International humanitarian missions can be mutually beneficial experiences. My fellow volunteers and I bring state-of-the-art medical and surgical technologies to help us make diagnoses and treat indigent patients, and we offer education and skills transfer to local physicians and staff. In exchange, we receive the heartfelt gratitude of patients and providers, gain experience handling some of the most challenging cases of our careers, and encounter unusual and rare conditions that we might never otherwise see.
Despite the use of long, detailed checklists, we frequently encounter challenges that require equipment we do not have with us. As a result, we must exercise a high level of creativity. In this situation, we must prioritize patient safety and well-being when developing an approach to the problem—whether it is a simple alternative to facilitate an eye examination, the substitution of nonophthalmic tools to complete complex surgery (Figure at outset), or the combination of several surgical techniques to meet a unique challenge.
SURGICAL EQUIPMENT AND SUPPLIES
Even compact tabletop autoclaves can be heavy and challenging to ship to remote mission sites. We have therefore used portable, cassette-based, rapid-cycle autoclaves such as the Statim 2000 (Statim USA; Figure 1) for many years. These units are much smaller and lighter than standard autoclaves. They have sterilization cycles as short as 6 minutes, and the cassette tray holds a phaco handpiece and all instruments required for cataract surgery or instruments for any other anterior segment, glaucoma, strabismus, or oculoplastic procedure.1,2

Figure 1. Portable cassette-based, lightweight autoclaves with short sterilization cycles are convenient for transport and use in eye mission settings.
When a large surgical cautery unit is not available, a much smaller one such as a Surgitron radiofrequency unit (Ellman) can be used. Even a simple handheld battery-powered cautery device such as a high-temperature cautery (Optemp, Alcon; Accu-Temp, Beaver-Visitec International or Bovie), can provide cutting and cautery for eyelid surgery.
Occasionally, a slit-lamp or surgical microscope bulb burns out. If no replacement is available, we have removed the bulb and inserted an LED flashlight (Figure 2), which has provided excellent illumination and allowed us to continue using the slit lamp or microscope for examinations or surgery.

Figure 2. The light source wiring was defective in this slit lamp, and bulb replacement did not help (A). A bright 450-lumen, single-bulb LED small portable flashlight fit perfectly into the light source chamber (B) and provided excellent illumination for patient examinations throughout the mission (C). Dr. Purdy has used this technique for surgical microscopes as well. Having extra batteries on hand can be helpful for prolonged use.
Regulations prohibit many medical supplies from being sterilized and reused in the United States. Many of the disposables we use in ophthalmic surgery, however, can be cleaned, irrigated, sterilized, and safely reused three or four times before being discarded.3,4 These include irrigating cannulas, cystotomes, phaco tips, cataract and paracentesis blades, the Malyugin Ring (MicroSurgical Technology), iris hooks, cautery handpieces, bone burrs, and many more surgical devices and supplies.
CATARACT AND ANTERIOR SEGMENT SURGERY
Some mission projects have excellent surgical microscopes, phaco units, and all the other equipment typically used for cataract surgery. In remote areas, however, it may not be feasible to bring large, heavy phaco machines, and it may be impossible to obtain enough expensive phaco cassette packs to permit the continuous, ongoing use of these machines. The use of manual small-incision cataract surgery (MSICS) can be particularly helpful in this setting. A dozen different MSICS techniques have been described over the years, and I recommend that cataract surgeons master at least a few of these.
The miLoop (Carl Zeiss Meditec) can be useful for MSICS as well as for manual nuclear segmentation during various phaco techniques. This handheld device can easily bisect most dense cataracts, allowing the nuclear fragments to be removed through a smaller incision (Figure 3).
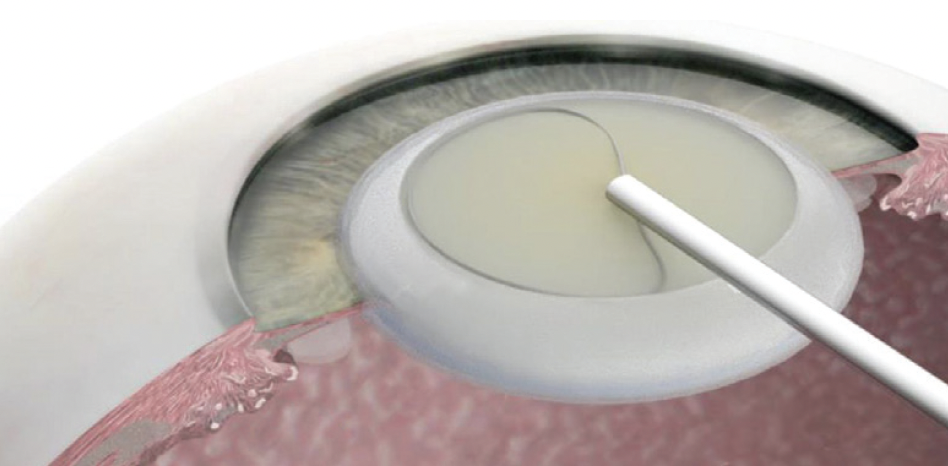
Figure 3. The miLoop can be useful in mission settings, especially when phaco equipment is not available and various MSICS techniques are being used. The nitinol flexible wire loop of the device is gently placed around the nucleus and then tightened to transect the nucleus into two or more segments.
