OICS and OR Waste Task Force
David F. Chang, MD
California, United States

The Ophthalmic Instrument Cleaning and Sterilization (OICS) Task Force was initially established with representatives from the ASCRS, AAO, and Outpatient Ophthalmic Surgery Society (OOSS) to evaluate and defend cataract surgeons’ use of shorter instrument sterilization cycles. The multisociety committee reviewed and conducted studies and surveys to develop evidence-based, ophthalmology-specific guidelines for the processing of anterior segment surgical instruments that were published in 2018.1 The document concluded by addressing the economic and environmental sustainability of cataract surgery given its high volume: “Many practices mandated by regulatory and licensing agencies might not have a proven benefit for ocular surgery and therefore might not justify the significantly higher cost and carbon footprint they entail. In addition, given the current and historically low rates of post-cataract endophthalmitis, costly new regulations should not be imposed without evidence of benefit.”
SURVEY RESULTS AND TRANSFORMATION
The OICS Task Force surveyed ASCRS, AAO, and OOSS members regarding OR waste and published the results in 2020.2 Of the more than 1,300 respondents, 93% stated a belief that OR waste is excessive and should be reduced, and 78% believed that more supplies should be reused. Most respondents (91%) expressed concern about climate change, and 87% agreed that their medical societies should advocate for reducing the OR carbon footprint; only 6% disagreed.
The most frequently cited causes of excessive waste were manufacturer and regulatory restrictions on the reuse or multiuse of devices, supplies, and pharmaceuticals. More than 90% of respondents believed the following:
- Profit, liability reduction, and a failure to consider the carbon footprint drive manufacturers to produce more single-use products; and
- There should be greater availability of reusable products and more regulatory and manufacturer discretion over when products may be reused.
Ten times as many survey respondents preferred reusable to disposable instruments if costs were comparable. In order of decreasing consensus, most respondents said they were already or would consider reusing topical and intracameral medications, phaco tips, irrigating solutions and tubing, blades, cannulas, devices, and surgical gowns.
Based on the strong consensus found in the aforementioned large survey, the OICS was renamed the OICS and OR Waste Task Force, and representatives from the American Glaucoma Society and Canadian Ophthalmology Society were added. OOSS President Cathleen M. McCabe, MD, and I cochair the task force. Our OR Waste Steering Committee includes John F. Doane, MD; Barbara Erny, MD; John A. Hovanesian, MD; David J. Palmer, MD; Alan L. Robin, MD; Audrey R. Talley Rostov, MD; Cassandra Thiel, PhD; Jeffrey Whitman, MD; and Ruth Williams, MD. Our goal is to advocate on behalf of our constituent society members for the reduction of needless surgical waste.
COLLABORATIONS CAN HELP REDUCE SURGICAL WASTE
As I wrote in a 2020 editorial for Ophthalmology, high surgical volumes in ophthalmology provide surgeons with both an opportunity and an imperative to collaborate with regulatory agencies and the surgical manufacturing industry to reduce surgical waste.3 The OICS questionnaire provided the surgical industry with an extensive market survey of surgeons’ preferences for multiuse and reusable products. The industry response has been positive, with virtually every company expressing a strong interest in and commitment to reducing our surgical carbon footprint. Each major manufacturer has designated liaison representatives to the OICS and OR Waste Task Force who have been active participants in our meetings. For example, multiple IOL manufacturers are working on replacing paper instructions for use with online instructions so that the box size can be reduced.
On the regulatory side, the OICS and OR Waste Task Force is working to overcome barriers to the multiuse of topical drugs in ambulatory surgery centers to sending newly opened bottles of topical drugs home with patients who need to continue them. Drs. Palmer and Robin are leading this initiative with their own volunteer subcommittee. The OICS and OR Waste Task Force is also conducting a survey of OOSS ambulatory surgery centers on their single use versus multiuse of topical medications and drafting a multisociety position statement on this issue. Unnecessary drug wastage is probably the single most costly problem in terms of the financial impact and carbon emissions in our ORs.4
1. Chang DF, Mamalis N. Guidelines for the cleaning and sterilization of intraocular surgical instruments. J Cataract Refract Surg. 2018;44;765-773.
