CASE PRESENTATION
A 27-year-old man presents for LASIK. The patient’s manifest refraction is -3.25 -1.00 x 180º OD and -5.50 -0.75 x 020º OS. Docking of the WaveLight FS200 femtosecond laser (Alcon) and creation of a LASIK flap (8.8-mm diameter and thickness of 110 µm) in each eye are uneventful.
Dissection of the flap in the right eye is initiated from the temporal side (at approximately the 10 clock position) by bringing the spatula toward the hinge. During dissection of the hinge (from temporal to nasal), the elbow of the spatula lifts, and the pressure exerted results in a tear (Figure 1). The eye then moves unexpectedly, causing the tear to extend nasally and completely severing the hinge (Figure 2; watch the video below).

Figure 1. The elbow of the LASIK spatula lifts instead of remaining flat, which causes the flap to tear at the hinge.
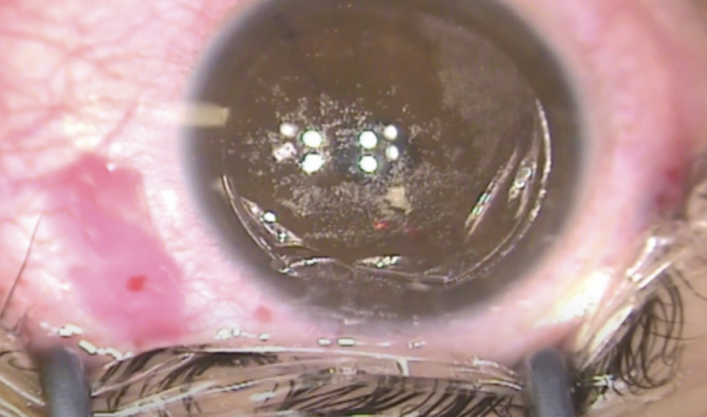
Figure 2. A completely severed flap hinge.
Would you continue with the LASIK procedure? If so, how would you handle the lack of hinge support? Alternatively, would you abort the procedure and return to the surgical suite later to perform surface ablation?
—Case prepared by Samir Melki, MD, PhD; Matthew Bickford, MD; and Nagib Salameh, BS

ROMESH ANGUNAWELA, BM, MD, FRCOPHTH, FRCSED, FWCRS, CERTLRS
The management of a total flap hinge tear during LASIK depends on the stage of surgery. Figures 1 and 2 show a well-centered flap with the remaining flap adhesions unseparated.
One option would be to separate the remaining flap, leave a nasal pseudo-hinge of adhesion, and complete the procedure as planned. Before proceeding, it would be important to ensure that the flap markings are clearly visible in case a free flap occurs.
If, however, the surgeon already separated the flap from the opposite side, creating a nasal or temporal hinge would be impossible. In this situation, an inferior hinge could be fashioned, and treatment completed. I have used this strategy in similar situations without adverse outcomes.
In my experience, the flap does not fold back as easily when a pseudo-hinge has been created and may have to be held down. An inferior hinge might be preferred if the flap were decentered and a nasal or temporal pseudo-hinge could impinge on the visual axis.
A pseudo-hinge should be shielded with a spear to protect the tissue from inadvertent ablation, which could cause haze or anomalous healing. Moreover, if the surgeon typically uses a large treatment zone independent of pupil size, it might be worth adjusting the optical zone size to avoid ablation of the pseudo-hinge. In cases like this one, if the original hinge has been traumatized, some surgeons apply mitomycin C for 10 to 15 seconds to discourage haze or scar formation.
If a free flap occurs, I would complete surgery, replace the flap (I always mark the flap before lifting it), carefully dry it into position, and place a bandage contact lens. I would instruct the patient to avoid rubbing the eye and wear a protective shield at night. I have yet to lose a flap.
How to proceed in this case depends on the surgeon’s confidence level. Although it is preferable to complete the case if it can be done safely, the ophthalmologist should not be criticized for aborting surgery and coming back another day. The patient's experience and confidence, however, may be reduced by the delay.

