
In the clinical setting, the optical properties of the eye have been described in terms of lower-order aberrations (LOAs), otherwise referred to as sphere, cylinder, and cylinder axis. Although these types of optical errors can be easily corrected with techniques such as conventional LASIK and PRK,1 classical LASIK ablation patterns have been demonstrated to induce complex aberrations, designated higher-order aberrations (HOAs). In short, HOAs are thought to be responsible for some of the visual disturbances reported by patients after refractive surgery, such as glare, halos, and starbursts.2-4
Innovations in ablation profile design, excimer laser design, and diagnostic equipment have allowed surgeons to correct not only LOAs but also to minimize HOAs, increasing the levels of postoperative efficacy, predictability, and visual quality.5 Even so, the management of significantly irregular corneas is still a challenge for refractive surgeons.
The use of wavefront-guided laser technology for the management of aberrated corneas has been shown to effectively reduce HOAs in corneas with previous keratorefractive surgeries that have left residual refractive errors.6-9 Wavefront-guided technology has also shown efficacy in addressing irregularity in pathologic corneas once their biomechanical weakening has been overcome by application of CXL.10 However, limitations of wavefront-guided procedures have been described, mainly related to the technical limitations of aberrometers in measuring ocular aberrations.11 The accuracy of Hartmann-Shack wavefront sensing, which is the most widely used approach to aberrometry in clinical practice, depends on the size of the spots and bit resolution of the system's camera.12
AN ADVANCED TOOL
A newer generation of Hartmann-Shack aberrometer (iDesign Advanced WaveScan Studio System; Abbott Medical Optics) now provides an advanced tool for performing highly accurate wavefront-guided excimer laser refractive surgery. In addition to wavefront aberration analysis, the system also performs autorefraction, complete topographic analysis, keratometry, and pupillometry with a single capture, maximizing the benefits of single-device diagnostics and treatment options.
At a Glance
• In a series of myopic patients treated with wavefrontguided
LASIK with the iDesign platform, significant
improvement from preoperative BCVA to postoperative
distance UCVA was observed.
• Similar results were seen in a separate interventional case
series of 20 consecutive eyes with significantly aberrated
corneas in 18 patients undergoing wavefront-guided laser
vision correction.
Analyzing up to 1,257 data points for a 7-mm pupil, the iDesign has a dynamic range of -16.00 to 12.00 D of sphere, 0.00 to 8.00 D of cylinder, and up to 8 µm of root mean square (RMS) HOA. One of the most interesting advances of this aberrometer is that data reconstruction is performed using a Fourier algorithm, equivalent in resolution to 20th-order Zernike analysis.
The iDesign system calculates the individual treatment for each patient, and the STAR S4 IR excimer laser (Abbott Medical Optics) translates it into a customized ablation in what the manufacturer calls an Advanced CustomVue procedure. The excimer laser uses an iris registration (IR) system with eye tracking to provide alignment of the treatment during the procedure, avoiding the use of the imprecise reference of the pupil for the purpose.13
RESULTS IN TWO SERIES
Series No. 1. At the Horus Vision Center, we evaluated the visual, refractive, and aberrometric outcomes in myopic eyes undergoing wavefront-guided LASIK using this advanced laser platform. This was a prospective, consecutive, noncomparative study including 40 myopic patients with preoperative sphere of up to -8.00 D and cylinder of up to -6.00 D.14
CASE EXAMPLES from series no. 2
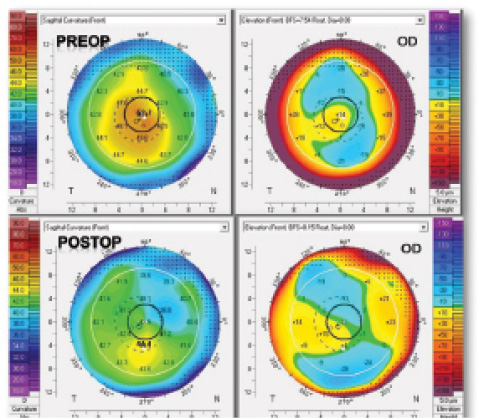
Figure 1. Corneal topographic map of a crosslinked keratoconic cornea before and after wavefront-guided PRK performed with the Advanced CustomVue laser platform.
