Refractive surgical options for hyperopia have tended to lag behind the advances made in the treatment of myopia. LASIK, PRK, and refractive lens exchange (RLE) have all been proposed to correct low, moderate, and high hyperopia. Phakic IOLs have also been to correct moderate or high hyperopia.
Hyperopes present a unique set of challenges for refractive surgeons. Compared to a normal emmetropic eye, a hyperopic eye typically has a short axial length; increased lens thickness; and, often, a small anterior segment and shallow anterior chamber depth, which is a contraindication for phakic lens implantation. Eyes with relatively flat corneal curvature and a thicker cornea are suited for a corneal laser refractive surgery procedure like hyperopic SMILE, as it is possible to significantly increase corneal curvature to correct hyperopia and continue to maintain postoperative visual quality.
Laser vision correction for hyperopic patients requires accurate preoperative assessment that must include cycloplegic refraction; this is a benchmark for setting surgical parameters. Precise centration during the surgery is also important for postoperative quality of vision. A larger treatment optical zone is required to minimize the potential induction of higher-order aberrations. Furthermore, a higher amount of tissue is removed during hyperopic compared to myopic ablations. Treating concomitant astigmatism, which is common in hyperopes, makes the surgery even more challenging. In most cases, surgical correction of refractive error also corrects accommodating esotropia, but sometimes a separate squint surgery is required.
An alternative approach to treating hyperopia using the lenticule extraction technique was first investigated in 2010. Although technically more difficult than myopic lenticule extraction, the investigators concluded that hyperopic lenticule extraction was feasible and merited further research. The results of the initial study, published 2 years later, were promising, but some eyes experienced similar problems to hyperopic LASIK, with a loss of corrected distance visual acuity and a significant degree of regression. It was surmised that the regression was most probably due to the treatment’s small transition zone size (<2.0 mm).
SOFTWARE IMPROVEMENTS
Since then, refinements have been made to hyperopic lenticule removal using the SMILE technique (Figure 1). An improved nomogram, alterations to the lenticule geometry, a larger transition zone of 2.0 mm, and optimized energy settings on the VisuMax femtosecond laser (Carl Zeiss Meditec), the proprietary laser used to perform SMILE, have successfully resolved many of the problems encountered in the first series of cases.
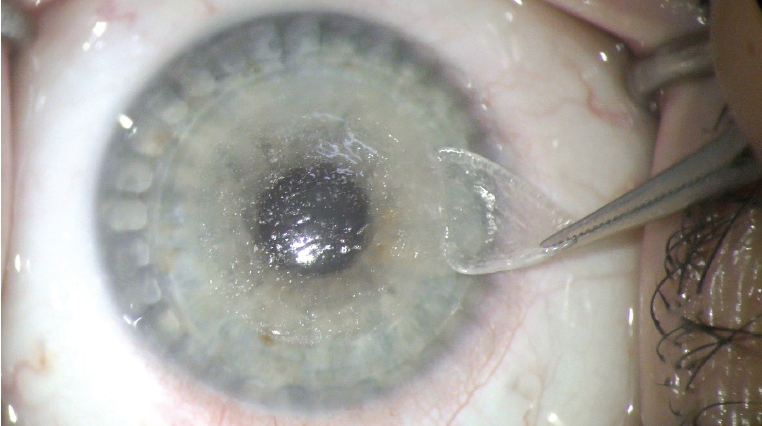
Figure 1. Lenticule removal during hyperopic SMILE.
To validate the safety and efficacy of these modifications, our clinic was selected to participate in a multicenter SMILE for hyperopia study, which involves six centers in Europe and three in Asia (two in China and one in India). The study will include up to 374 eyes, with hyperopia of 6.00 D or less and cylinder of 5.00 D or less. The highest intended correction is 7.00 D at the most hyperopic meridian, leading to a maximum postoperative keratometry (K) reading of 51.00 D. The primary endpoints of the study are safety and effectiveness as measured by corrected distance visual acuity (CDVA) and uncorrected distance visual acuity (UDVA). Secondary endpoints include contrast sensitivity, topography measurements, and subjective quality of vision questionnaires (see the sidebar At a Glance: SMILE for Hyperopia Study).
