
The field of ophthalmology is characterized by a wealth of highly accurate, repeatable metrics. This is especially evident in cataract and refractive surgery, where rapid advances in computing, technology, and sensor development over the past decade have provided an influx of a vast amount of data. How can the potential of these data be maximized?
This article explores how to harness advanced data, precision tools, and machine learning to achieve optimal surgical outcomes in cataract and refractive surgery.
THE POWER OF PRECISION IN REFRACTIVE SURGERY
Refractive surgeons are fortunate to have access to some of the most precise instruments in medicine. Setting a new standard in surgical precision, the femtosecond laser achieves a standard deviation of approximately 4 µm, and the excimer laser achieves a standard deviation of 0.25 µm per pulse—a level so exact that it is also widely used in semiconductor manufacturing.
In refractive surgery, this precision is critical because a change of just 1.00 D equates to the removal of 12 µm of corneal tissue, according to the Munnerlyn formula for an optical zone of 6 mm. The current challenge is not only to gather but harness these data by leveraging the abundance of pre- and postoperative metrics to achieve better surgical outcomes.
QUALITY OVER QUANTITY: GETTING THE DATA RIGHT
Objective Versus Subjective Data
The potential for leveraging data in ophthalmology is immense, yet the foundation must be data quality; as the saying goes, “garbage in, garbage out.” Ophthalmology benefits from a wealth of objective measurements, distinguishing it from many other medical fields. Subjective metrics, however, such as manifest refraction and defocus curves, must be approached with caution.
Creating and Refining Nomograms
One of the most straightforward ways to use refractive surgery data is to develop nomograms for laser vision correction. Although third-party companies offer this service, creating nomograms internally can deepen surgeons’ understanding of the nuances and noise in their outcomes. Essentially, nomograms illustrate the line of best fit in an attempted-versus-achieved scatterplot; the dispersion of these data points reflects the surgical noise to minimize, thereby improving the R-squared value, which quantifies how well the model’s predictions align with observed outcomes of the regression line.
How can this noise be reduced and outcomes be enhanced? The answer is standardization.
STANDARDIZATION AS A KEY TO CONSISTENCY IN SURGERY
Lessons From Industry for Standardization
Industrial processes rely on precise sensors and metrics. Components are produced under consistent environmental controls, achieving uniformity and reproducibility. Refractive and cataract surgery can adopt similar standardization practices by drawing on industrial processes and using tools such as the excimer laser.
When applying these principles to LASIK, each surgery should be performed under standardized air conditions (temperature and humidity) and with consistent surgical techniques, tissue hydration levels, and procedural speed. Observing the impact of these details on cases, including the R-squared value in nomograms, can illustrate how variations in technique affect outcomes.
This attention to consistency—modeled in part after industrial standards—proves essential in high-precision fields such as refractive surgery. As Henry Ford wisely remarked, “If you think of standardization as the best that you know today, but which is to be improved tomorrow, you get somewhere.”
Advancing Cataract Surgery Through Data and Standardization
Robotic cataract surgery is under development, and debate about its potential advantages over manual procedures is ongoing. Femtosecond laser–assisted cataract surgery already provides enhanced reproducibility, precision, and customization for critical steps in cataract surgery.
Increasing the standardization of these procedures, especially when refining IOL constants and formulas, is essential for optimizing the performance of advanced technology IOLs, such as multifocal and extended depth of focus lenses, to deliver greater spectacle independence.
INTEGRATING CONNECTIVITY AND DATA PLATFORMS
Fully leveraging today’s data-rich environment demands connectivity. One need only imagine transforming all paper records and PDF reports from diagnostic devices into a continuous data stream stored in the cloud. In this model, data from each diagnostic station would populate a central, real-time spreadsheet, with thousands of metrics gathered throughout the preoperative workflow.
This comprehensive dataset enables algorithms to guide surgeons in selecting the most appropriate treatment for each case, thereby unlocking the full potential of data-driven, personalized cataract surgery.
Just as oil must be refined, careful curation of data is required to extract their value. Applying advanced algorithms or even machine learning tools can transform raw data into actionable surgical insights—a powerful evolution in personalized cataract surgery.
Overcoming Data Integration Challenges
Data extraction from ophthalmic equipment presents major challenges because different devices export information using various protocols (eg, Digital Imaging and Communications in Medicine [DICOM], Excel [Microsoft], Access [Microsoft]) and unified nomenclature across brands is often lacking.
Despite these obstacles, it is possible to develop a data platform customized to the equipment within a practice, allowing all relevant parameters to be collected simultaneously. Running a surgical algorithm on these data points could provide surgeons with a streamlined dashboard displaying only the most critical parameters (Figure 1). This could facilitate real-time decision-making and potentially improve patients’ visual outcomes.