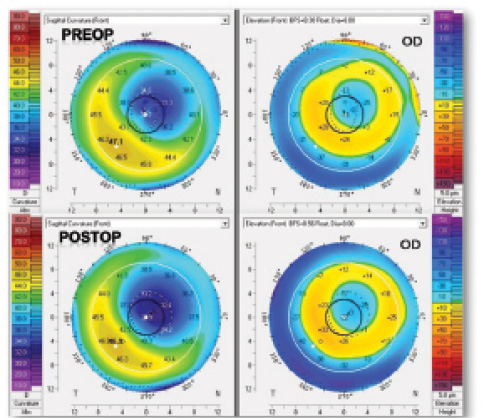
Figure 2. Corneal topographic map of an irregular cornea due to a decentered LASIK procedure before and after wavefront-guided LASIK enhancement performed with the Advanced CustomVue laser platform.
In this series, significant improvement from preoperative BCVA to postoperative distance UCVA was observed (P<.01). At 3 months postoperative, 23% of eyes achieved 20/16 or better UCVA, compared with 12% of eyes with 20/16 BCVA preoperatively. Also at 3 months, 86% of eyes achieved 20/20 or better UCVA, compared with 79% of eyes with 20/20 or better BCVA preoperatively (Figure 1).
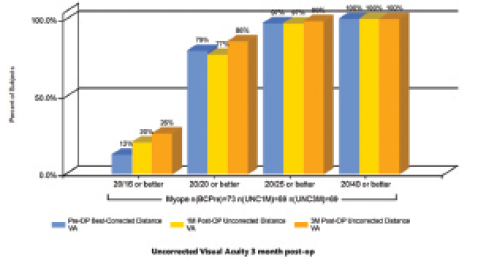
Figure 1. UCVA outcomes at 3 months postoperative in a series of myopic eyes undergoing wavefront-guided LASIK.
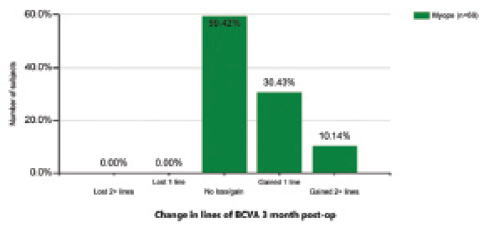
Figure 2. Change in lines of distance BCVA at 3 months postoperative in a series of myopic eyes undergoing wavefront-guided LASIK.
The preoperative level of distance BCVA was maintained postoperatively in most eyes and even improved with surgery in some. Postoperatively, 40.6% of eyes gained lines of distance BCVA, and no eyes lost lines of distance BCVA (Figure 2). This was consistent with a significant reduction in spherical equivalent (P<0.01), with 97.2% of eyes having a postoperative value within ±0.25 D.
Regarding HOAs, minimal induction of primary spherical aberration (at a 5-mm pupil) was found in the myopic group, as might be expected considering that the ablation profile was designed with that purpose. HOAs changed from a mean preoperative value of 0.03 ±0.08 µm to a mean postoperative value of 0.04 ±0.08 µm (P=.16).
Series No. 2. We also recently conducted a prospective interventional case series including 20 consecutive eyes with significantly aberrated corneas in 18 patients undergoing wavefront-guided laser vision correction with the Star S4 IR excimer laser platform. Of the patients enrolled, 10 (11 eyes) had keratoconus with previous CXL (epithelium-off), five (five eyes) had previous decentered LASIK treatments, and three (four eyes) had previous RKs that had left significant levels of corneal irregularity. The patients who had previous CXL underwent wavefront-guided PRK instead of LASIK. At 3 months postoperative, all eyes gained 1 or more lines of distance BCVA that was associated with a reduction in spherical equivalent (P≤.04) and in magnitude of manifest cylinder of 50% or more (P<.01).
