Cataract surgery is one of the most frequently performed surgeries worldwide. In Germany, 700,000 to 800,000 cataract surgeries are performed annually, and approximately 100,000 of these are completed as inpatient procedures.1 One of us (TK) has performed more than 3,350 femtosecond laser cataract and refractive surgeries since 2012. This is now our routine procedure for cataract surgery; it is outlined here and in an accompanying Eyetube video at bit.ly/kohnen0220.
Patients present to our eye clinic for the treatment of cataract and also when they desire spectacle independence. If a patient wishes to be independent from glasses and no visually significant cataract is present, a refractive lens exchange is performed. When a cataract is present, we schedule the patient for cataract surgery. In either case, after a preliminary examination including an IOL assessment, the best-suited lens is ordered and, once the IOL has been delivered to the surgical center, the outpatient procedure is scheduled. The eyes are operated on two different days with typically a 1- to 5-day interval between the surgeries. In rare cases, cataract surgery is performed under general anesthesia.
SURGICAL PREPARATIONS
The patient registers on the day of the surgery for the outpatient procedure. After the patient has been admitted, the nursing staff takes his or her medical history, which includes heart rate, blood pressure, and blood sugar. While the patient is prepped for surgery, the following medications are administered:
- A mydriatic solution (phenylephrine HCl 2.5%) as required for pupillary dilatation;
- tropicamide 0.25%, also to dilate the pupils;
- A midazolam 3.75 mg (Dormicum, Roche Pharma) sedative tablet; and
- Optional medication if the patient is agitated and restless before the procedure.
For laser cataract surgery, we use the digital measurement unit of the Verion Image Guided System (Alcon) to take two images of the patient's eye, one with the patient in a seated position prior to surgery and one later, in the OR, with the patient in supine position. The blood vessels and iris pigmentation serve as landmarks, and the two images are used intraoperatively for IOL positioning and to determine the cyclorotation of the eye. The latter can be compensated by intraoperative image comparison with the help of the LenSx Laser System (Alcon). We also remeasure the biometry of the patient's eye before the start of surgery.
Once these steps are completed, a member of the nursing staff explains the course of the subsequent surgery to the patient. The patient, who has been waiting in a resting area in a reclined position, is then brought to the OR and prepared for surgery. In a supine position on the operating table, the patient is connected to a blood pressure monitor. The surgical staff aligns the surgical bed with the patient under the femtosecond laser and centers the laser on the eye that is to be treated.
SURGERY BEGINS
The surgeon inserts the eyelid speculum into the patient's eye. Next, the patient interface is connected to the laser and the surgeon aligns the interface with the patient's eye. The patient assists the surgeon by changing viewing direction as instructed by the surgeon. Finally, contact between the eye and the laser is established. Once suction is achieved, the surgeon compares the preoperative image (acquired with the patient in seated position) with the intraoperative image (acquired with the patient in supine position). The cyclorotation of the eye is then compensated by superimposing the images and rotating them clockwise or counterclockwise.
At this stage, the surgeon checks three things: that there is adequate suction with the patient interface, that no air bubbles are present in the surgical field, and that no eyelashes are visible between the interface and the patient's eye. The surgeon then uses the femtosecond laser to perform the capsulotomy, lens fragmentation in the form of a cube cut pattern, a 2.3-mm temporal incision, and two 1.8-mm paracenteses located 45° away from the main incision. The laser portion of the procedure is controlled by the integrated OCT, and the IOP is also monitored while the femtosecond laser is working. After the incisions have been cut, the eye is released from suction and the surgeon removes the eyelid retractor.
Next, the patient is aligned under an LX3 microscope (Alcon), and the surgeon preps the eye for lens removal by covering the eye with an incision foil and gluing the eyelashes in place. The surgeon then cuts the foil open with blunt Bonn scissors, inserts a lid speculum, and opens the paracenteses and main incision with a hand spatula. Using tweezers, the surgeon then removes the laser-cut anterior capsule.
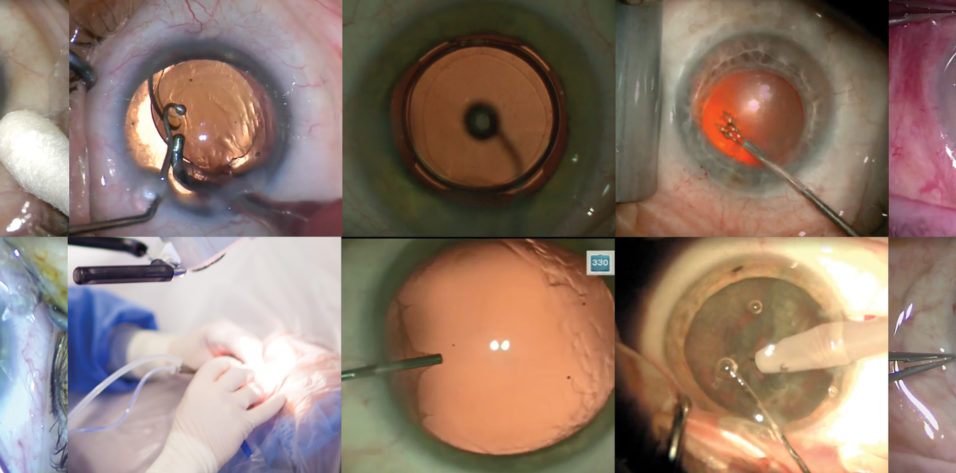
At the start of hydrodissection, the surgeon injects ProVisc 0.55 mL (Alcon) into the eye to facilitate lens removal (Figure 1) as well as 1% xylocaine on a 3-mL luer-lock syringe for anesthesia.

