Cataract surgery is an ever-evolving procedure. We now have extensive options for pseudophakic vision correction, thanks to IOLs that can meet a variety of vision goals. Over the past several decades, the threshold for cataract surgery has been lowered as we have become able to offer more precise and safer surgery.
All of this progress has led to higher patient expectations. Cataract surgery has become refractive surgery, and surgeons are expected to offer options to tailor our patients’ outcomes to meet their lifestyle and occupational vision goals. With these expanded options, however, ophthalmologists are faced with new obstacles: We need to know how best to match patient expectations with the reality of our clinical options, and we need to discuss the out-of-pocket costs associated with nonstandard cataract surgery options, such as astigmatism and presbyopia correction with femtosecond lasers and/or IOLs.
Learning how to approach these topics with patients is now a crucial aspect of performing a refractive cataract surgery evaluation. Obtaining appropriate informed consent and ensuring that patients have a complete understanding of the realities of refractive cataract surgery are vital to achieving postoperative success.
AT THE CONSULTATION
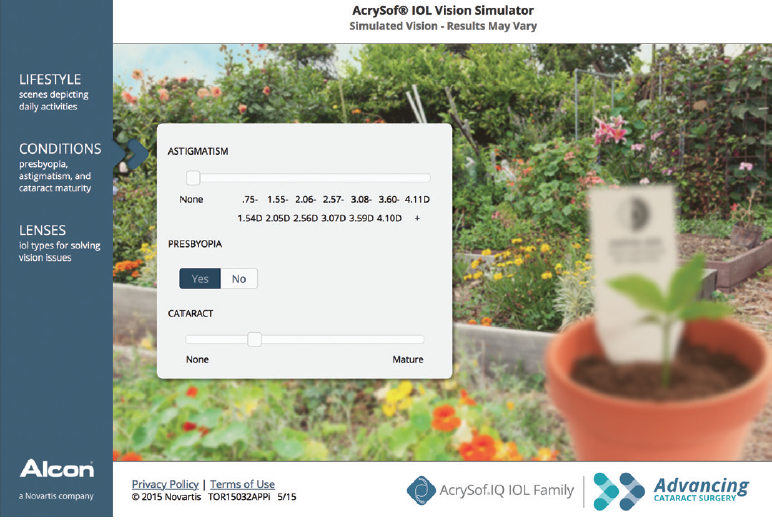
The preoperative consultation is our opportunity to discuss patient expectations and to set realistic goals. Questionnaires (Figure 1) are useful to gain a better understanding of the patient’s vision goals, and the information gathered can assist in tailoring your discussion of lens choices. Reviewing the questionnaire is an efficient way to see what the patient does and does not want. You can quickly rule in or out certain lens options based on the patient’s acceptance or reluctance to need spectacles for near, intermediate, and distance vision targets.
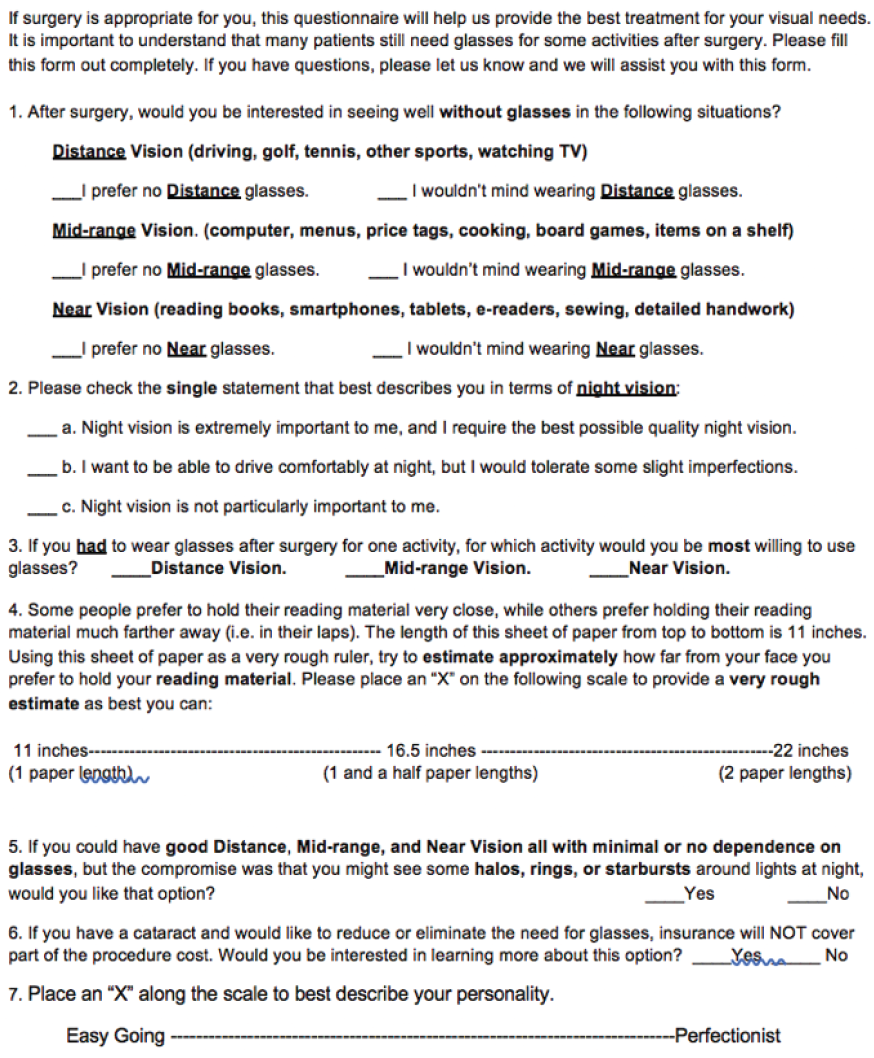
Figure 1. Example of a modified Dell questionnaire used in the authors’ practice.
A comprehensive slit-lamp examination is also necessary to identify ocular comorbidities that may lead to intra- or postoperative complications. Certain preexisting ocular conditions may exclude a patient from receiving certain IOLs, so it is important to conduct a thorough examination before recommending a specific premium lens option.
THE OCULAR SURFACE
Special attention should always be paid to the ocular surface, as significant ocular surface disease (OSD) can cause inaccuracies on corneal topography. When inaccuracies are present, they can ultimately lead to a refractive surprise. OSD can, and typically does, worsen in the postoperative period as well; therefore, addressing dry eye disease (DED) during the preoperative evaluation can be crucial to achieving patient satisfaction after surgery.
