CASE PRESENTATION
A 71-year-old woman reports experiencing fluctuating, poor-quality vision and constant glare, halos, and starbursts in her right eye since undergoing cataract surgery by another surgeon 5 weeks ago. Surgery included the creation of limbal relaxing incisions (LRIs) at the 3 and 9 clock positions and the placement of a multifocal IOL. The patient says that she has not experienced foreign body sensation or significant ocular dryness. She is following her postoperative drug regimen of twice-daily topical prednisolone, a daily topical NSAID, and a topical preserved fluoroquinolone administered four times a day.
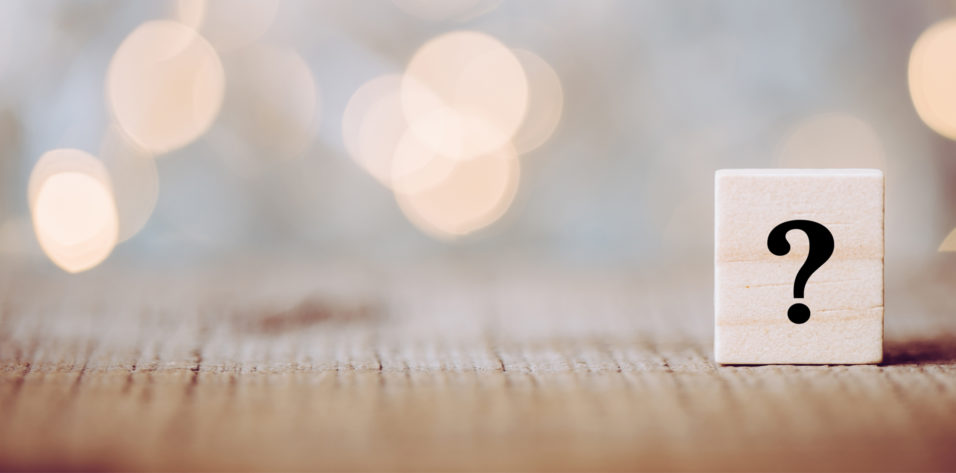
On examination, the UCVA in the patient’s right eye is 20/40 at distance and J3 at near, but it fluctuates wildly with rapid blinking. About 10 minutes after the instillation of artificial tears, her UCVA improves to 20/20 OD. Her manifest refraction in that eye is -0.25 D sphere. Keratometry readings for her eyes are as follows: K1 = 46.00 D @ 0º and K2 = 46.25 D @ 90º. The multifocal IOL is well centered on the undilated pupil
(Figure 1).
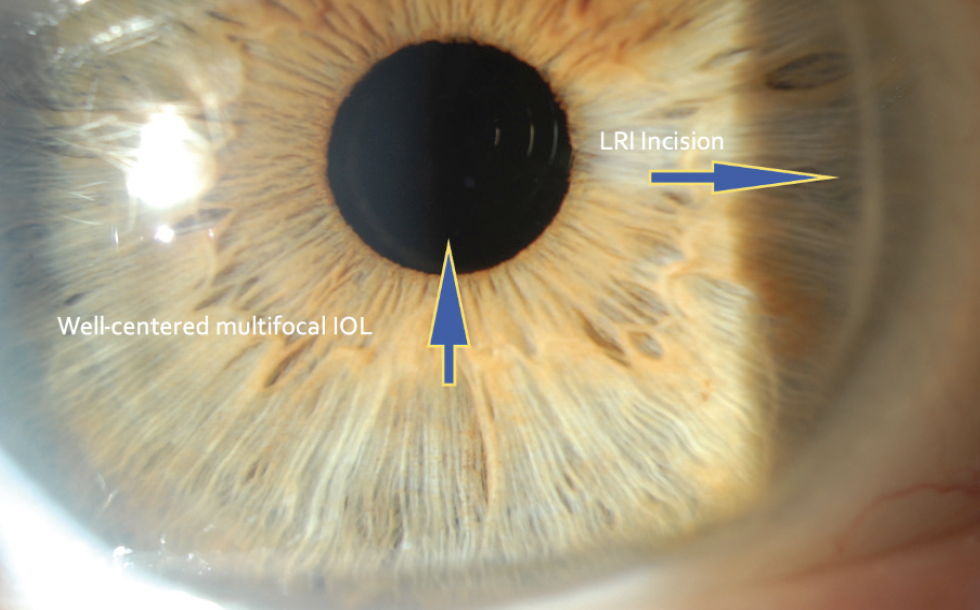
Figure 1. A multifocal IOL is well centered over the undilated pupil 5 weeks after cataract surgery.