The study is ongoing. Initial results from our own cohort of patients (N=53) have been promising and augur well for the overall trial results, which will hopefully be announced in the near future. In our clinic, 102 eyes have already been successfully treated, including those with high astigmatism.1
The objective visual outcomes compare favorably with those obtained with hyperopic LASIK in the published literature. There was also a very high level of patient satisfaction, which indicates very good predictability. We believe that the wide optical zone after hyperopic SMILE provides a very good quality of vision, which is often difficult to achieve with LASIK. Regression and long-term stability must be confirmed with longer follow-up. We have also had very good results in eyes with high cylinders, leading us to believe that high astigmatism correction can be effectively combined with hyperopia correction. Interestingly, patients with higher corrections tended to be the happiest postoperatively because they derived the maximum benefit from the procedure.
The principle of hyperopic SMILE is not radically different from the principle used in myopic treatments, but it differs in terms of the geometry of the extracted lenticule. For hyperopic eyes, a negative doughnut-shaped lenticule with a diameter of 7.5 mm or more is created, which is thinner in the center and thicker in the periphery. After removal, the overlying anterior stroma remodels to create a steeper corneal profile and to correct the ametropia.
FIRST STEPS
We performed our first hyperopic SMILE procedure in October 2017 and were pleased that the surgery was relatively straightforward and the patient obtained a very good visual outcome. As we enrolled more patients and became more familiar with the procedure, the results continued to be impressive. We also became more accomplished at lenticule manipulation and extraction, and the procedure became routine.
From a surgical perspective, hyperopic SMILE is more challenging than its myopic counterpart. The reason is that the lenticule is about 8 mm, which is wider than the lenticule in myopic SMILE. It takes a bit longer to create the lenticule with the laser and to manually detach and remove it. With the longer laser surgery time, there is an increased risk that the patient will not fixate properly during the creation of the lenticule. However, this risk is largely theoretical, as it has not happened during surgery in our first 100 eyes.
The other challenge with the wider lenticule is that the incision is positioned closer to the limbus, where the blood vessels are located, which can increase the risk of bleeding and can interfere with the creation of the femtosecond laser cuts, including the entry to the incision for lenticule extraction, and, therefore, the smooth completion of surgery. Again, however, the risk is rather low, as we have not encountered this issue with our patients and have always managed to successfully conclude the surgery.
I also know that some other surgeons performing hyperopic SMILE avoid this problem either by performing a temporal incision, which is further away from the limbus, or by creating a second incision as a backup to enable them to proceed with the surgery in the event of difficulties in opening the first incision. I have never had to use this approach with a second incision, but it is good to know that this option is available if required.
In terms of complications, we did experience some mild haze in a few early patients, but we resolved this by reducing the energy settings slightly. We also had some transitory dry eye and some incidence of halos and glare at night, but these resolved spontaneously and were less significant compared to what we have experienced with hyperopic LASIK patients over the years. There were no issues with suction loss or torn or incomplete lenticule extraction.
SURGICAL PEARLS
For surgeons interested in adopting hyperopic SMILE when it becomes available, I would advise not to operate on low hyperopia early in the learning curve. The thinner lenticule in these patients is more difficult to manipulate.
For preoperative assessment, the maximum K reading after the surgery should be lower than 51.00 D, so it should be calculated preoperatively. Patients with steeper corneas or high hyperopia or a combination of these factors must be screened carefully and might not be eligible for hyperopic SMILE surgery. Dry eye can also be a contraindication, although this is not as critical as with hyperopic LASIK, in my opinion. Hyperopic SMILE should not be performed in unstable or irregular corneas because it would require a significant amount of corneal stroma, which can potentially induce ectasia. Finally, based on common surgical sense, patients with serious pathologies, recurrent or acute infections, ocular inflammation, or cataract or retinal disease will also not be good candidates for this treatment. Many of these exclusion criteria are not specific to SMILE but apply to all laser vision correction procedures.
Before the start of surgery, it is important to clean the cornea thoroughly and rinse out all debris. In terms of anesthesia, we instill a few oxybuprocaine drops into the eye a few seconds before inserting the speculum and commencing the docking procedure (Figure 2). Be careful not to instil too many drops over a long period of time before surgery, as the cornea might become slightly less transparent and interfere with the laser action.