Despite a good refractive outcome, if patients experience fluctuating or decreased vision due to OSD postoperatively, they are more likely to report overall low satisfaction with their surgery. In our practice, we routinely begin aggressive treatment of the ocular surface for patients with clinical evidence of DED—both symptomatic and asymptomatic DED patients—before signing up them for cataract surgery. Preoperative biometry measurements for cataract surgery are repeated once the ocular surface has been optimized to ensure consistency and repeatability of IOL power calculations.
REFRACTION CONSIDERATIONS
Another important consideration is the patient’s preoperative refraction. Our current presbyopia-correcting lens options have a variety of near focal points, and, depending on the patient’s refraction, he or she may or may not be a good candidate for a presbyopia-correcting IOL. It is important to discuss the pros and cons of particular lenses, including expectation of focal points.
Also, beware of low myopes! Because these patients tend to have usable uncorrected distance vision and very functional near vision, they don’t realize their dependence on glasses. It is therefore important to clearly explain what they can expect from their new lens postoperatively; never assume they understand what it means when you discuss a distance goal.
In general, a frank discussion of the pros and cons of a particular IOL should be explored with the patient, including his or her desire for good uncorrected reading distance vision and the possibility that spectacles will be needed for certain situations.
INFORMED CONSENT
The informed consent process should be viewed as an opportunity to educate your patient about the procedure to be performed. It should explain the options for treatment, including no treatment or referral for treatment, as appropriate.
In our practice, we routinely tell patients that there is no perfect IOL and that we must choose from what is available to best meet their personal vision goals. This discussion should be tailored to each patient’s comprehension level. An interpreter should always be used if there is any language barrier. With in-office telephone services, getting a verified interpreter is now easier than ever. Even if a family member is in the room and offering to interpret, he or she may not know the scientific terms or be able to appropriately translate key aspects of the consent; therefore, authorized interpreters should always be used. The interpreter identification number should always be included on the consent and documented in the medical record.