2. Chang DF, Thiel CL; Ophthalmic Instrument Cleaning and Sterilization Task Force. Survey of cataract surgeons’ and nurses’ attitudes toward operating room waste. J Cataract Refract Surg. 2020;46:933-940.
3. Chang DF. Needless waste and the sustainability of cataract surgery. Ophthalmology. 2020;127:1600-1602.
4. Tauber J, Chinwuba I, Kleyn D, Rothschild M, Kahn J, Thiel CL. Quantification of the cost and potential environmental effects of unused pharmaceutical products in cataract surgery. JAMA Ophthalmol. 2019;137:1156-1163.
We Have No Time Left to Waste
J.J. Mura, MD, MHA, PDip (Film Studies)
Santiago, Chile

I was asked to give a lecture at the 37th Congress of the ESCRS about a new preloaded IOL delivery system. The system looked pretty good and offered several advantages, but it also had some flaws. First, if the IOL could not be inserted, it could not be reloaded, and a brand-new IOL package had to be used. Second, the system was disposable, so the inserter was discarded after every use. The evaluation of new technology, in my opinion, must consider the technology’s impact on the environment. Likewise, the adoption of new technologies, particularly in the case of disposables, must incorporate a recycling strategy. We must address this need together with industry. We simply have no time left to waste.
I am 52 years old. When I was a child, people were careful not to waste food. Currently, the United States wastes roughly 40% of its food, and much of the estimated 125 to 160 billion pounds of food that goes to waste every year is edible and nutritious.1 When I was a child, people fixed things—toasters, washing machines, almost anything. Currently, more than 300 million tons of plastic are produced every year, and single-use items compose about half of this amount.2
Waste doesn’t disappear, and a large proportion of it ends up in the ocean.3 At the beginning of the 20th century, human-produced anthropogenic mass (ie, the mass of all human-produced materials) equaled approximately 3% of the total biomass. On average, a quantity of anthropogenic mass greater than the body weight of each person on the planet is currently produced every week.4
Single-use disposable instruments for cataract surgery offer several advantages, but their impact on the environment must also be considered.
UNSUSTAINABLE PRACTICES
At the aforementioned ESCRS congress, I proposed reducing the carbon footprint of cataract surgery through readily available resource efficiency measures such as increasing the use of reusable instruments and supplies, performing immediate sequential bilateral cataract surgery, using flash autoclaving (ie, immediate-use sterile supplies), minimizing waste, instituting recycling practices, using energy-efficient appliances and air-handling systems, and investing in low-carbon energy sources.5 I cited an analysis of waste generation and life cycle environmental emissions from cataract surgery conducted at the Aravind Eye Care System in India.6 By combining several techniques, the facility’s carbon emissions per cataract procedure were 96% lower than in the United Kingdom. Considering that the reported rates of endophthalmitis are 0.01% and 0.04% to 0.08% at Aravind and internationally, respectively, Aravind’s greater reliance on reusable equipment did not appear to adversely affect the infection rate. The authors of the Aravind study concluded, “Surgical systems in most developed countries, and in particular their use of materials, are unsustainable.”7
The Aravind analysis suggests that ophthalmologists and other specialists can reduce material use (Figure 1) and emissions in medical procedures without compromising patient safety or surgical outcomes. The carbon footprint of the global health care sector equals 4.4% of all global net emissions (5% in the United Kingdom and 10% in the United States).8,9 Furthermore, a recycling strategy for new disposable technology should be devised by industry and medical professionals.

Figure 1. The waste generated from just one cataract surgery in the United States (left) compared to the waste generated from 93 cataract surgeries at the Aravind Eye Care System in India (right).
Courtesy of J.J. Mura, MD, MHA, PDip (Film Studies)
MEDICAL CONFERENCES
Most greenhouse gas emissions from medical conferences are generated by attendee travel.10 For example, 26,506 people attended the world’s largest radiology conference in 2017, which was associated with the emission of 39,506,038 kg of carbon dioxide. About 80% of that was attributable to international air travel.11
Restrictions on global travel related to COVID-19 drove medical conferences online.12 I believe a hybrid approach of in-person and virtual meetings should be used going forward.
