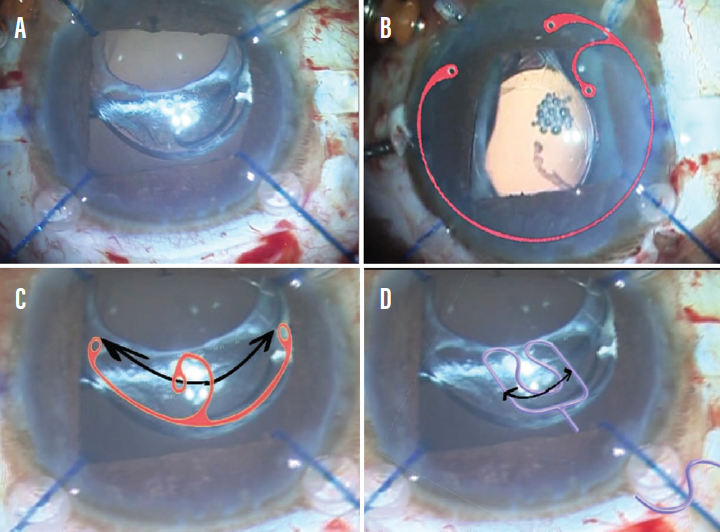
Figure 6. A subluxated capsular bag-IOL complex (A). A Cionni Ring for Scleral Fixation (B), an Ahmed Capsular Tension Segment (C), and a Jacob Paperclip Capsule Stabilizer (D), all from Morcher, are shown superimposed on the image. The amount of dissection of the bag required to implant the Paperclip Capsule Stabilizer is the least and can be accomplished more easily, even in fibrosed bags.
Courtesy of Soosan Jacob, MD, FRCS, DNB
Advantages of Technique
No extensive capsular bag dissection required. There is no need for extensive dissection of the capsular bag in order to insert the capsular hook, a step that is necessary with other fixation techniques such as the placement of an Ahmed Capsular Tension Segment or a Cionni Ring for Scleral Fixation (both from Morcher). Moreover, no complex suturing maneuvers are required, which simplifies the procedure.
Easy centration adjustment. Centration of the capsular bag and IOL is achieved by increasing or decreasing the degree to which the haptic is tucked into the intrascleral Scharioth tunnel. Just as with sutured scleral fixation, accurate placement of the flap is important; the flap should be centered on the zone of dialysis to avoid decentration of the capsular bag–IOL complex.
That said, I find that rectifying decentration secondary to a wrongly positioned flap is much easier with this technique than with sutured segments. A new lamellar scleral flap can be constructed in the desired area and the haptic interiorized into the eye by simply retracting it back with end-gripping microforceps. The haptic can then be exteriorized again through a newly constructed sclerotomy under the new lamellar scleral flap and tucked into a new Scharioth tunnel. Then, both flaps can be glued down using fibrin glue. The Jacob Paperclip Capsule Stabilizer offers good long-term stability and ease of surgery.
Traumatic Cataract
The tale of a traumatic cataract and three federal agencies.
By Michael E. Snyder, MD

An FBI agent—let’s call him Agent Iris—suffered a blunt injury to his left eye during a training exercise. The injury left him with significant photophobia and markedly reduced vision due to a mature, misshapen cataract and a 4.5–clock hour iridodialysis with a necrotic bridge of iris tissue (Figure 7). After a lengthy discussion of options, Agent Iris elected to undergo phacoemulsification of the cataract with vitrectomy and implantation of a Cionni Capsular Tension Ring and CustomFlex Artificial Iris (HumanOptics).

Figure 7. After a blunt injury to the left eye, a dense cataract, capsular plaque, iridodialysis, and zonules tethering the lens edge superonasally were observed. Pigment in the prolapsed vitreous is evident in the anterior chamber.
Red Tape
At the time, the CustomFlex Artificial Iris was not available in the United States. We therefore planned to obtain the device by making use of the US FDA’s Compassionate Use Device Exemption (CUDE) program, which we had previously used in a handful of cases. Unfortunately, the Department of Labor, which manages employment benefits for FBI employees, was very slow to approve payment for the device, so Agent Iris waited and waited.
After 6 months, the Department of Labor approved payment for the custom iris device, and a CUDE request was submitted to the US FDA. However, the US FDA’s investigational device exemption (IDE) study protocol for the CustomFlex was already under negotiation, and the agency was unwilling to issue a CUDE for the device in anticipation of the launch of the IDE study. Agent Iris had to go back to waiting.
The Surgery
Agent Iris became patient No. 1 in the US FDA IDE study 20 months after presentation. His surgery began with a one-port pars plana anterior vitrectomy to remove the prolapsed vitreous gel. A highly dispersive OVD was used to tamponade and protect the remaining exposed aphakic space during phacoemulsification. A type 1G Cionni Capsular Tension Ring was threaded into the capsular bag, and the capsule was recentered by tethering the ring to the scleral wall with a permanent suture.
An IOL was implanted into the capsular bag, and the CustomFlex Artificial Iris was trephined to the correct size and implanted into the capsular bag. Trypan blue dye was used to visualize the capsule while the device unfolded in the capsular bag because the red reflex is no longer visible when the opaque device begins to open. The necrotic iris tissue was removed using a vitrector, and the surgery was completed uneventfully. Agent Iris achieved a happy outcome with marked reduction in photophobia, no glare, and a UCVA of 20/16 at his final visit (Figure 8).
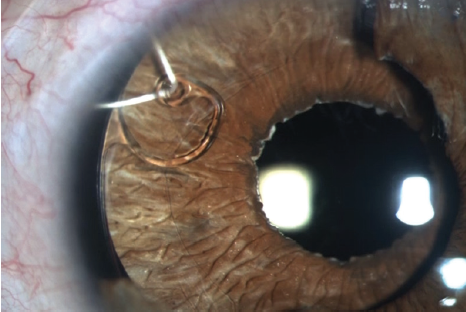
Figure 8. The Cionni ring and iris prosthesis are visible within the capsular bag postoperatively. The capsulorhexis is visible overlying the prosthesis, and the suture securing the Cionni ring is visible in its anterior chamber path and along the episcleral surface under the conjunctiva in the upper right corner of the image. The color match of the device compares favorably to the residual native iris tissue, which can be seen temporally.
Figures 7 and 8 courtesy of Michael E. Snyder, MD
Challenges Not Uncommon
This story, although unique in the layers of federal bureaucracy involved, is not unique with regard to the administrative challenges that patients with traumatic eye injuries face, especially when they have other comorbid ocular injuries, such as the iris damage in this patient. His case was finally resolved after 2 years, but I have had other patients who had to wait even longer. One patient who presented during my early experience with CUDEs had to wait 8 years to get approval, which came only after the device had been approved by the US FDA for more than a year.
Fortunately for similar patients today, the CustomFlex Artificial Iris is now US FDA approved and covered by Medicare and an increasing number of commercial insurers.
Roman Candle Injury
Treating a remarkable child’s thermal injury taught me several lessons early in my career.
By Elizabeth Yeu, MD