JONATHAN J. ROSS, MBCHB, MRCSED (EDIN), FRCPSG (GLAS), FRCOPHTH
The surgeon must immediately acknowledge that a free cap has been created and simultaneously bring their autonomic response under control. An optimal outcome and a reassured patient are the goal. The surgeon can verbally check in with the patient to boost his confidence and avoid causing unnecessary stress intraoperatively. There will be time later for an explanation of the case.
The correct orientation of the flap has been preserved. If orientation is lost, irregular astigmatism could arise. The video shows a nasal pseudo-hinge, which should be covered by a polyvinyl alcohol spear during excimer laser ablation. Upon completion of the procedure, the position of the flap should be monitored for 4 minutes to ensure it is correct before a bandage contact lens is placed.
If the cap occurred during surgery on the first eye of a bilateral case, it would be worth considering the technicalities of what happened, the patient’s disposition, and the surgeon’s comfort level before continuing. The level of refractive error (anisometropia) should also be taken into account. That said, the same complication is unlikely to occur twice.
Once surgery has been completed, the patient should be provided with verbal and written explanations of what happened as well as immediate and follow-up opportunities to discuss his concerns. He should be asked to see the same surgeon for future eye care. If that is not possible, the patient should receive written correspondence to present to other caregivers. The bandage lens should remain on the cornea for 2 days after treatment to stabilize the cap.



WHAT WE DID: SAMIR MELKI, MD, PHD; MATTHEW BICKFORD MD; AND NAGIB SALAMEH, BS
I (S.M.) took over from the operating surgeon. After assessing the flap, I gently completed the dissection but spared the nasal side of the flap cut to be used as the new hinge (Figure 3).
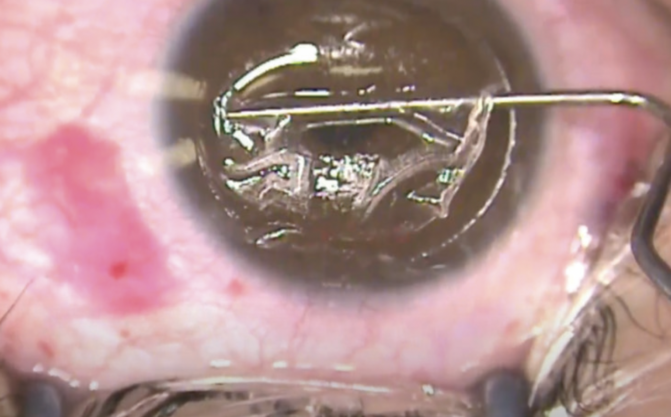
Figure 3. Dissection resumes. The nasal side cut is spared for use as a new hinge.
The flap was reflected nasally and gently pulled to provide sufficient exposure of the stromal bed (Figures 4 and 5). The optical zone size was reduced from 6.5 to 6.0 mm. Myopic LASIK treatment was performed successfully, and the flap was repositioned without incident (Figure 6).

Figure 4. The flap is reflected.

Figure 5. The undissected nasal side cut is used as the new hinge.
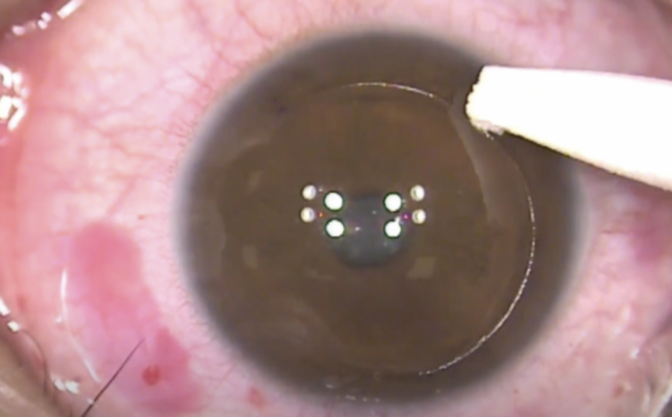
Figure 6. The flap is adequately repositioned at the conclusion of surgery.
One day after surgery, the patient’s UCVA was 20/15 OD and 20/20 OS.



