
I am a firm believer in the benefits of premium IOLs for patients who desire less dependence on spectacles after cataract surgery. Toric and presbyopia-correcting IOLs offer a wonderful opportunity for cataract patients with otherwise healthy eyes to regain some of their youthful range of vision.
One of the biggest mistakes cataract surgeons can make, however, is to ignore the tear film. Ocular surface disease (OSD) is extremely common in the cataract-age population. Many individuals do not seem particularly symptomatic preoperatively despite the presence of ocular surface changes. If these silent problems are not detected and addressed prior to surgery, refractive surprises can occur, and surgeons will have unhappy patients. Additionally, if ophthalmologists fail to alert patients to the presence of OSD before surgery, patients may blame the surgery or their surgeon for their postoperative dry eye disease (DED).
DED AFFECTS THE PREOPERATIVE WORKUP
The impact that DED has on the accuracy of the preoperative measurements (eg, keratometry, topography, and wavefront analysis) used for IOL power calculation and astigmatism correction is monumental (Figure 1). If the lens power or the axis calculation is based on unreliable data, one cannot expect to achieve optimal visual outcomes with any IOL, let alone with an implant that has complex multifocal or toric optics.
Unfortunately, this situation was clearly illustrated in a recent case that necessitated an IOL exchange. The patient, a pharmaceutical company executive with demanding visual acuity needs, had a toric IOL implanted elsewhere. Her surgery was flawless, with a well-placed toric IOL in the bag. When I saw her, she had significant complaints of blurred vision in her operated eye, making it impossible for her to drive at night. Lissamine green showed marked corneal and conjunctival staining in both eyes. These DED problems, I would guess, were present preoperatively. The original surgeon had not only ignored her preexisting OSD but had also performed the lens power measurements immediately after the removal of the one contact lens the patient wore for near vision correction. Dryness and contact-lens–related corneal changes masquerading as astigmatism resulted in the selection of a toric IOL for a spherical cornea (Figure 2).
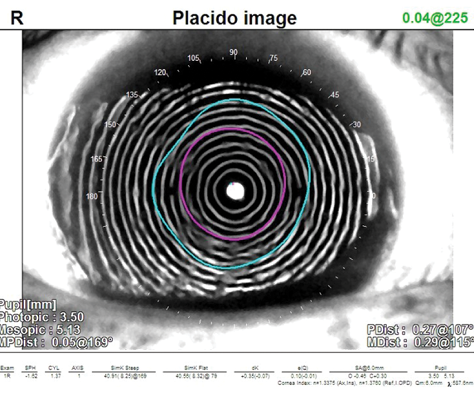
Figure 1. The irregularity and warpage in the rings on this Placido-disc image are indicative of significant OSD that should be treated prior to preoperative measurements.
Following IOL exchange with removal of the toric IOL and insertion of a monofocal IOL, the patient now has a visual acuity of 20/20, and she is happy. The second surgical procedure and months of dissatisfaction could have been avoided.
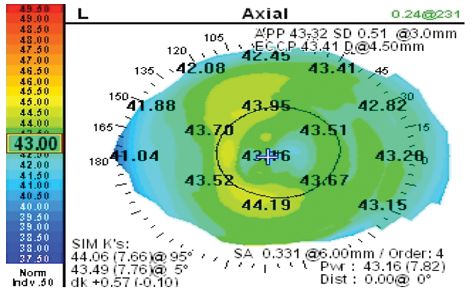
Figure 2. Tear film abnormality secondary to dry eye and corneal surface irregularity due to contact lens wear masquerading as pseudoastigmatism, leading to incorrect lens selection.