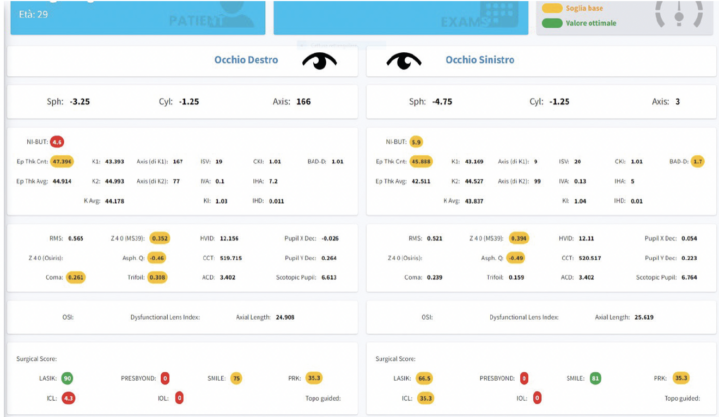
Figure 1. A customized dashboard highlighting the most crucial parameters to enhance surgical decision-making.
Developing Standardized Outcome Metrics
The next step is to standardize metrics for outcome measures such as patient satisfaction and improvements in visual acuity and quality of life. These metrics, however, are often subjective and highly dependent on effective communication between the physician and patient. The ideal scenario is one of “underselling and overdelivering.” In essence, patient satisfaction is maximized when their outcomes exceed their expectations.
Interestingly, studies have indicated that patient satisfaction rates following multifocal lens implantation have remained at approximately 90% for the past 3 decades and across multiple generations of lenses and technologies. This stability suggests a high level of proficiency in promoting lens technology but also emphasizes the need for more objective parameters to assess visual quality accurately.1,2
LEVERAGING TECHNOLOGY FOR OBJECTIVE VISUAL QUALITY ASSESSMENT
Fortunately, technological advances now allow objective measurements of visual quality using modern diagnostic tools.
Key Metrics for Image Quality Assessment
In an ideal optical system, a point object is viewed as a compact, high-contrast retinal image (Figure 2). This representation, known as the point spread function, is calculated as the squared magnitude of the inverse Fourier transform of the pupil function.

Figure 2. Measures of image quality for point objects are based on the contrast and compactness of the image.
For more complex objects, such as gratings, the modulation transfer function quantifies how image contrast varies with spatial frequency, and the phase transfer function describes how the image phase shifts with spatial frequency. Together, the modulation transfer function and phase transfer function compose the optical transfer function of the eye, which is computed as the Fourier transform of the point spread function.
Objective Defocus Curves and Aberrometry Devices
Collecting these data during follow-up examinations after surgery provides an objective and efficient means of assessing patients’ visual quality. These data can serve as crucial input for a machine-learning platform, where linear and nonlinear correlations with preoperative parameters can inform future surgical planning.
Additionally, modern aberrometry devices such as the Osiris (CSO; Figure 3) can generate objective defocus curves through high-quality sensors. These robust feedback data, when integrated into the platform, enhance its learning capacity and may facilitate optimal IOL selection for each eye, based on preoperative factors such as pupil aperture and dynamics.
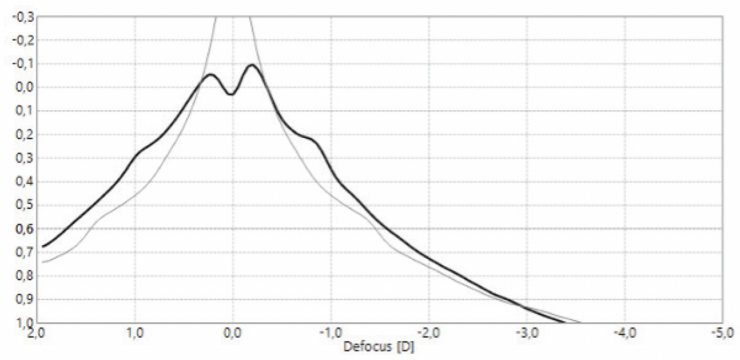
Figure 3. Objective defocus curve computed by the Osiris.
MACHINE LEARNING AND DATA-DRIVEN SURGICAL DECISIONS
After decades of developing high-quality sensors and computing power, the focus of ophthalmology may soon shift to software and information technology. Together with machine learning, these tools offer a path to continuous improvement in the quality of ophthalmic practice by leveraging objective outcomes data to drive strategic advances.
1. Lwowski C, Pawlowicz K, Petermann K, Hemkeppler E, Hinzelmann L, Böhm M, Kohnen T. Visual and patient-reported factors leading to satisfaction after implantation of diffractive extended depth-of-focus and trifocal intraocular lenses. J Cataract Refract Surg. 2022;48(4):421-428.
2. Chiam PJ, Chan JH, Haider SI, Karia N, Kasaby H, Aggarwal RK. Functional vision with bilateral ReZoom and ReSTOR intraocular lenses 6 months after cataract surgery. J Cataract Refract Surg. 2007;33(12):2057-2061.