The consent process is your chance as the surgeon to discuss IOL options that you think will best meet the visual goals of the patient and help him or her make an informed decision. Often, this involves explaining the concept of astigmatism and the options for its management. If patients decline correction of astigmatism and/or presbyopia, they must understand that they may require this additional correction in their glasses postoperatively. This conversation should also be documented in patients’ medical records.
The consent process is also your opportunity to discuss known risks of the surgery and to focus on possible complications that patients may experience, depending on their anatomy or certain predispositions. The specific postoperative complaints associated with particular IOLs should also be addressed during the consent process. For instance, if patients understand that they will have glare and halos in the postoperative period after placement of a multifocal IOL, they will be more tolerant of them early on.
For patients who are at elevated risk of postoperative refractive surprises, such as those with a history of refractive surgery, the potential need for ancillary procedures to correct any such surprises—mainly limbal relaxing incisions or laser vision correction—should also be mentioned during the consent process.
LEARNING ABOUT THE PATIENT
Your technicians and other staff members can provide valuable input during the preoperative evaluation. As the first people your patients encounter during their visits, all staff members should be well equipped to answer basic questions, including why testing and dilation are required for a preoperative evaluation. They may also pick up on a patient’s quirks or characteristics during the screening process that can be helpful to provide insight to the surgeon.
Actively including the patient and his or her family members in the decision-making process can help you choose the most appropriate lens to recommend for the patient. Knowing simple, practical things about your patient, like his or her preferred reading distance, can be helpful in selecting the add power for a multifocal IOL. This information can be obtained from the patient questionnaire or elicited during your conversation with the patient.
VISION SIMULATION TOOLS
• Carl Zeiss Meditec Vision Simulation Tool, available at zeiss.com/meditecpatient/int/cataract-treatment/service-and-tools/vision-simulationtool.html.
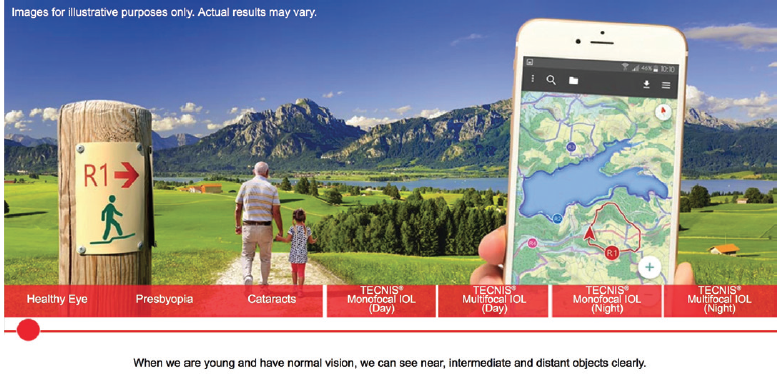
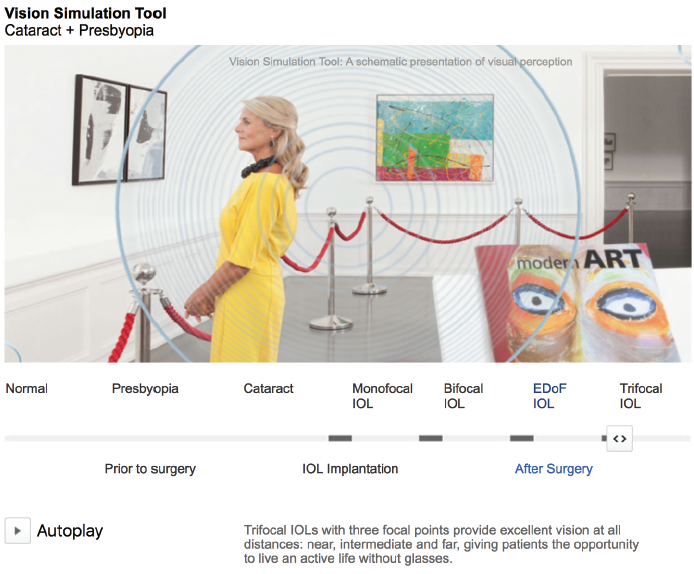
Educational videos and pamphlets can be useful tools to demonstrate the basic concepts of cataract surgery and to ease anxiety about the surgery. Vision simulators are an exciting new tool that can demonstrate potential vision with several commonly implanted premium IOLs (for some examples, see Vision Simulation Tools). These simulations can help translate our descriptions of vision into easy-to-understand visual simulations portraying various vision targets. In a busy clinic, putting instructional materials into patients’ hands can help streamline the consultation, answer some of their basic questions, and allow you to spend more time tailoring your lens selections to meet their specific needs (Figure 2).