Managing ocular trauma can be physically and emotionally draining for all involved—the patient, the patient’s support system, and the clinicians. One case that taught me several lessons occurred early in my career. The patient was a 4-year-old boy who came in as an emergency with a Roman candle injury to the right eye that had occurred 1 or 2 days earlier. He was mature for his age and allowed me to perform a thorough slit-lamp examination.
Lesson No. 1:
Thermal injuries can devastate the eye very quickly. The initial examination surprised me, as there was already symblepharon beginning to form superiorly and inferiorly. The paracentral cornea had a small 0.5 mm by 1 mm perforation with iris plugging it, and the anterior chamber was formed. The corneal epithelium was denuded, with stromal thinning that was thinnest near the perforation. What a nightmare for this young child.
In the OR, I performed repair of the corneal perforation. I released the iris plug and placed cyanoacrylate glue to close the small hole. After releasing the conjunctival adhesions within the superior and inferior fornices, I performed amniotic membrane transplantation (AMT) with a large graft, reforming the fornices and covering the palpebral and bulbar conjunctiva with the AMT. A large-diameter soft contact lens was placed, followed by a temporary tarsorrhaphy. I prescribed topical moxifloxacin four times per day, prednisolone acetate 1% four times per day, and 500 mg vitamin C daily.
Lesson No. 2:
Young children have very robust healing potential. This patient required daily visits because his clinical examination changed quickly. Even the silk suture of the bolstered temporary tarsorrhaphy loosened much more quickly than in an adult patient. The AMT dissolved away within 3 days. The large-diameter soft contact lens was allowing almost full conjunctival epithelialization without further symblepharon formation. The corneal surface was healing with conjunctivalized epithelium, which was not unexpected but unfortunate, as I knew this meant limbal stem cell transplantation would be in his future. The main worrisome sign was slow reepithelialization of the central cornea. The corneal stroma was quite thin in the central 3 mm surrounding the area of the perforation. The anterior chamber was deep, which was a promising sign.
Lesson No. 3:
Collagenase activity is fierce. I saw how quickly a cornea can decompensate and melt away after a thermal injury, and, coupled with the metabolism of a young child, the process literally seemed to happen overnight. The central corneal perforation enlarged within a few days as it underwent deturgescence. The patient required a tectonic penetrating keratoplasty (PKP). I explained to his parents that for vision rehabilitation the patient would almost certainly require repeat corneal transplantation and a possible allograft AMT. Thus, back we went to the OR for a tectonic PKP, multilayered AMT to the surface, large-diameter bandage contact lens, and a temporary tarsorrhaphy.
This time, the cornea had a very difficult time reepithelializing postoperatively, and the patient’s peripheral cornea began to thin further. We decreased the topical medications, switched to preservative-free dexamethasone 0.1%, and maintained the oral vitamin C. The sutures loosened quickly. The clinical course necessitated multiple repeat returns to the OR for this child, who willingly obliged, for suture removal or replacement and repeat AMTs.
A BRAVE PATIENT
After all these heroic efforts, the patient presented four weeks after the PKP for a scheduled follow-up. He had no pain, but endophthalmitis had consumed the eye, which was completely filled with exudate anteriorly and gas-forming exudate within the entire vitreous cavity. This precocious boy knew what this meant for him. He turned to his mother, who was in tears, and told her that he was ready to have the eye removed because he didn’t want her to cry over him anymore.
After the eye was removed, he always returned for his appointments, fully understood the importance of monocular protection, and was compliant with wearing polycarbonate spectacles at all times.
Ocular trauma can take devastating turns, especially thermal or chemical injuries. The resultant damage may be progressive in nature, necessitating sequential procedures, and the prognosis is guarded for extensive injuries.