In the keratoconic eyes, a significant visual improvement was associated with an increase in contrast sensitivity and some degree of HOA correction (see Case Examples from Series No. 2). In the eyes with previous decentered LASIK treatments, a significant reduction of primary coma was observed after relifting of the flap and application of a wavefront-guided ablation to optimize the corneal and ocular optics. There was also a significant improvement in distance BCVA and mesopic contrast sensitivity in these eyes.
CONCLUSION
The combination of the precise aberrometric measurements provided by the iDesign System and treatment with the Star S4 IR excimer laser allows refractive surgeons to perform wavefront-guided LASIK with excellent safety, efficacy, and predictability in myopic eyes, preserving the visual quality of the eye. Likewise, ocular wavefront-guided LASIK and PRK enhancement using the Advanced CustomVue platform is an effective option to correct the spherocylindrical error and to restore visual quality in eyes with significantly aberrated corneas. This platform is a step forward in excellence in corneal refractive surgery, allowing successful performance of all types of refractive surgical treatments, even in highly aberrated corneas. n
1. Koller T, Iseli HP, Hafezi F, Mrochen M, Seiler T. Q-factor customized ablation profile for the correction of myopic astigmatism. J Cataract Refract Surg. 2006;32:584-589.
2. Mrochen M, Donetzky C, Wüllner C, Löffler J. Wavefront-optimized ablation profiles: theoretical background. J Cataract Refract Surg. 2004;30:775-785.
3. Holladay JT, Dudeja DR, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing and corneal topography. J Cataract Refract Surg. 1999;25:663-669.
4. Chalita MR, Chavala S, Xu M, Krueger RR. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction and topography. Ophthalmology. 2004;111:447-453.
5. Schallhorn SC, Tanzer DJ, Kaupp SE, Brown M, Malady SE. Comparison of night driving performance after wavefront-guided and conventional LASIK for moderate myopia. Ophthalmology. 2009;116:702-709.
6. Alió JL, Piñero DP, Plaza Puche AB. Corneal wavefront-guided enhancement for high levels of corneal coma aberration after laser in situ keratomileusis. J Cataract Refract Surg. 2008;34:222-231.
7. Alió JL, Piñero D, Muftuoglu O. Corneal wavefront-guided retreatments for significant night vision symptoms after myopic laser refractive surgery. Am J Ophthalmol. 2008;145:65-74.
8. Hiatt JA, Grant CN, Wachler BS. Complex wavefront-guided retreatments with the Alcon CustomCornea platform after prior LASIK. J Refract Surg. 2006;22:48-53.
9. Kanellopoulos AJ, Pe LH. Wavefront-guided enhancements using the wavelight excimer laser in symptomatic eyes previously treated with LASIK. J Refract Surg. 2006;22:345-349.
10. Kymionis GD, Kontadakis GA, Kounis GA, et al. Simultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconus. J Refract Surg. 2009;25:S807-811.
11. López-Miguel A, Maldonado MJ, Belzunce A, Barrio-Barrio J, Coco-Martín MB, Nieto JC. Precision of a commercial Hartmann-Shack aberrometer: limits of total wavefront laser vision correction. Am J Ophthalmol. 2012;154:799-807.
12. Akondi V, Vohnsen B. Myopic aberrations: impact of centroiding noise in Hartmann Shack wavefront sensing. Ophthalmic Physiol Opt. 2013;33:434-443.
13. Khalifa M, El-Kateb M, Shafik Shaheen M. Iris registration in wavefront-guided LASIK to correct mixed astigmatism. J Cataract Refract Surg. 2009;35:433-437.
14. Shafik M. Wavefront-guided treatment of irregular corneas using high resolution aberrometer. Paper presented at: the ASCRS/ASOA Symposium and Congress; April 25-29, 2014; Boston.
Mohamed Shafik Shaheen, MD, PhD
• Department of Ophthalmology, University of Alexandria, Egypt
• Horus Vision Correction Center, Alexandria, Egypt
• m.shafik@link.net
• Financial disclosure: None