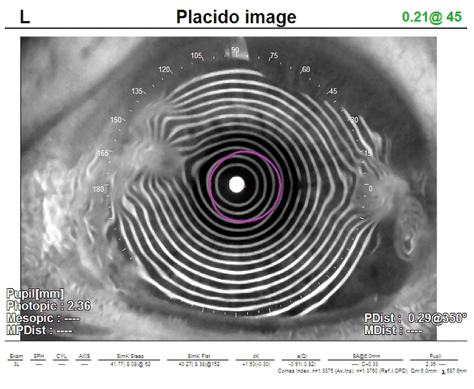
Figure 3. Salzmann nodular corneal dystrophy: The nodules are clearly seen in the Placido-disc image.
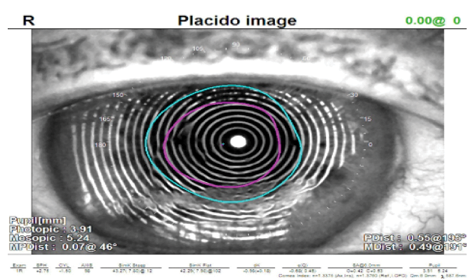
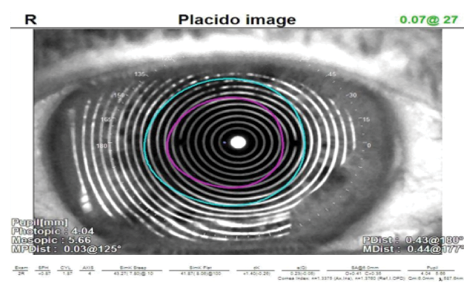
Figure 4. Placido-disc rings with significant distortion in a patient with dry eye (A). The same patient after 1 month of treatment with cyclosporine 0.05% ophthalmic emulsion. The surface looks more regular, indicating readiness for preoperative measurements (B).
SCREEN FOR DRY EYE
I carefully evaluate the ocular surface of every patient scheduled for a cataract consultation. Considered a lens-based refractive procedure now, cataract surgery has to be approached with the same precision as cornea-based refractive procedures. I test for and treat DED aggressively before proceeding with preoperative measurements—even if that means delaying surgery by weeks or months.
Cataract patients in my practice receive tear osmolarity testing (TearLab Osmolarity System), which the staff performs before I examine the patient. The higher the osmolarity above 300 mOsms/L, the more advanced the disease. I like to see an osmolarity result that is less than or equal to 300 mOsms/L.1 The two eyes should also be similar, because a difference of more than 8 mOsms/L is another sign of DED. Moreover, I evaluate the lid margin, conjunctiva, and cornea with lissamine green.
Data and images from the OPD-Scan III Corneal Analyzer (Nidek) are increasingly important to me in both diagnosis and patient education. In particular, I look at the Placido-disc images. In a healthy eye, I would expect to see clear, even, concentric rings. If the rings are wavy or missing, that is an indication of OSD. Anecdotally, I find there to be a correlation between the images and osmolarity values. Eyes with Placido-disc images that are very distorted, such as the one in Figure 1, usually have abnormal tear osmolarity results.
USE IMAGES TO EDUCATE
Placido-disc topography makes it easy to visually explain DED to patients because it does not require special knowledge or sophistication to understand whether the rings are clear and regular. A picture is worth a thousand words, and I show the images to the patient and his or her family on a big-screen monitor in the examination room. If the patient has OSD, I explain the need to treat it before taking any surgical measurements in order to ensure the best refractive outcomes.
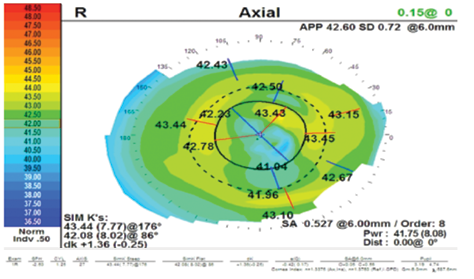
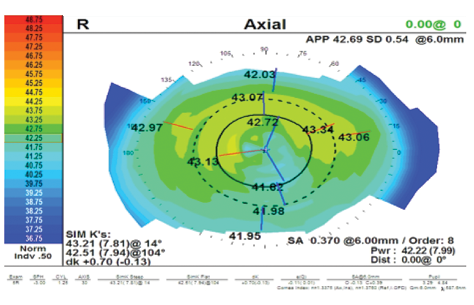
Figure 5. Tear film abnormality in a patient with DED demonstrating false higher astigmatism: Dk 1.36 D (A). The same patient after 2 weeks of treatment; the astigmatism was reduced to Dk 0.70 D (B).