PERSONAL CHANGES
Ophthalmologists can use several simple strategies to reduce their carbon footprint. One method is to switch from single- to double-sided printing, and another is to use electronic communication instead of printing when possible. Computer monitor brightness can be reduced to 80%. At the end of clinic, computers can be powered off, and room lights can be extinguished.12 (For more ideas, click the link in Read It Now: Related Content from the CRST Europe Archives.)
An average search engine query generates 0.2 g of carbon dioxide emissions. Providers can use the search engine Ecosia.org, which plants a tree for every 45 searches and donates 80% of its profits to nonprofit organizations.12
COLLABORATION
Cataract surgery is the most commonly performed surgical procedure worldwide. A huge amount of preoperative visits are conducted and laboratory tests are ordered by ophthalmologists before cataract surgery. Evidence suggests, however, that routine laboratory testing does not affect patient outcomes and that such testing could therefore be considered a misuse of resources.13 The aggregate cost of laboratory testing is substantial. As good stewards of the medical system, physicians must use these tests more judiciously.
The use of evidence-based preoperative evaluation guidelines that reduce unnecessary preoperative testing and clinic visits may help reduce total greenhouse gas emissions by up to 25% (from 79.56 to 59.32 kg) per patient.14 Ideal implementation might even have the potential to reduce carbon dioxide emissions by 50%. Utilization of telemedicine may be especially advantageous in the reduction of avoidable travel and should be incorporated into preoperative evaluations.
In 2013, the Royal College of Ophthalmologists published guidance on sustainability15 in their members’ practices. It was a visionary piece of work for that time, making suggestions ranging from community optometrist–led primary investigations for chronic eye conditions to the use of energy-saving light bulbs to reduce the carbon footprint. We need more initiatives like that.
CONCLUSION
Collaboration and a change in mindset are imperative to increasing the sustainability of medical practice. We have no time left to waste.
READ IT NOW
Related Content From the CRST Archives
Click here to read thoughts from Matthew P. Jensen; Randall J. Olson, MD; Jeff Pettey, MD; Thulasiraj D. Ravilla; Alan L. Robin, MD; Cassandra L. Thiel, PhD; Natarajan Vengadesan; and Rengaraj Venkatesh, MD, on adopting eco-friendly initiatives to reduce the carbon footprint of ophthalmology.
1. The problem of food waste. Foodprint. Accessed July 1, 2021. https://foodprint.org/issues/the-problem-of-food-waste/
2. Single-Use Plastics 101. Natural Resources Defense Council. Accessed September 3, 2021. https://www.nrdc.org/stories/single-use-plastics-101
3. Marine plastics. IUCN. Accessed July 1, 2021. https://www.iucn.org/resources/issues-briefs/marine-plastics
4. Elhacham E, Ben-Uri L, Grozovski J, Bar-On YM, Milo R. Global human-made mass exceeds all living biomass. Nature. 2020;588(7838):442-444.
5. Guttman Krader C. Surgery’s impact on environment. Eurotimes. May 1, 2020. Accessed July 1, 2021. https://www.eurotimes.org/cataract-surgery-impact-environment
6. Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43(11):1391-1398.
7. Haripriya A, Chang DF, Ravindran R. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: results from 2 million consecutive cataract surgeries. J Cataract Refract Surg. 2019;45(9):1226-1233.
8. Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care
system and effects on public health. PLoS One. 2016;11(6):e0157014.
9. Carbon footprint update for NHS in England 2015. Sustainable Development Unit. Accessed September 3, 2021. https://www.sduhealth.org.uk/documents/publications/2016/Carbon_Footprint_summary_NHS_update_2015_final_v2.pdf.