Even when phaco equipment is available in a mission setting, it occasionally breaks down. When this occurs, cataract surgery may come to a halt unless the surgeon can implement either an extracapsular or MSICS technique.
STRABISMUS SURGERY
We have taken ophthalmology residents with us on mission projects since 2006. They help with large preoperative patient screening clinics and postoperative examinations, and they assist in surgeries.
These experiences can teach residents to think outside the box. For example, one of the University of Cincinnati residents assisting me on a bilateral lateral rectus recession for exotropia in Honduras developed a helpful technique for using traction sutures for the medial rotation of both globes to allow each of us to operate on a lateral rectus muscle simultaneously. The technique requires placing a lateral perilimbal traction suture on each eye, then tying the ends together over the nasal bridge to rotate each globe medially (Figure 4).
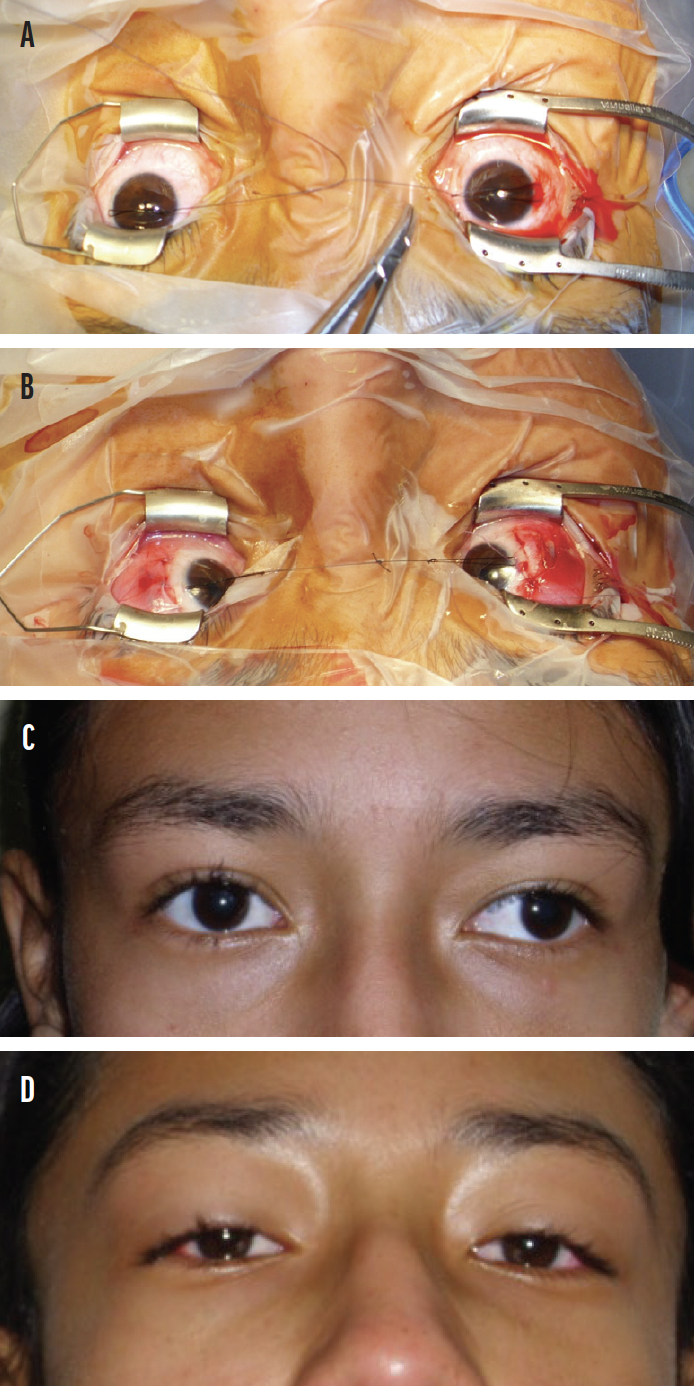
Figure 4. Bilateral limbal traction sutures were tied together to facilitate simultaneous two-surgeon bilateral lateral rectus recession surgery without the interference of long traction sutures and hemostats draping over each contralateral eye during surgery (A, B). The eyes before (C) and after (D) surgery.
