The transition from a normal physiologic state to a pathologic one in the ocular surface, like other tissues and organs, is influenced by etiologic factors, genetic predisposition, and host response (Figure 1). The extent to which these factors contribute determines whether a patient exhibits a subclinical or clinical phenotype of an ocular surface disorder (Figure 1). Beyond the elimination of etiologic factors, modulating the host response can be advantageous in resolving these conditions due to their critical role in regulating tissue homeostasis.
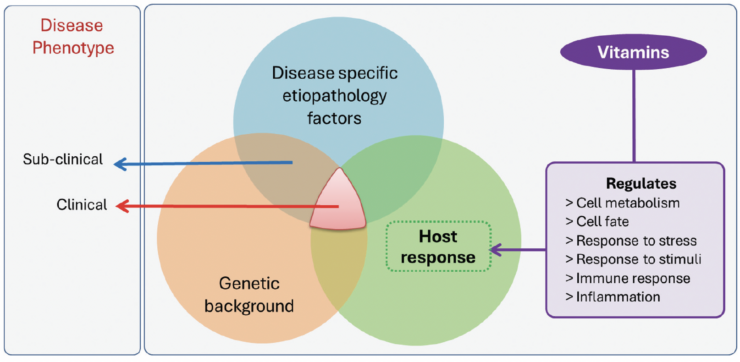
Figure 1. Interaction of genetic, etiologic, and host factors in ocular surface disease (OSD) phenotypes with the modulatory role of vitamins.
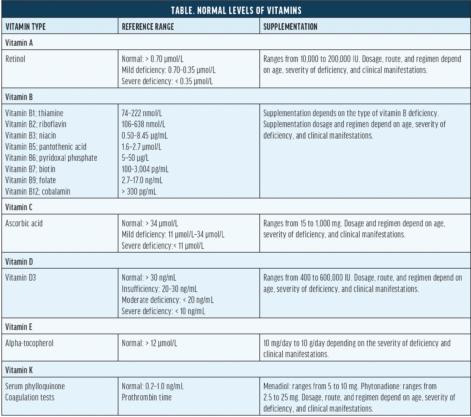
Nutrients, including vitamins, are crucial for optimizing host responses (Figure 1). Vitamins, a vital category of micronutrients, are classified as either fat-soluble or water-soluble. Vitamins A, D, E, and K are fat-soluble, whereas the B vitamins (B1 [thiamin], B2 [riboflavin], B3 [niacin], B5 [pantothenic acid], B6 [pyridoxine], B7 [biotin], B9 [folate], and B12 [cobalamin]) and vitamin C are water-soluble. The normal levels of these vitamins are outlined in the Table. Deficiencies can lead to a variety of systemic conditions with a profound impact on public health.
Vitamins also play a crucial role in maintaining ocular surface homeostasis by acting as cofactors or coenzymes in key biologic processes.1-3 The detection of and fluctuations in vitamin levels in tear fluid highlight the importance of vitamins in ocular surface health.4-7 Consequently, vitamin deficiencies and supplementation can lead to the development or resolution of ocular surface conditions, including dry eye disease (DED), conjunctivitis, and keratoconus; the ocular manifestations of autoimmune diseases; corneal haze; corneal dystrophies; the outcomes of corneal transplantation; wound healing after refractive surgery; and infectious and noninfectious inflammatory conditions of the ocular surface tissues and structures.1-3,8-13
Vitamin A
Vitamin A exists primarily in the forms of retinol, retinyl esters, and provitamin A carotenoids. It is crucial for growth, development, metabolism, cell proliferation, immune response regulation, and the differentiation of ocular surface epithelium. Vitamin A plays a key role in the visual cycle. It is an indispensable component of rhodopsin, a light-sensitive protein in the retina.14 Consequently, deficiency can lead to a variety of ocular conditions, including childhood blindness and night blindness (nyctalopia). On the ocular surface, vitamin A stimulates mucin production and enhances corneal wound healing.