10. Roberts I, Godlee F. Reducing the carbon footprint of medical conferences. BMJ. 2007;334(7589):324-325.
11. Yakar D, Kwee TC. Carbon footprint of the RSNA annual meeting. Eur J Radiol. 2020;125:108869.
12. Merugumala SV. Keep calm and cut the carbon — sustainability in ophthalmology. Eyenews. December 7, 2020. Accessed July 1, 2021. https://www.eyenews.uk.com/education/specialty-trainee/post/keep-calm-and-cut-the-carbon-improving-sustainability-in-ophthalmology
13. Rusk MH. Avoiding unnecessary preoperative testing. Med Clin North Am. 2016;100(5):1003-1008.
14. Carbon footprint reduction by implementing standardized preoperative evaluation center guidelines. American Society of Anesthesiologists. Accessed September 3, 2021. http://www.asaabstracts.com/strands/asaabstracts/abstract.htm?year=2018&index=17&absnum=3770
15. The Royal College of Ophthalmologists ophthalmic services guidance. Sustainability in ophthalmology executive summary. Accessed September 3, 2021. https://www.rcophth.ac.uk/wp-content/uploads/2014/11/2013_PROF_222_Sustainability-in-Ophthalmology-May-2013.pdf
Going Green Made Easy
Todd L. Sack, MD, FACP
Florida, United States

Modern health care is not friendly to the environment. The US health care industry is responsible for an estimated 8% to 10% of the nation’s air pollution and about 10% of greenhouse gases. The health care industry is therefore a sizable contributor to the incidence of asthma, chronic lung disease, cardiovascular disease, cancer, and premature death.1 About 26% of air pollution and greenhouse gas associated with health care is the result of outpatient medicine (see Greenhouse Gases by US Health Care Service Type).1,2
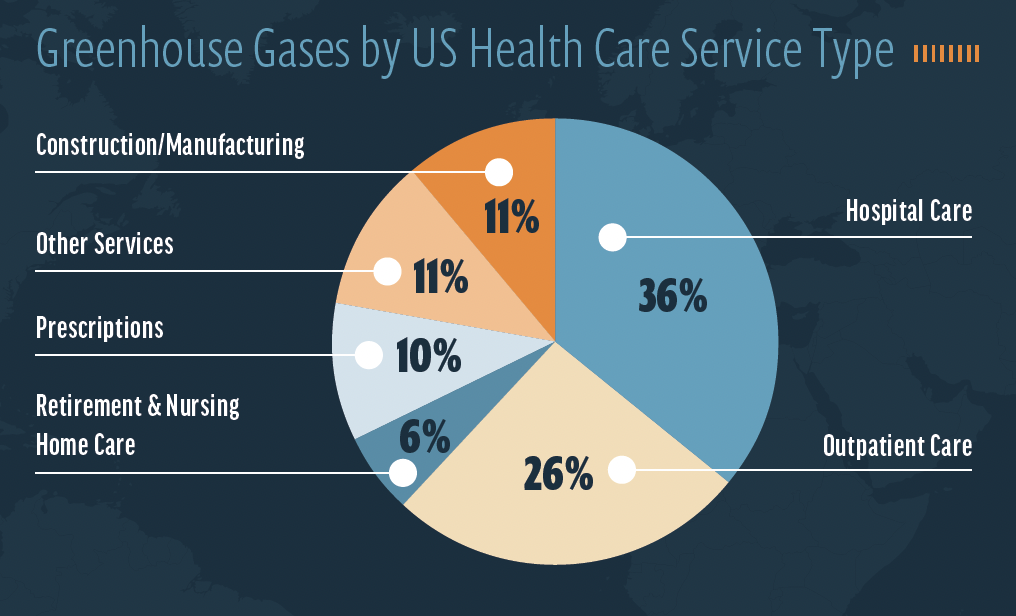
Source: Eckelman MJ, Sherman J. Environmental impacts of the US Health care system and effects on public health. PLoS One. 2016;11(6):e0157014.
Health care facilities also tend to waste energy, water, chemicals, and other materials, and they generally purchase and waste nonrenewable products. Materials are seldom recycled or composted.
WIELDING INFLUENCE TO EFFECT CHANGE
Few health professionals know if the products they use are produced from sustainable sources, are packaged responsibly, or were made in ways that treat workers fairly and safely. Health professionals, however, are powerful role models. Year after year, surveys report that these individuals are among the most trusted members of society. Nurses, medical doctors, and pharmacists often are listed as the top three most trusted US professional groups.3 As such, they have the potential to influence the sustainability choices of others.