The patient’s responses to a dry eye questionnaire indicate normalcy and no symptoms. Tear osmolarity measures 310 mOsm/L OD and 345 mOsm/L OS with the TearLab Osmolarity System (TearLab), and the result of a matrix metalloproteinase-9 test (InflammaDry, Quidel) is a dark red positive. Central and inferior corneal punctate epithelial erosions are observed. The tear meniscus is low, and tear breakup time is rapid. The patient exhibits moderate meibomian gland dysfunction (MGD) with poor expression and mild anterior blepharitis with soapy tears but no collarettes (Figure 2). The upper eyelid of the right eye is lax and floppy. Upon questioning, the patient says that she sleeps on her right side every night. Topography shows mild central irregular astigmatism that fluctuates in between blinks (Figure 3).
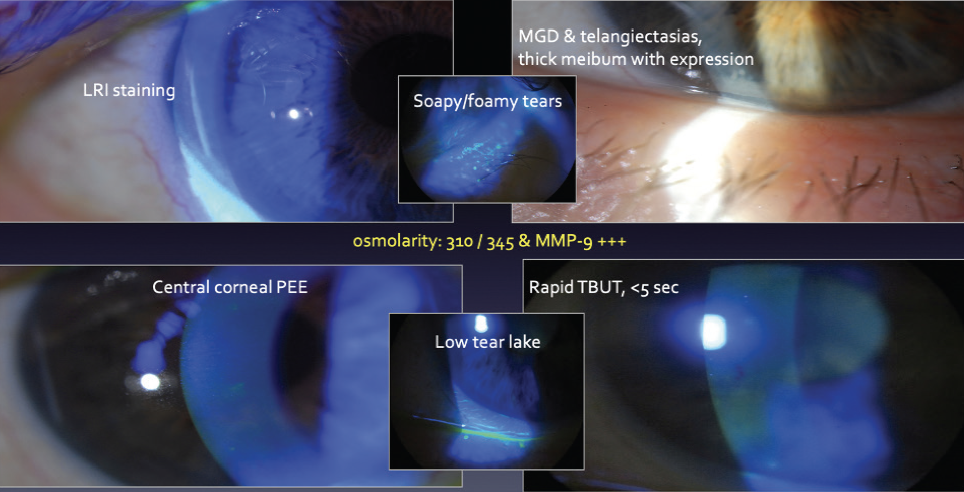
Figure 2. Tear osmolarity is 310 mOsm/L OD and 345 mOsm/L OS. Tear breakup time is rapid, and the level of matrix metalloproteinase-9 is elevated. An examination finds corneal punctate epithelial erosions, moderate MGD with poor gland expression, a low tear meniscus, and mild anterior blepharitis with soapy tears but no collarettes.
Figure 3. Mild central irregular astigmatism on topography.
The patient voices concern that her right eye is not healing correctly after cataract surgery and says she thinks a surgical complication occurred. The patient is seeking a second opinion. She is contemplating suing her original surgeon and has already contacted a lawyer.
What is the cause of this patient’s unsatisfactory result? Did a surgical complication occur? How would you help her?
—Case prepared by Christopher E. Starr, MD

MARJAN FARID, MD
This is a classic example of a patient with ocular surface disease (OSD) who was previously asymptomatic but whose OSD has become more apparent and visually significant after cataract surgery. Several studies have demonstrated that most cataract surgery patients have significant signs of dry eye disease (DED) yet are asymptomatic preoperatively.1,2 This case underscores the importance of identifying DED signs, educating patients about DED, and treating the disease before cataract surgery so that patients understand that their DED is preexisting and not a complication of the procedure. It is also important to counsel patients that cataract surgery will worsen their DED and explain why the tear film should be optimized before surgery.
This patient probably had undiagnosed MGD with high tear osmolarity and tear film inflammation before undergoing cataract surgery. Several factors likely worsened her signs and symptoms postoperatively. The creation of LRIs has been shown to worsen tear film production postoperatively because these incisions can disrupt the corneal basal nerve plexus, which then alters the feedback loop for tear production by the lacrimal functional unit.3 The LRIs at the 3 and 9 clock positions probably exacerbated her DED. That her symptoms and ocular surface staining are more significant in the right eye, correlating with the side that she sleeps on, suggests that exposure and mechanical complications from floppy eyelid syndrome are contributing to her OSD.