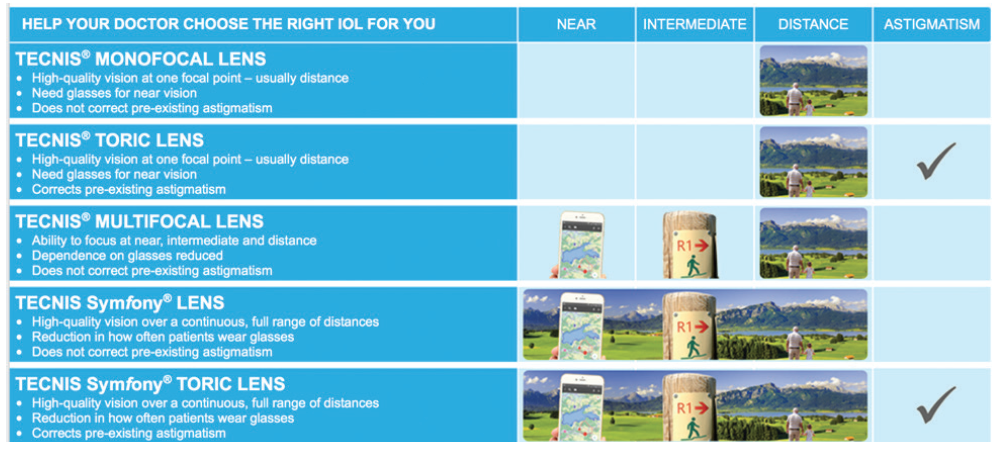
Figure 2. Instructional aids, like this one from the Tecnis Vision Simulator website, can help patients to understand the available IOL technologies.
PRECONCEIVED NOTIONS
Most patients have friends or family members who have gone through cataract surgery. They may come to your office with preconceived notions of what cataract surgery should be like. It is important to explain to patients that you are aiming to personalize their surgery and that their eyes may have some added complexity or comorbidity that may not lead to the same outcome that their friend or family member experienced. Alternatively, if they know of someone who had a complicated postoperative course, they may feel hesitant to pursue the surgery despite being an appropriate, low-risk candidate. Our job as surgeons is to personalize our conversations with patients to let them know where they lie on the spectrum of complexity and risk.
There are many valuable resources available to surgeons to foster appropriate informed consent. The Ophthalmic Mutual Insurance Company (OMIC) and the AAO have consent form libraries for commonly performed procedures that are readily available online. On the AAO site, these forms are available as PDF and Word documents in English and Spanish (aao.org/ethics-detail/informed-consent-form-library).
OMIC recommends that surgeons personally obtain patients’ informed consent to ensure that the procedure is being explained appropriately. Surgeons are also advised to document their efforts to educate patients about possible additional risks of surgery—for example, the possible need for an iris expansion device or the added complexity of surgery in a patient taking tamsulosin.
CONCLUSION
Spending extra time during the preoperative evaluation and consent process will save both you and your patients from postoperative surprises and you, ultimately, from potential liability. The consent must be thoroughly explained in the patient’s preferred language and at the patient’s educational level to ensure appropriate understanding. The consent process then must be further tailored based on the patient’s particular complexities and the IOL selection. Using patient questionnaires and online vision simulators can greatly assist in gaining the patient’s understanding.
Cataract surgeons have learned a lot from the refractive surgery community about how to appropriately achieve consent for premium IOL implantation to meet individual patient needs and expectations. By personalizing the consent process, we are doing our best to achieve postoperative success and earn high levels of patient satisfaction.