Health care professionals can influence patients and colleagues by using energy wisely, recycling, choosing healthier cleaning products, and selecting energy-efficient vehicles. For example, during a Zoom conference in June 2021, Maya Ragavan, MD, MPH, MS, an assistant professor of pediatrics at the University of Pittsburgh in Pennsylvania, and Andrew A. Lewandowski, MD, a pediatrician with Group Health Cooperative of South Central Wisconsin in Madison, shared with me that patients and their families were pleased to hear their doctors and nurses discuss sustainability and climate change and they wanted to hear more.
MAKING AN OPHTHALMOLOGY PRACTICE ENVIRONMENTALLY SUSTAINABLE in four Easy steps
My Green Doctor is a free practice management service designed for all types of outpatient health care, including ophthalmic care. It was launched by the Florida Medical Association in 2010 to help members save money by adding environmental sustainability to their practices. Currently, My Green Doctor is offered by 15 health professional societies to their members as a free membership benefit (Figure 2). Health professionals who are not members of these societies can access most of the system’s offerings and teaching materials for free by registering at the organization’s website (www.mygreendoctor.org or www.mygreendoctor.es for Spanish). A 3-minute video on the homepage explains how to use My Green Doctor.
Figure 2. My Green Doctor is a free practice management service that helps members save money by adding environmental sustainability to their practices.
Courtesy of Todd L. Sack, MD, FACP
Step No. 1: Commitment. Leadership commits to making environmental sustainability a core value of the practice or facility.
Step No. 2: Scheduling. Team managers add 5 minutes of My Green Doctor business to the agenda of each regular staff meeting.
Step No. 3: Direction. Managers use My Green Doctor’s Meeting-by-Meeting Guide to lead each 5-minute session. Gradual improvements are made on topics such as energy and water use, recycling, chemical safety, patient education, climate change, and food choices. The guide provides a script to follow for each meeting. There is no need to be an expert or to hire a sustainability consultant.