The Placido-disc images enable patients to better understand the chronicity of their condition and its impact on their vision. The need to delay cataract surgery to optimize the ocular surface becomes easier to explain. The Placido-disc images also help me rule out patients who are not multifocal IOL candidates. For example, a patient who recently presented for cataract surgery had Salzmann nodular corneal dystrophy—a slowly degenerative condition characterized by grayish-white nodules in the peripheral cornea typically affecting both eyes. These raised nodules, clearly visible on the Placido-disc picture, alter the tear film and cause irregular astigmatism (Figure 3).
The nodules can be removed easily, but, in this case, the patient declined the treatment. Consequently, I explained to her that she was not a good candidate for a multifocal IOL and that she might not achieve a visual acuity of 20/20 due to her corneal pathology.
TREAT AND FOLLOW PROGRESS
I save images and use them on subsequent visits to demonstrate progress (or lack thereof). This helps patients visualize how much their ocular surface has improved. Figure 4 show a patient with OSD and 1 month after treatment with cyclosporine ophthalmic emulsion 0.05% (Restasis; Allergan) twice daily. Compliance with and adherence to a dosing regimen is enhanced when patients have a way to see their improvement.
The treatment protocol and the wait time before capturing surgical measurements are personalized for each patient. At a minimum, I start every patient scheduled for cataract surgery on preservative-free artificial tears four times a day for 2 weeks before they return for their keratometry, topography, and biometry appointment. Depending on the type and severity of OSD, I may add cyclosporine, oral omega-3 supplements, loteprednol 0.5% gel drops or ointment (Lotemax; Bausch + Lomb), a microwavable hydrating heat mask, and/or intense pulsed light therapy. I may wait as long as 2 months before performing preoperative measurements.
At a Glance
• Without a proactive OSD screening approach, surgeons may miss dry-eye–related tear film pathology in their cataract patients.
• Most patients can be readied for surgery in a relatively short period.
• Placido-disc images can be saved and used on subsequent visits to demonstrate progress (or lack thereof).
Most patients can be readied for surgery in a relatively short period. In one recent patient, for example, the initial images looked quite distorted (Figure 5A), but there was no sign of lid disease. I initiated aggressive treatment. A few weeks later, the ocular surface had improved (Figure 5B), at which time, we proceeded with the preoperative measurements.
CONCLUSION
Without a proactive OSD screening approach, surgeons may miss dry-eye–related tear film pathology in their cataract patients. With unreliable preoperative data, the postoperative refractive outcomes may not only yield refractive surprises but also cause disappointment in the patient. In my experience, OSD is responsible for some of the dissatisfaction with multifocal IOLs and for some of the miscalculations of axis and magnitude for toric IOLs. By carefully evaluating and educating patients preoperatively and treating DED appropriately, eye care providers can improve success rates with premium IOLs. n
1. Foulks GN, Lemp MA, Berg M, et al. TearLab osmolarity as a biomarker for disease severity in mild to moderate dry eye disease. Poster presented at: The American Academy of Ophthalmology Annual Meeting; October 24-27, 2009; San Francisco.
Cynthia Matossian, MD
• Founder and CEO, Matossian Eye Associates, Pennsylvania and New Jersey
• Clinical Instructor, Department of Ophthalmology, Temple University School of Medicine, Philadelphia
• cmatossian@matossianeye.com
• Financial disclosure: Consultant, Speaker (Abbott Medical Optics, Allergan, Bausch + Lomb, Nidek, PRN, TearLab)