Figure 2. Docking the interface on the patient’s eye.
As with myopic SMILE procedures, it helps to talk to the patient during the treatment phase, reassuring him or her and asking that he or she maintains proper fixation. I find this helps to keep the patient calm and concentrated and leads to safer surgery and better outcomes. If the patient is nervous and the eye is moving around a lot, it increases the risk of failure considerably. Our feedback from the patients has been positive, and they often remark how pain-free and comfortable they found the treatment. Sometimes they don’t even realize that we have completed the procedure—it really is that smooth and efficient.
AT A GLANCE: SMILE FOR HYPEROPIA STUDY
Participating Centers
- Six centers in Europe
- Two centers in China
- One center in India
Patient Population
- Up to 374 eyes with hyperopia of 6.00 D or less and cylinder of 5.00 D or less
- The highest intended correction is 7.00 D at the most hyperopic meridian, leading to a maximum postoperative keratometry reading of 51.00 D
- Primary endpoints: safety and effectiveness as measured by CDVA and UDVA
- Secondary endpoints: contrast sensitivity, topography measurements, and subjective quality of vision questionnaires
We target plano refraction in our hyperopic procedures and have found that the results have been excellent with this approach, although this must be verified with longer follow-up. With any hyperopic corneal procedure, there is marginally slower visual rehabilitation after the surgery, but I think this is probably something that is noticed more by the surgeon than by the patient.
Patients notice the “wow” factor at the first follow-up visit, especially higher hyperopes. We have found that patients are better informed and will often come to the clinic specifically asking for SMILE. This is usually because they have a friend or family member who had the treatment and were happy with the outcome. Word-of-mouth is a big factor in the growth of SMILE.
Early Study Results from another Hyperopic SMILE Study Site1
Purpose
- Evaluating the visual and refraction outcomes of SMILE for hyperopia
Study design
- Prospective study of vertex-centered hyperopic SMILE treatments in 93 eyes
- Inclusion criteria: maximum attempted hyperopic meridian between 1.00 and 7.00 D, CDVA of 20/40 or better
- Lenticule parameters: 6.3 to 6.7 mm diameter, 2-mm transition zone, 30 µm thickness, 120 µm cap thickness
- 3-month follow-up data included contrast sensitivity with the Functional Vision Analyzer
Results
- 82 eyes were available for follow-up
- Attempted spherical equivalent refraction: 5.62 ±1.20 D (range, 1.00–6.90 D)
- Attempted cylinder: -0.91 ±0.68 D (range, 0.00 to -3.50 D)
- Emmetropia target (n = 36): UDVA of 20/40 or better in 89%
- Spherical equivalent refraction relative to target: -0.17 ±0.85 D (range, -2.20 to 3.00 D)
- 59% and 76% of eyes were within ±0.50 and ±1.00 D of target refraction, respectively
- No clinically significant change in contrast sensitivity
Conclusion
- At 3 months postoperative, results with hyperopic SMILE in this population were promising
1. Reinstein DZ, Pradhan KR, Carp GI, Archer TJ, Day AC, Sekundo W, Dhungana P. Small incision lenticule extraction for hyperopia: 3-month refractive and visual outcomes. J Refract Surg. 2019;1;35:24-30.
CONCLUSION
The road to developing hyperopic SMILE has been long and occasionally difficult, but we have learned a lot along the way and have emerged with a treatment that I believe delivers high-quality visual outcomes with minimal complications.
Regulatory approval in the near future should give us a much-needed option for hyperopic patients who want to take advantage of the growing trend toward minimally invasive surgery. I think we will see a big demand for SMILE for hyperopia from our young hyperopic patients and a subsequent reduction in RLE rates. Based on my own results in more than 100 cases, I no longer perform hyperopic LASIK—the corneas are better postoperatively and the visual results superior, in my hands, with hyperopic SMILE.
Explore more and get in contact!
1. Stodulka P. Correction of hyperopia with hyperopic astigmatism by ReLEx SMILE: a case report. Paper presented at: the ESCRS Winter Meeting; February 15-17, 2019; Athens, Greece.