Step No. 4: Goal. Plan to complete the steps required for the practice to qualify for My Green Doctor’s office certificate. This can be accomplished in as little as 3 months. Readers who learn about My Green Doctor from this article and register in 2021 will receive their certificate for free (the cost is $250 for practices that do not belong to a society that partners with My Green Doctor).
This management service has been used by thousands of health care professionals in 43 US states and 80 countries. The program is science-based, comprehensive, peer-written, nonpartisan, and easy to use. Most offices save money in the first weeks.
1. Eckelman MJ, Sherman J. Environmental impacts of the US Health care system and effects on public health. PLoS One. 2016;11(6):e0157014.
2. Sack TL. “Green” offices are healthier: new analysis. My Green Doctor. Accessed July 1, 2021. https://mygreendoctor.org/green-offices-are-healthier-new-analysis
3. McCarthy N. America’s most & least trusted professions [infographic]. Forbes. January 11, 2019. Accessed July 1, 2021. https://www.forbes.com/sites/niallmccarthy/2019/01/11/americas-most-least-trusted-professions-infographic/?sh=361013937e94
Minimizing Our Carbon Footprint: Initiatives and Practices Within Aravind Eye Care System
Rengaraj Venkatesh, MD, and Bharat Gurnani, MD
Pondicherry, India


Climate change is one key component of the World Health Organization’s sustainable development goals (Figure 3), and it is advancing faster than the expected rate.1 The atmospheric levels and emission of carbon dioxide are currently higher than they have been in thousands of years.2 Together, a continuous rise in temperature, extreme weather changes, and increased air pollution are intensifying the global burden of disease.3
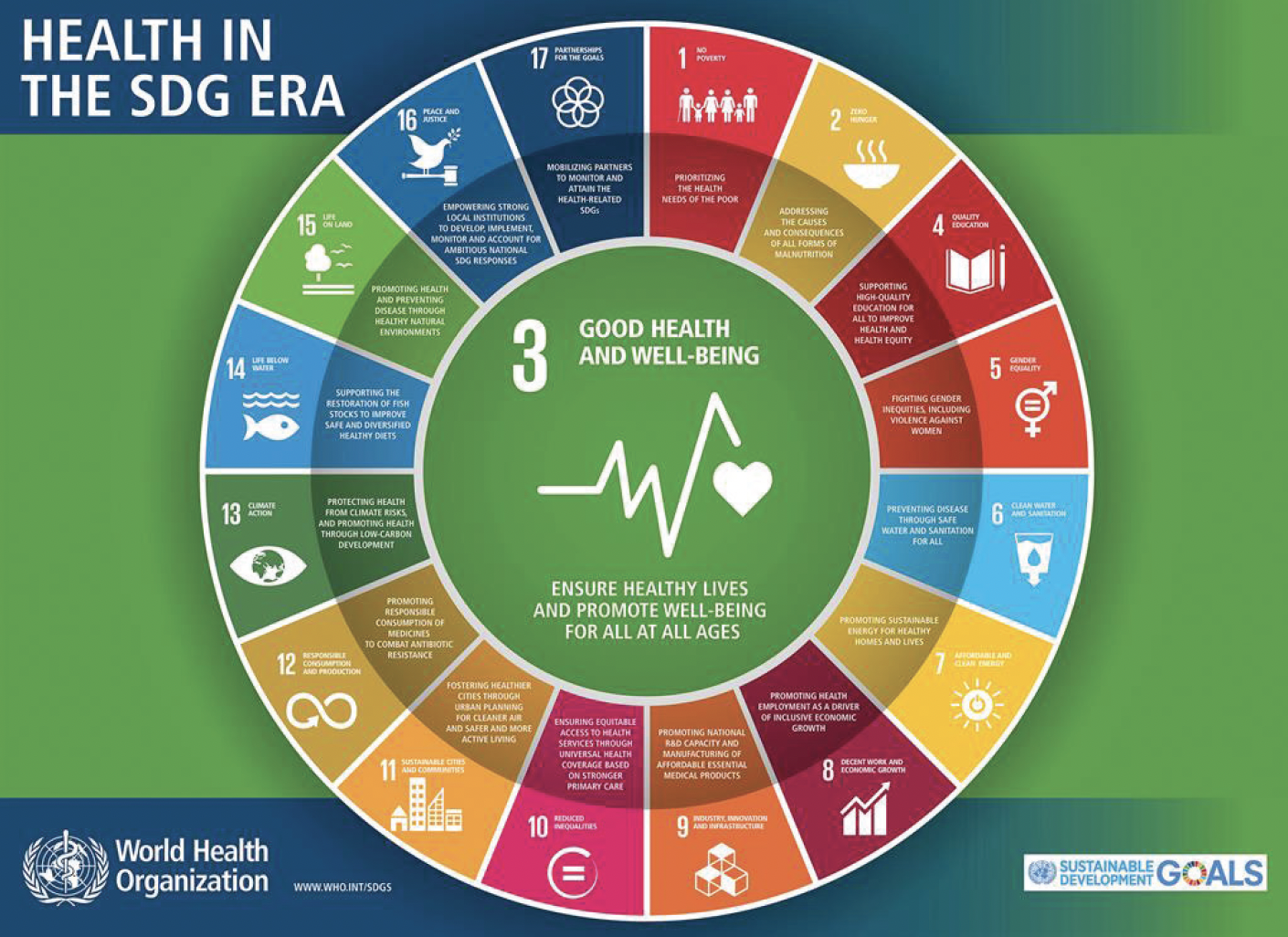
Figure 3. Explanation of the World Health Organization’s sustainable development goals (SDG).
Courtesy of the World Health Organization
Health care is a necessity, but it can leave a significant carbon footprint through activities such as the procurement of goods and services; energy use; the transport of staff, patients, and supplies; and the generation of complex waste.4 A recent analysis by NHS England showed that their total emissions were equivalent to 25 metric tons of carbon dioxide.5 This eye-opening statistic demonstrates why health care providers worldwide should develop and adopt environmentally sustainable practices.