Vitamin A deficiency can result in reduced goblet cell density, instability of the tear film, dryness of the ocular surface, epithelial metaplasia, keratinization, Bitot spots, punctate keratopathy of the cornea, corneal perforations, and keratomalacia.15 Dietary intake is the primary source of vitamin A, which is available in animal products, fruits, and vegetables. Both systemic and topical supplementation of vitamin A have been shown to improve ocular surface health by enhancing tear film quality through increased goblet cell density and mucin production, aiding corneal reepithelialization, reducing corneal epitheliopathy, preventing damage to the ocular surface, reversing conjunctival keratinization and squamous metaplasia, and alleviating DED.1-3 Oversupplementation of the vitamin, however, can have adverse effects such as blepharoconjunctivitis, conjunctival hyperemia, and meibomian gland dysfunction, all of which are reversible upon the cessation of supplementation.1,16
Vitamin B
The vitamin B complex is essential for ocular surface health. It plays a critical role in regulating antioxidative and immune responses, carbohydrate metabolism, protein synthesis, epithelial healing, neurotransmitter production, nerve regeneration, and remyelination. Research has indicated that epigenetic modifications might contribute to ocular surface conditions.17 Certain B vitamins are involved in the metabolism of homocysteine, which is crucial for epigenetic mechanisms such as DNA methylation.3,17
Deficiencies in vitamin B are often linked to OSD characterized by neurosensory abnormalities, including neuropathic pain. A double blind, randomized pilot study suggested that oral supplementation of vitamins B1 and B2, along with forskolin and rutin, can reduce DED signs and symptoms in glaucoma patients with OSD.18
The systemic supplementation of vitamin B12 has been found to enhance tear secretion and stability while reducing ocular discomfort in patients deficient in this vitamin who are experiencing neuropathic ocular pain.19,20 Topical administration of vitamin B12, either alone or in combination with citicoline or hyaluronic acid, can improve ocular surface health.21-23 Published reports have suggested that topical supplements containing vitamin B12 can decrease signs and symptoms related to DED, increase epithelial and subbasal plexus density, and reduce the number of corneal dendritic cells.21-23
Vitamin C
Vitamin C plays a crucial role in antiinflammatory, antioxidative, and immunomodulatory responses. It supports the synthesis of collagen and certain neurotransmitters, the metabolism of proteins, and the absorption of iron.24 Acting as a cofactor for proline and lysine hydroxylases, vitamin C is essential for the stabilization of types I and VI collagen. Vitamin C cannot be synthesized endogenously; fruits and vegetables serve as its natural sources. Its deficiency can lead to scurvy.
The measurement of vitamin C in the tear film and its role in stabilizing types I and VI collagen indicate the organic molecule’s significant impact on ocular surface homeostasis. In vivo research has demonstrated that vitamin C enhances corneal wound healing after injury by mitigating corneal edema, reducing infiltration by inflammatory cells, curbing corneal neovascularization, and fostering limbal stem cell proliferation.2 Systemic supplementation of vitamin C—in conjunction with vitamin E or with astaxanthin, vitamins A and E, and herbal extracts—has been shown to increase tear production and enhance tear film stability, particularly in diabetic patients and those with DED.25,26
Vitamin D
Vitamin D, a naturally synthesized steroid hormone, plays a key role in regulating calcium homeostasis, modulating inflammation, and influencing cell survival, proliferation, differentiation, and barrier functions. Vitamin D3 (cholecalciferol) is either synthesized endogenously in the skin from 7-dehydrocholesterol or obtained through dietary sources. It is then converted into its active form, calcitriol, in the kidney—a process that also occurs in the cornea.27 Notably, vitamin D levels have been found to be higher in tear fluid than in serum. Serum and tear fluid levels of vitamin D are positively correlated with tear film stability and tear production and inversely correlated with ocular surface discomfort and tear fluid inflammatory markers in patients who have DED.6
The beneficial effects of vitamin D are mediated predominantly through its interaction with the vitamin D receptor (VDR). Significantly reduced VDR levels have been observed in the ocular surface epithelium of patients with DED and keratoconus, a finding attributed to oxidative stress-induced VDR degradation.28,29 Restoring VDR levels in cells and tissues is therefore vital for enhancing the efficacy of vitamin D supplementation.
Systemic vitamin D supplementation has been shown to decrease ocular surface discomfort, enhance tear production and stability, and improve gut microbiome diversity.1-3,30 The development of practice guidelines for systemic vitamin D supplementation for the management of ocular surface conditions would be beneficial for practitioners.31
Topical supplementation of vitamin D, combined with vitamin A and omega-3, has been reported to enhance tear film stability, diminish ocular surface inflammation, and support reepithelialization.
Vitamin E
Vitamin E, encompassing tocopherols and tocotrienols, is recognized for its antioxidant properties. It influences cell signaling, gene expression, metabolic activities, and immune functions. Deficiencies in vitamin E have been linked to neuropathies, neuromuscular disorders, hemolytic anemia, and retinopathy. This organic molecule has been reported to lower the risk of developing cataracts, age-related macular degeneration, diabetic retinopathy, and retinopathy of prematurity. Although a direct causal link between vitamin E deficiency and OSD has yet to be established, systemic supplementation with vitamin E, combined either with vitamin C or with astaxanthin, vitamins A and C, and herbal extracts, has been shown to enhance tear production and tear film stability in patients with diabetes or DED.25,26 The topical application of vitamin E and coenzyme Q10 was found to improve tear film stability and corneal nerve innervation in patients.32
Vitamin K
Vitamin K, existing in forms such as phylloquinone (vitamin K1) and menaquinones (vitamin K2), plays a critical role in blood coagulation, bone metabolism, and cardiovascular health. Pathways dependent and independent of vitamin K–dependent proteins (VKDP) contribute to various biologic processes, including coagulation regulation, apoptosis, ferroptosis, angiogenesis, and receptor-mediated cellular signal transduction.8 Emerging research has highlighted the significance of VKDP in ocular conditions such as Schnyder corneal dystrophy, cataracts, and glaucoma.8,33 Further studies are needed to elucidate the roles of vitamin K and VKDP in OSD.
