
In routine cataract surgery, one of the biggest challenges is getting the IOL power right and the refractive predictability on target. Some of the variability in refractive outcomes arises from the effective lens position (ELP): Where exactly is the IOL going to settle within the capsular bag postoperatively? Although the role of the cornea is important, it is less important than axial length and ELP in getting the IOL power selection right in normal eyes.
ATA GLANCE
- Keratoconus adds complexity to cataract surgery, but there are methods and approaches that can help to improve refractive outcomes and patient satisfaction.
- An adjusted keratometric algorithm based on corneal steepness can greatly improve refractive predictability in IOL calculations for keratoconic eyes.
- The timing of cataract surgery depends on how well the patient was seeing prior to the cataract developing.
That all changes in eyes with keratoconus. Corneal distortions, including topographic and tomographic irregularity of the anterior and posterior corneal surfaces, the altered refractive index in keratoconus, and the irregular thinning of the cornea, all combine to make the cornea the key factor in IOL power determination in keratoconic eyes.
BIOMETRY
Most IOL formulas use a single number for the keratometry (K) value; this is simply not feasible in the keratoconic eye. Equally problematic is the use of one value for the corneal refractive index (1.3375). The cornea is too distorted to be represented by any one number, and it is unknown which part of the cornea the patient uses for his or her best acuity. Furthermore, that point may not be stable throughout the day, and it may not be the same for near, intermediate, and distance targets.
There is optical decentration in keratoconus, but if differs from the decentration that we deal with after decentered laser refractive surgical procedures. In keratoconus, the posterior cornea steepens along with the anterior cornea, decreasing the anterior-to-posterior curvature ratio. (This differs from the condition after ablative corneal surgery, in which the posterior corneal curvature typically remains unchanged.) What this leads to is an overestimation of the actual corneal net power. A second differentiating factor is the ELP, which is more posterior in keratoconic eyes than in normal ones due to the anterior displacement of the cornea. Both factors shift the refractive prediction error toward hyperopia. This is why, in mild to moderate keratoconus, a regular vergence formula can be used, targeting mild myopia. When multifocality within the optically active visual axis is pronounced, as in advanced keratoconus, ray-tracing software should be used to select the best IOL power. If possible, the ELP should be increased, as there is no algorithm specific for keratoconic eyes. A simple alternative is to target a slightly myopic refraction.
Camps et al recently showed that an adjusted keratometric algorithm based on corneal steepness can greatly improve refractive predictability in IOL calculations for keratoconic eyes.1 An overestimation of the corneal power leads to an underestimation of the IOL power, and the reverse is equally true.
In 18 eyes studied, the use of an adjusted keratometric approach based on an estimation of keratometric corneal power reduced residual refraction from greater than 5.00 to 0.60 D. The user simply looks up the appropriate refractive index for a specific K-value, and this value is then entered into the biometry calculations.
TIMING, LOCATION
Additional considerations besides biometry in keratoconic eyes include the timing of cataract surgery and the incision location. The timing of cataract surgery depends on how well the patient was seeing prior to the cataract developing. In most patients with keratoconus, by the time that cataracts develop, the keratoconus is no longer progressing and steepening, and the eyes have been stable for many years. Cataract surgery will restore vision to the level that the patient enjoyed prior to the cataract developing.
If vision was insufficient before the cataract developed, then it is prudent to first try to regularize the cornea by means of topography-guided PRK (if the pachymetry allows) or placement of intrastromal corneal ring segments such as Intacs (Addition Technology) or the MyoRing (Dioptex). Once the corneal shape has improved, cataract surgery can be performed and can be expected to yield a better visual quality outcome.
In corneas that are not too irregular, cataract surgery can provide good results. Toric IOLs can be used if the corneal astigmatism is regular (as is often the case with very inferiorly located cones or eyes with pellucid marginal degeneration), but they are not particularly useful in eyes with irregular astigmatism. Unless intraoperative aberrometry is available, my advice would be to steer clear of toric IOLs in irregular corneas (eg, where the cornea is bisected into a flat and a steep area, all within the pupillary zone).
Figure 1 illustrates a decision tree that can help to determine the best approach to cataract surgery in eyes with keratoconus.
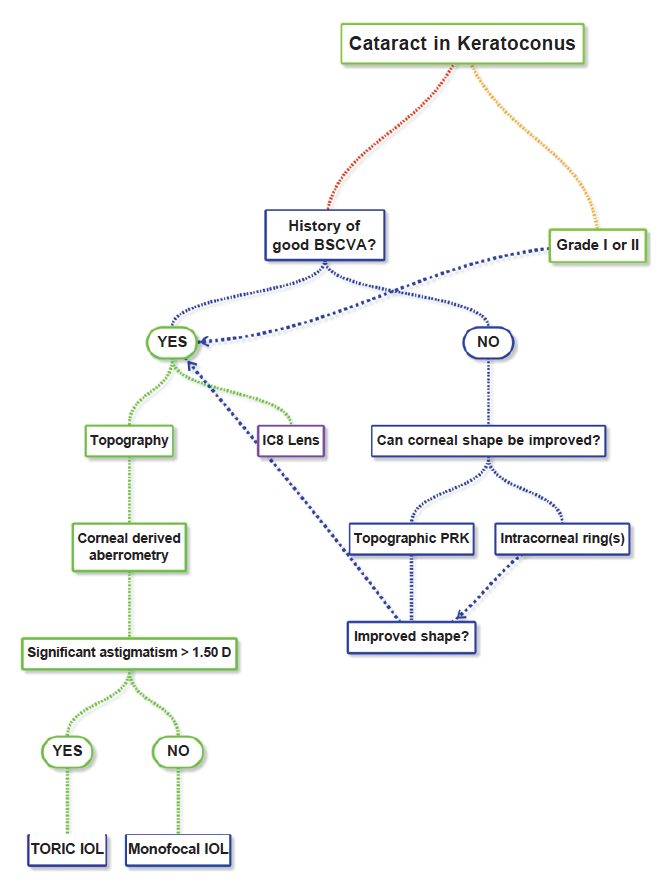
Figure 1. Decision tree for cataract surgery in keratoconic eyes. Adapted from Cummings A, Daya S. Cataract Surgery in Keratoconus. In Eds. Narang P, Trattler M. Optimizing Suboptimal Results Following Cataract Surgery; Refractive and Non-Refractive Management. In Press.
Incisions are best placed away from the thinnest area of the cornea. It is better to place them in the sclera rather than the cornea. Incisions that are placed in the cornea and near the thinnest point have the potential to further distort the corneal anatomy, leading to an even less predictable outcome.
SUMMARY
Keratoconus undoubtedly adds a layer or two of complexity to cataract surgery, but methods and approaches such as those described here can help to improve refractive outcomes and patient satisfaction.
1. Camps VJ, Piñero DP, Caravaca E, De Fez D. Preliminary validation of an optimized algorithm for intraocular lens power calculation in keratoconus. Indian J Ophthalmol. 2017;65(8):690-699.