Initiatives AT Aravind Eye Care System
Aravind Eye Care System (AECS) provides outpatient eye care to 4 million individuals and surgery to 5 million patients every year in an effort to reach our goal of eliminating needless blindness in our country. One of our primary focuses has been patient safety and health care regulations. More recently, however, we began pursuing environmentally sustainable initiatives to reduce our carbon footprint.
Green building and energy efficiency. AECS-Pondicherry is spread across 20 acres. The built-up area encompasses 2 million ft2, and it has a capacity of 700 beds. Green building and energy efficiency allow the maximum amount of natural light to enter the premises, and the building uses LED lights for lighting only when needed. Only a few key areas are air-conditioned; the corridors and open spaces have natural ventilation. A 138.68-kV alternative energy–generation unit (ie, solar-power) installed on the roof of the hospital (Figure 4) can generate more than 3 million units of electricity per year, which decreases the emission of carbon dioxide by 3 million kg per year.

Figure 4. Solar-generation panels were installed on the roof top of the AECS building.
Transportation. A comprehensive eye examination and select procedures are performed on the same day to reduce the number of patient visits required. Individuals who must travel long distances for care are admitted and undergo cataract surgery the next day. AECS has also established teleophthalmology-based primary eye care centers (our vision center model), and we offer roundtrip transportation to patients from outreach camps. These measures significantly reduce carbon dioxide emissions caused by patient travel. Additionally, nearly 90% of our 650 health care staff members live inside the premises and walk to the hospital daily for work.
Food management. AECS maintains its own low-maintenance, sustainable food forest that attempts to mimic the local woodland ecosystem. Our food forest includes rice paddies that generate 50 bags of rice and a vegetable garden that generates 200 kg of organic vegetables using wastewater each year (Figure 5). This food is served at the patient care cafeteria, and surplus vegetables are sold to staff. The food waste generated in the cafeteria and staff quarters is collected and used to generate biogas in our inhouse plant to cook in our cafeterias.

Figure 5. The food forest and lush garden at AECS are maintained using recycled water.
Surgical efficiency and reduced waste generation. Despite its high surgical volume, AECS generates only 0.25 kg of waste per phaco case (compared to an average of 2.25 kg per case in the United States reported in one study6) thanks to our resource utilization system. Nearly one-third of the waste at AECS is biomedical and goes to an incinerator located in Pondicherry. The remaining two-thirds is mostly plastic and paper. Plastic waste is taken by vendors to make plastic pellets, which are then used to create plastic utensils. Paper waste is either recycled or upcycled into paper artwork. The surgeons and staff wear reusuable gowns to cut down on OR waste (Figure 6).

Figure 6. Reusable gowns are used by surgeons and staff to reduce OR waste.
Figures 4–6 courtesy of Rengaraj Venkatesh, MD
Water. AECS installed waterless urinal systems to reduce water consumption, and several rainwater-harvesting soak pits were installed to recharge groundwater. AECS installed Southeast Asia’s largest wastewater treatment plant to recycle water. Its design is based on German decentralized wastewater treatment system technology, and it is able to process 100 m3 out of 120 m3 of water used at AECS daily. The recycled water is used to irrigate our fields and garden, and sludge deposits are used as fertilizer.
CONCLUSION
The initiatives described in our contribution to this article have helped AECS to reduce its carbon footprint and to become a role model for health care systems across the globe.7
1. The Sustainable Development Agenda. United Nations. Accessed September 14, 2021. www.un.org/sustainabledevelopment/development-agenda/
2. Lüthi D, Le Floch M, Bereiter B, et al. High-resolution carbon dioxide concentration record 650,000-800,000 years before present. Nature. 2008;453(7193):379–382.
3. Protecting health from climate change: World Health Day 2008. World Health Organization. 2008. Accessed September 14, 2021. https://www.who.int/world-health-day/toolkit/report_web.pdf
4. Brown LH, Buettner PG, Canyon DV. The energy burden and environmental impact of health services. Am J Public Health. 2012;102(12):e76-e82.
5. Tennison I, Roschnik S, Ashby B, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):e84-e92.
6. Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43(11):1391-1398.
7. Venkatesh R, van Landingham SW, Khodifad AM, et al. Carbon footprint and cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2016;27(1):82-88.