Strategic Nutrient Management for
Ocular Surface Health
Given that vitamins are integral to the biologic processes essential for ocular surface health (Figure 2), identifying and addressing vitamin deficiencies are crucial in the management of OSD. The choice of supplementation, dose, route, and regimen should be tailored to the severity of the deficiency and the patient’s clinical symptoms under the guidance of a physician (Table). For dietary intake guidance, specific recommendations34 can be consulted.
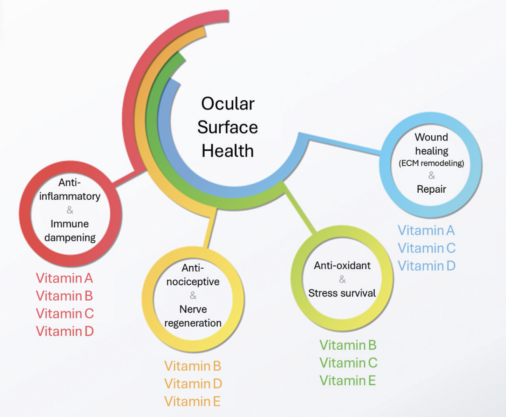
Figure 2. Schematic overview of vitamins’ roles in ocular surface health.
Although vitamin supplementation–related adverse reactions are rare, patient monitoring is essential, particularly for vitamin A. To date, supplementation with vitamins B, C, D, and E has not been linked to adverse reactions.1 Addressing vitamin deficiencies as a component of OSD management can enhance treatment efficacy, accelerate resolution, and prevent recurrence, which highlights the importance of this dietary approach in routine clinical practice.
1. Fogagnolo P, De Cilla’ S, Alkabes M, Sabella P, Rossetti L. A review of topical and systemic vitamin supplementation in ocular surface diseases. Nutrients. 2021;13(6):1998.
2. Han JY, Sang HB. Dry eye disease and vitamins: a narrative literature review. Applied Sciences. 2022;12(9):4567.
3. Markoulli M, Ahmad S, Arcot J, et al. TFOS Lifestyle: impact of nutrition on the ocular surface. Ocul Surf. 2023;29:226-271.
4. Ubels JL, MacRae SM. Vitamin A is present as retinol in the tears of humans and rabbits. Curr Eye Res. 1984;3(6):815-822.
5. Khaksari M, Mazzoleni LR, Ruan C, Kennedy RT, Minerick AR. Determination of water-soluble and fat-soluble vitamins in tears and blood serum of infants and parents by liquid chromatography/mass spectrometry. Exp Eye Res. 2017;155:54-63.
6. Khamar P, Nair AP, Shetty R, et al. Dysregulated tear fluid nociception-associated factors, corneal dendritic cell density, and vitamin D levels in evaporative dry eye. Invest Ophthalmol Vis Sci. 2019;60(7):2532-2542.
7. Sethu S, Shetty R, Deshpande K, et al. Correlation between tear fluid and serum vitamin D levels. Eye Vis (Lond). 2016;3(1):22.
8. Mong MA. Vitamin K and the visual system-a narrative review. Nutrients. 2023;15(8):1948.
9. Al-Sharif EM, Stone DU. Correlation between practice location as a surrogate for UV exposure and practice patterns to prevent corneal haze after photorefractive keratectomy (PRK). Saudi J Ophthalmol. 2016;30(4):213-216.
10. Dang ST, Lu XH, Zhou J, Bai L. Effects of 1alpha, 25-dihydroxyvitamin D3 on the acute immune rejection and corneal neovascularization in high-risk penetrating keratoplasty in rats. Article in Chinese. Di Yi Jun Yi Da Xue Xue Bao. 2004;24(8):892-903.
11. 11. Kundu G, Shetty R, Modak D, et al. Vitamin D and tear fluid cytokines in predicting outcomes in viral conjunctivitis: a new outlook. Indian J Ophthalmol. In press. 2024.
12. Gupta PC, Pathak M, Thakur B, Fogla R, Agarwal A, Ram J. Association of keratoconus with serum levels of 25-hydroxyvitamin D and antioxidant trace elements: a systematic review and meta-analysis. Indian J Ophthalmol. 2022;70(8):2818-2824.