Figure 1. OVD is injected into the eye prior to lens emulsification.
Inserting the phaco handpiece through the main incision and a push-pull instrument through one of the two paracenteses, the surgeon begins emulsifying and aspirating the lens (Figure 2). Depending on the cataract density, removal of the lens may take some time. In advanced cataracts, increasing ultrasound energy can help to achieve more efficient removal.

Figure 2. The lens is emulsified and aspirated with the phaco tip and a push-pull instrument.
The lens cortex remnants must also be completely removed (Figure 3), as any residue can lead to postoperative complications such as formation of posterior capsular opacification or ocular inflammation.2 After lens removal, the surgeon injects Healon (Johnson & Johnson Vision) or ProVisc to stabilize the anterior chamber.3 In patients older than 75 years, Healon5 (Johnson & Johnson Vision) is substituted.

Figure 3. Nuclear remnants are removed from the eye.
IOL INSERTION
The surgical assistant opens the packaging of the IOL and hands it to the surgeon, who uses lens implantation forceps to remove the IOL from the sterile packaging (Figure 4). The surgeon carefully folds the haptics of the IOL with Utrata forceps and precisely positions the lens in the cartridge. The cartridge is clicked into the lens injector. The IOL can then be pushed forward with light pressure on the injector so that the lens is placed in the front of the injector. This can also be performed by the nurse. The surgeon then places the injector into the main incision and implants the IOL into the capsular bag.

Figure 4. The IOL is removed from its sterile packaging with lens implantation forceps.
During IOL implantation, the patient is instructed to look toward the injector so that the eye does not turn away during the injection. Using a push-pull instrument, the surgeon centers the IOL in the capsular bag. If a toric IOL is being implanted, the axis of alignment is displayed in the microscope oculars. After the IOL is implanted, the surgeon manually removes the OVD and any lens remnants from both incision points with an I/A probe. After all OVD and lens remnants have been removed, the surgeon checks the final lens position and, in the case of toric lenses, ensures that the lens aligns with the marked axis position. Finally, the surgeon centers the IOL.
The last step of the procedure is administration of cefuroxime, assembled in the university’s local pharmacy, with an enzyme cannula. After checking the wound closure and the anterior chamber stability with a swab, the surgeon removes the lid speculum and incision foil. The eye is disinfected with povidone-iodine, and pilocarpine 2% drops are administered to reverse the pupillary dilation. The eye remains closed and is covered with a cotton swab for 1 day.
POSTOPERATIVE CARE
The nursing staff assists the patient from the operating table to a recovery room where the patient’s vital signs are monitored. The surgeon's documentation is completed in the OR, and the file is passed to the ward staff so that they can document the patient’s heart rate, blood pressure, and blood sugar. The patient is given an acetazolamide tablet to prevent a postoperative increase in IOP.
Postoperatively, the patient lies supine for 1 hour on a bed in the resting area so that the lens retains its position in the eye. After the 1-hour rest period, the pupil is checked. The nursing staff continues to assist the patient with walking until the patient feels steady. Postoperative follow-up appointments are scheduled for day 1, week 1, and month 1 postoperatively.
Prescriptions for pain relief and inflammation inhibition and a discharge letter are given to the patient. Our routine postoperative antiinflammatory regimen is most commonly an NSAID such as diclofenac sodium (Pharma Stulln) four times daily or nepafenac 3% (Nevanac, Novartis Pharma) once daily for 6 weeks and a steroid such as dexamethasone sodium phosphate ophthalmic solution (Bausch + Lomb) four times daily for 2 weeks. NSAIDs are administered to prevent and relieve eye pain and inflammation of the anterior segment after cataract surgery and to reduce the risk of macular edema.4-7 Patients are no longer treated with antibiotics postoperatively. If necessary, a taxi is ordered for the patient to travel home. The operated eye is uncovered and checked the next day at the 1-day follow up.
1. Berufsverband der Augenärzte Deutschlands e.V. Augenärzte informieren: Katarakt [in German]. http://cms.augeninfo.de/nc/hauptmenu/presse/statistiken/statsitik-katerakt. Accessed November 29, 2019.
2. Taneri S, Heiligenhaus A. Infections after intraocular lens surgery: implications for refractive surgery. Klin Monbl Augenheilkd. 2012;229(9):910-916.
3. Cavallini GM, Campi L, Delvecchio G, Lazzerini A, Longanesi L. Comparison of the clinical performance of Healon 5 and Healon in phacoemulsification. Eur J Ophthalmol. 2002;12(3):205-211.
4. Lwowski CM, de Robaulx AC, Kohnen T. Peri-/postoperative antiinflammation therapy after cataract and refractive surgery. Klin Monbl Augenheilkd. 2019;236(5):636-646.
5. Wielders LHP, Schouten JSAG, Winkens B, van den Biggelaar FJHM, Veldhuizen CA, Findl O. European multicenter trial of the prevention of cystoid macular edema after cataract surgery in nondiabetics: ESCRS PREMED study report 1. J Cataract Refract Surg. 2018;44(4):429-439.
6. Kim SJ, Schoenberger SD, Thorne JE, Ehlers JP, Yeh S, Bakri SJ. Topical nonsteroidal anti-inflammatory drugs and cataract surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2015;122(11):2159-2168.
7. Duan P, Liu Y, Li J. The comparative efficacy and safety of topical non-steroidal anti-inflammatory drugs for the treatment of anterior chamber inflammation after cataract surgery: a systematic review and network meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2017;255(4):639-649.