All patients—especially those paying out of pocket for technology to optimize their refractive outcomes—should be thoroughly examined for underlying tear film abnormalities before IOL selection. A pristine ocular surface and healthy tear film are required for optimal visual performance with a multifocal IOL. If these requirements cannot be achieved and if patients are not counseled on the importance of a healthy ocular surface before cataract surgery, they may blame the surgeon for their poor quality of vision postoperatively.

SUPHI TANERI, MD, FEBOS-CR
The case Dr. Starr shared is highly relevant and, unfortunately, indicative of a scenario that occurs more frequently than we surgeons would like. It demonstrates that, to achieve the intended outcome (ie, improved vision and a happy patient), it is not enough to perform flawless surgery, implant a premium IOL, and achieve a perfect refractive result.
The patient has tear film instability that worsened after cataract surgery. Aggravating the problem is that the LRIs severed the corneal nerves over approximately 2 clock hours each. These factors combined with a standard tunnel width of 2.5 mm and the creation of one or two paracenteses produced corneal nerve damage that explains why she has no foreign body sensation and a normal dry eye questionnaire despite several objective signs of OSD.
The instillation of artificial tears relieved her dysphotopsias and improved her vision. I would use this fact to explain to the patient that the cataract procedure was performed perfectly but that her tear film is no longer perfect. I would counsel her that the surgery and postoperative drug regimen had a negative but temporary impact on her tear film, the stability of which is crucial for good vision. I would also comfort the patient, who may fear persistent vision loss. Ideally, her preexisting MGD and anterior blepharitis would be treated with lid massage, oral minocycline, local antibiotics (azathioprine), and topical cyclosporine.
It is safe to assume that the patient seeks a rapid improvement in her symptoms. I would therefore counsel her to stop all preserved eye drops and prescribe viscous artificial tears that incorporate perfluorohexyloctane and omega-3 fatty acids (EvoTears Omega, Ursapharm) administered five times per day to increase tear breakup time. This regimen can be supplemented with the administration of hyaluronic acid and/or punctal occlusion as needed.
I would send the patient back to her operating surgeon but caution her not to undergo cataract surgery on the second eye until the vision in her right eye has stabilized. I expect the same issues to arise with her left eye.
If the tear film of her right eye is permanently compromised, a monofocal IOL might have been a more forgiving choice than a multifocal IOL. The LRIs contributed to corneal denervation and could have been avoided in favor of a toric IOL.

WHAT I DID: CHRISTOPHER E. STARR, MD
The insightful and thorough responses of the esteemed panel leave me with little to add. This case highlights the influence of the ocular surface on surgical outcomes, and it demonstrates that visually significant OSD can be perceived by patients as a surgical complication.
The cause of visually significant OSD is often multifactorial. For this patient, the causes of postoperative OSD included medicamentosa from medications and preservatives that are toxic to the cornea, disruption of the lacrimal functional unit by surgical incisions and LRIs that are long and deep, and exacerbation of untreated preoperative OSD (now recognized as flares). Compromised multifocal optics contributed to the unsatisfactory result.
An aggressive and multifaceted approach to treatment was therefore required. Treatment with toxic medications and preservatives was halted. Therapy with topical steroids and immunomodulators was initiated. Occlusion of the lower punctum, microblepharoexfoliation, and thermal pulsation procedures were performed. The health of the ocular surface recovered quickly, and visual quality, stability, and performance improved.
The patient was ultimately so pleased with the results of treatment and her surgical outcome that, after completing a similar but prophylactic regimen to treat OSD in the fellow eye, she returned to her original surgeon for cataract surgery on the second eye.
As the saying goes, an ounce of prevention is worth a pound of cure. The ASCRS published a preoperative algorithm for assessing and managing OSD in the preoperative setting that can be easily adopted in the office.4
1. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients' Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
2. Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44(9):1090-1096.
3. Ahmed MAA, Abdelhalim AS. Differential time-course tear film quantitative changes following limbal relaxing incisions. BMC Ophthalmol. 2020;20(1):175.
4. Starr CE, Gupta PK, Farid M, et al; ASCRS Cornea Clinical Committee. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45(5):669-684.