13. Lasagni Vitar RM, Bonelli F, Rama P, Ferrari G. Nutritional and metabolic imbalance in keratoconus. Nutrients. 2022;14(4):913.
14. Saari JC. Vitamin A metabolism in rod and cone visual cycles. Annu Rev Nutr. 2012;32:125-145.
15. Gilbert C. The eye signs of vitamin A deficiency. Community Eye Health. 2013;26(84):66-67.
16. Samarawickrama C, Chew S, Watson S. Retinoic acid and the ocular surface. Surv Ophthalmol. 2015;60(3):183-195.
17. Busanello A, Santucci D, Bonini S, Micera A. Review: environmental impact on ocular surface disorders: possible epigenetic mechanism modulation and potential biomarkers. Ocul Surf. 2017;15(4):680-687.
18. Nebbioso M, Rusciano D, Pucci B, Zicari AM, Grenga R, Pescocolido N. Treatment of glaucomatous patients by means of food supplement to reduce the ocular discomfort: a double blind randomized trial. Eur Rev Med Pharmacol Sci. 2013;17(8):1117-1122.
19. Shetty R, Deshpande K, Ghosh A, Sethu S. Management of ocular neuropathic pain with vitamin B12 supplements: a case report. Cornea. 2015;34(10):1324-1325.
20. Ozen S, Ozer MA, Akdemir MO. Vitamin B12 deficiency evaluation and treatment in severe dry eye disease with neuropathic ocular pain. Graefes Arch Clin Exp Ophthalmol. 2017;255(6):1173-1177.
21. Yang J, Liu Y, Xu Y, et al. A new approach of ocular nebulization with vitamin B12 versus oxytocin for the treatment of dry eye disease: an in vivo confocal microscopy study. Drug Des Devel Ther. 2019;13:2381-2391.
22. Fogagnolo P, Melardi E, Tranchina L, Rossetti L. Topical citicoline and vitamin B12 versus placebo in the treatment of diabetes-related corneal nerve damage: a randomized double-blind controlled trial. BMC Ophthalmol. 2020;20(1):315.
23. Macri A, Scanarotti C, Bassi AM, et al. Evaluation of oxidative stress levels in the conjunctival epithelium of patients with or without dry eye, and dry eye patients treated with preservative-free hyaluronic acid 0.15 % and vitamin B12 eye drops. Graefes Arch Clin Exp Ophthalmol. 2015;253(3):425-430.
25. Peponis V, Papathanasiou M, Kapranou A, et al. Protective role of oral antioxidant supplementation in ocular surface of diabetic patients. Br J Ophthalmol. 2002;86(12):1369-1373.
26. Huang JY, Yeh PT, Hou YC. A randomized, double-blind, placebo-controlled study of oral antioxidant supplement therapy in patients with dry eye syndrome. Clin Ophthalmol. 2016;10:813-820.
27. Alsalem JA, Patel D, Susarla R, et al. Characterization of vitamin D production by human ocular barrier cells. Invest Ophthalmol Vis Sci. 2014;55(4):2140-2147.
28. Panigrahi T, D’Souza S, Shetty R, et al. Genistein-calcitriol mitigates hyperosmotic stress-induced TonEBP, CFTR dysfunction, VDR degradation and inflammation in dry eye disease. Clin Transl Sci. 2021;14(1):288-298.
29. Shivakumar S, Shetty R, Ghosh A, Jeyabalan N. Abstract presented at the Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting; April 27-May 2, 2019; Vancouver, Canada. Invest Ophthalmol Vis Sci. 2019;60(9):2819.
30. Singh P, Rawat A, Alwakeel, M, Sharif E, Al Khodor S. The potential role of vitamin D supplementation as a gut microbiota modifier in healthy individuals. Sci Rep. 2020;10:21641.
31. Gorimanipalli B, Shetty R, Sethu S, Khamar P. Vitamin D and eye: current evidence and practice guidelines. Indian J Ophthalmol. 2023;71(4):1127-1134.
32. Fogagnolo P, Sacchi M, Ceresara G, et al. The effects of topical coenzyme Q10 and vitamin E D-tocopheryl polyethylene glycol 1000 succinate after cataract surgery: a clinical and in vivo confocal study. Ophthalmologica. 2013;229(1):26-31.
33. Sarosiak A, Oziębło D, Udziela M, et al. High expression of matrix Gla protein in Schnyder corneal dystrophy patients points to an active role of vitamin K in corneal health. Acta Ophthalmol. 2021;99(2):e171-e177.
34. National Institutes of Health, Office of Dietary Supplements. Dietary Supplement Fact Sheets. Accessed March 26, 2024. https://ods.od.nih.gov/factsheets/list-all/#V