

Refractive and cataract surgeons are accustomed to presbyopic patients describing the deep impact their lack of accommodation has had on their lifestyles. Spending several hours a day educating patients on presbyopia and the options for its management has not desensitized us to the desire to do everything we can to help these patients.
And so, when a 50-year-old hyperopic woman entered our clinic desperate for a solution to her new problem, we listened attentively. Her refraction in each eye was around 2.00 D, and she shared the common story of once never needing glasses nor ever having the need for an eye doctor. Of course, in her 40s, she began realizing that her near vision was deteriorating, and it wasn’t many years after that her distance vision also crumbled.
The patient sold wine for a living, and she spent a significant portion of her day leaning over the small print on wine bottles as well as the fine print on contracts. Her workdays often ended late, requiring her to drive significant distances at night, which made her visual setbacks even more troublesome.
It was hard not to sympathize with her troubles as she made her case and asked for help. Through our conversation, it was apparent that she was highly motivated in her career and paid attention to detail. She came off as reasonable, honest, and as someone who would be content with any improvement in her situation at all, even if the result was not perfect.
THE IDEAL PATIENT?
It is estimated that more than 2 billion people will be affected by presbyopia by 2030.1 Many refractive and cataract surgeons refer to the treatment of presbyopia as the holy grail of eye surgery. Options for surgical correction of presbyopia at present include corneal inlays, monovision laser vision correction, and refractive lens exchange with either a monofocal IOL targeted for monovision or a multifocal IOL.
Our clinic has had relative success with the Kamra corneal inlay (CorneaGen). Once the inlay is implanted under a corneal flap in the nondominant eye, the small-aperture pinhole effect of the Kamra maintains its efficacy even as the patient continues to lose accommodation. Theoretically, the patient will not lose his or her distance or near vision as the eye ages. Most patients lose 1 line or less of distance visual acuity and gain about a 5-line improvement in near vision.2,3
Our group has published on how to select the ideal Kamra patient, and this particular patient seemed to meet most of our criteria. We look for hyperopic patients between 45 and 55 years old with a pristine ocular surface and reasonable expectations.4
At presentation, this 50-year-old woman had no significant medical history and was actively using cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan) for dry eye symptoms. Her distance UCVA (UDVA) was 20/200 OD and 20/400 OS, and her near UCVA (UNVA) was 20/400 OD and 20/400 OS. Her manifest refraction was +2.00 -0.25 x 021° = 20/20 OD and +2.00 -0.25 x 043° = 20/20 OS.
The patient’s central corneal thickness was 550 µm OD and 543 µm OS. Her keratometry readings were 39.76/40.21 @ 113 OD and 40.34/40.77 @ 100 OS. She was right-eye dominant. Her left eye tear breakup time (TBUT) measured on AcuTarget (Visiometrics) was normal, and her ocular scatter index (OSI) measured less than 1 (Figure 1).
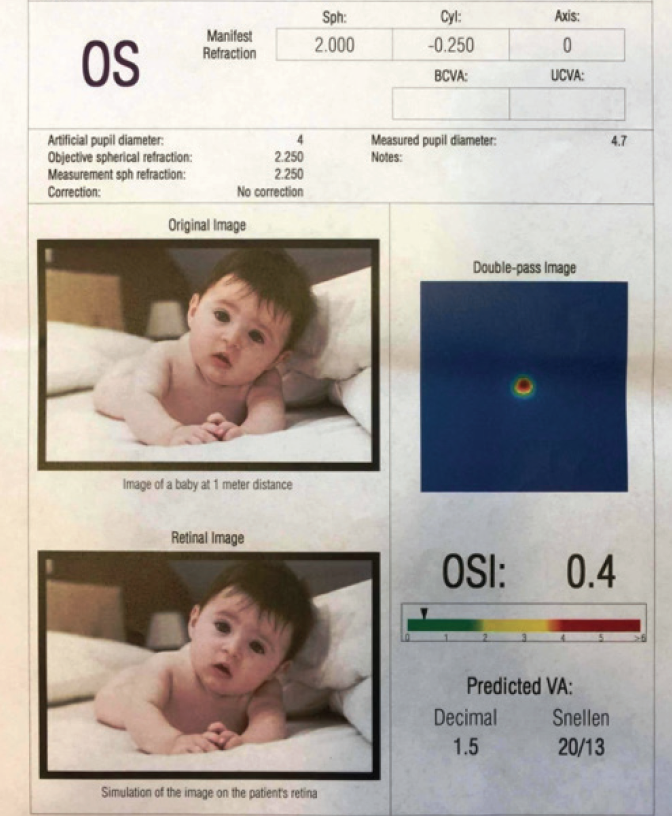
Figure 1. Preoperative OSI on AcuTarget HD shows minimal irregularity.
We had an extensive discussion with the patient regarding expectations, in which she acknowledged that her vision would not be perfect and that it would take several months to fully adapt, especially in the context of hyperopic LASIK. We agreed on a plan of LASIK for distance in her right eye and -1.00 D in her left eye, with placement of a Kamra corneal inlay also in her left eye.
THE RESULT
Surgery went smoothly, and the patient reported no issues that night. On postoperative day 1, her UDVA was 20/30 OD and 20/60 OS, and UNVA was 20/30 OS. Examination of her anatomy at that visit was unremarkable, and the Kamra was well centered. She demonstrated a fair level of anxiety on that day regarding her outcome but appeared reassured after extensive discussion about healing time.
Most of our challenges began at the postoperative month 1 visit. The patient’s UDVA was 20/25- OD and 20/80 OS and her UNVA was 20/20 OD and 20/20 OS. Her manifest refraction was -0.75 OD and -2.50 -1.50 x 180° OS. Upon entering the room she was tearful, with tissues in her hand. She said she was unable to drive and described her inability to get safely to work every day.
Her attitude during the visit alternated between anger and despair. Even her near vision wasn’t adequate, as she complained that it would transiently blur as she was attempting to read. She expressed regret for having had surgery several times and cited financial challenges that she felt were being exacerbated by her surgical outcomes. She adamantly denied ever being told that it would take several months for her vision to settle to our expected outcome, and she stated that multiple sources told her that her vision would be “perfect.”
One of us (SB) listened respectfully and acknowledged her frustrations. It truly was dispiriting to see how upset she had become over the past month and hear about the impact her vision was having on her work life.
When I saw an opening, I took the time to examine the patient thoroughly and to slowly review her measurements and imaging taken that day. As I had surmised from the refraction, her hyperopic ablation had overshot her into myopia in both eyes. Additionally, her AcuTarget HD images were notable for significant OSI levels and decreased TBUT (Figure 2). Her cornea in each eye showed significant superficial punctate keratitis. She reported that she was using artificial tears four times daily but had stopped using the cyclosporine due to cost.
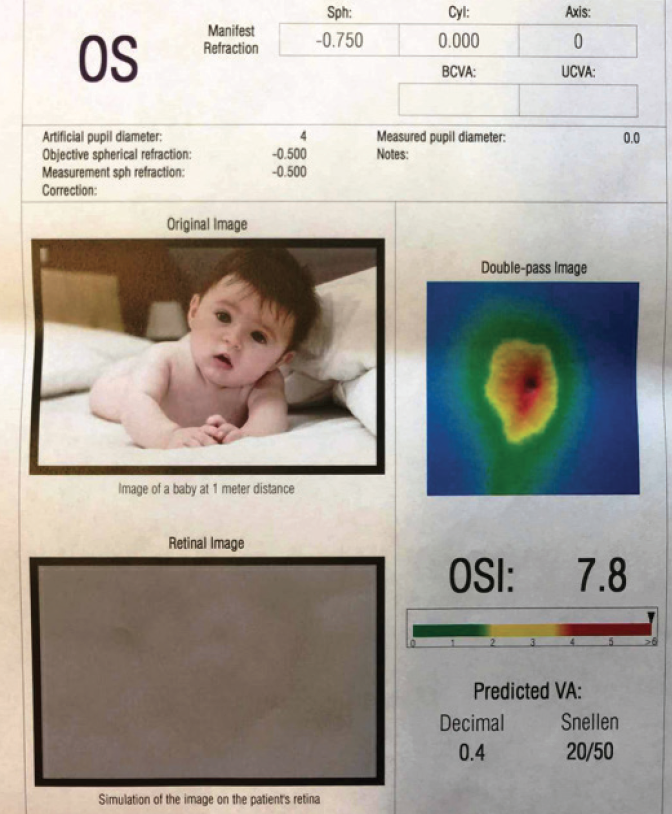
Figure 2. Month 1 postoperative OSI on AcuTarget HD shows significant irregularity.
I explained to the patient that she needed more time for the refraction to drift back toward hyperopia and, most important, that we needed to aggressively manage her ocular surface. We placed punctum plugs and provided samples of lifitigrast ophthalmic solution 5% (Xiidra, Novartis [formerly Takeda Pharmaceutical]) to be used twice daily. We recommended continued use of preservative-free artificial tears and encouraged the use of warm compresses at night. She left the visit upset and discouraged.
HAPPY, BUT …
Over the following 5 months, the patient called consistently to share her disappointment and to discuss removal of her Kamra. She often stated that we had misled her and that she wished she had never had surgery. I had the same conversation with her several times regarding refractive changes and ocular surface rehabilitation.
Although the patient required continued reassurance, her vision improved and she became more confident in us. At her 6-month follow-up visit, her UDVA was 20/20 OD and 20/30 OS, and her UNVA was 20/20 OS with a manifest refraction of -1.25 OS. AcuTarget HD measurement showed significant improvement in her OSI, to a level of 1.0.
The patient ultimately was happy with her results, but she continued to express disappointment with the overall process and our setting of expectations.
Our take-away from this patient and others like her is that, even though we do our best to properly set expectations, and even though many patients acknowledge what we’ve told them and believe that they are capable of being patient enough for the desired outcome, in reality this may not be so. We are all human, and, even when we think we understand a proposal properly and believe that we can handle the consequences, we do not know how we will react to the event until we are actually going through it.
When we encounter a patient like the one described here, therefore, we must be diligent in guiding him or her through troubling times. We must refrain from passing judgment on those who are not capable of handling the outcomes that we know they agreed to prior to surgery.
1. Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modeling. Ophthalmology. 2018;125:1492-1499.
2. Alarcon A, Anera RG, Villa C, Jimenez del Barco L, Gutierrez R. Visual quality after monovision correction by laser in situ keratomileusis in presbyopic patients. J Cataract Refract Surg. 2011;37:1629-1635.
3. Linn S, Hoopes PC. Stereopsis in patients implanted with a small aperture corneal inlay. Invest Ophthalmol Vis Sci. 2012;53:1392.
4. Logothetis H, Bafna S. Pearls for corneal inlay success. Ophthalmology Management. 2019;5:26-29.