OCULOPLASTIC, ORBITAL, AND LACRIMAL SURGERY
The broad diversity of surgical techniques used in oculoplastic surgery requires surgeons to have a high level of creativity on mission trips. Various tissue flaps, grafts, or alloplastic implants can be used to achieve excellent results after the reconstruction of large defects for large tumor resections, trauma, burns, or congenital disorders. In some complex cases, it may be necessary to use a combination of several techniques, including myocutaneous, tarsoconjunctival, and periosteal flaps; full-thickness skin, mucous membrane, and dermis-fat grafts; orbital or eyelid implants; and/or lacrimal tubes (Figure 5).
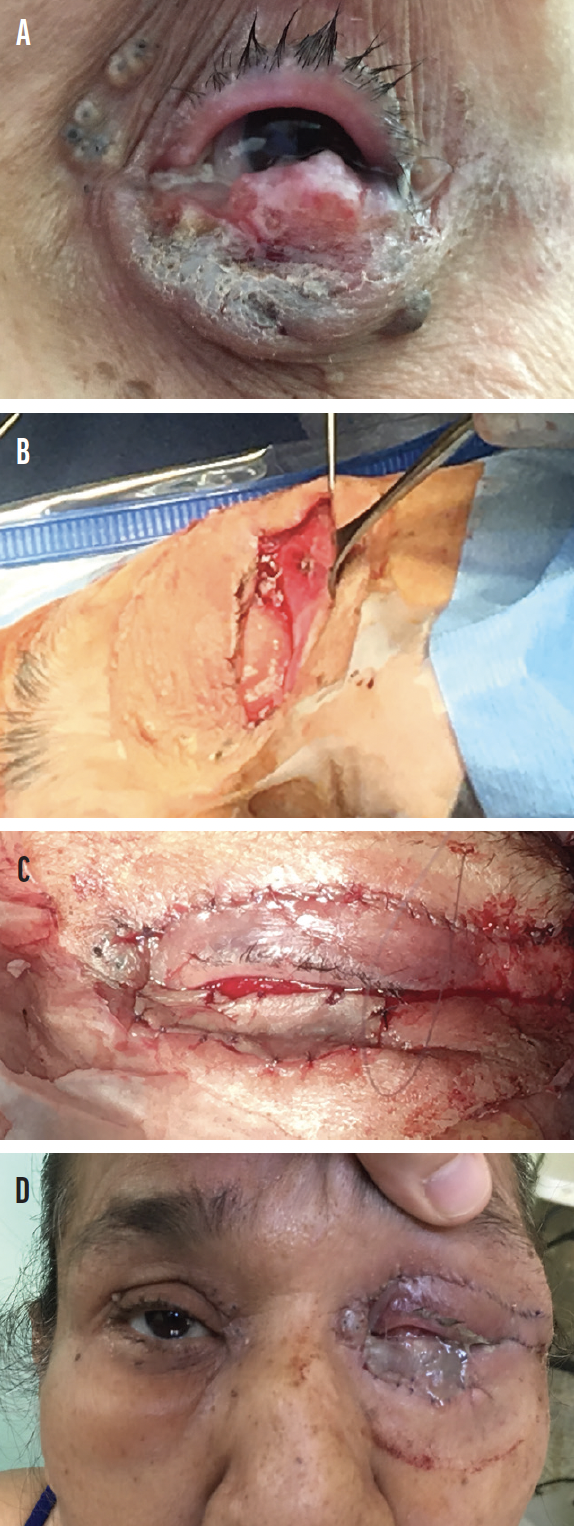
Figure 5. Multiple flaps and a large skin graft from the upper lid were used to reconstruct a 120% width eyelid and periorbital surgical defect after wide excision of a large sebaceous carcinoma (A). Hughes tarsoconjunctival, Tenzel myocutaneous, and lateral orbital rim periosteal flaps were used, and a full-thickness skin graft was placed over the Hughes flap (B, C). The eye at the end of the case (D).
One simple alternative product I began using during oculoplastic surgical teaching projects in Asia is the sterile foam insert that comes inside many ophthalmic suture packets of common materials such as silk, nylon, and polypropylene. These inserts can be cut and trimmed to provide sutured bolsters over antibiotic ointment and Telfa dressing (Covidien), apply pressure over a full-thickness skin graft, and prevent bleeding and hematoma formation under the graft. Cotton dental rolls have been used as bolsters for years. In my experience, however, the sterile foam insert material is much less likely to adhere to the graft when it is removed or harbor infectious organisms during the early postoperative period.
My use of some alternative devices during lacrimal surgery has been due to a lack of surgical tools or products during mission projects. For example, I was frustrated on several missions when I was not able to offer dacryocystorhinostomy and conjunctivodacryocystorhinostomy with Jones tube surgeries because of a lack of surgical air-powered or electric bone drills at many mission sites in developing countries. I therefore took a new, small-profile, battery-powered shop drill on several mission trips. A sterilized 5-mm bone burr is inserted into the drill chuck. The nasal and anterior lacrimal crest bone are then carefully thinned with the sterile drill bit (Figure 6). I then change gloves again and complete the surgery. This method has also been used by orthopedic surgeons in mission settings and developing countries.5
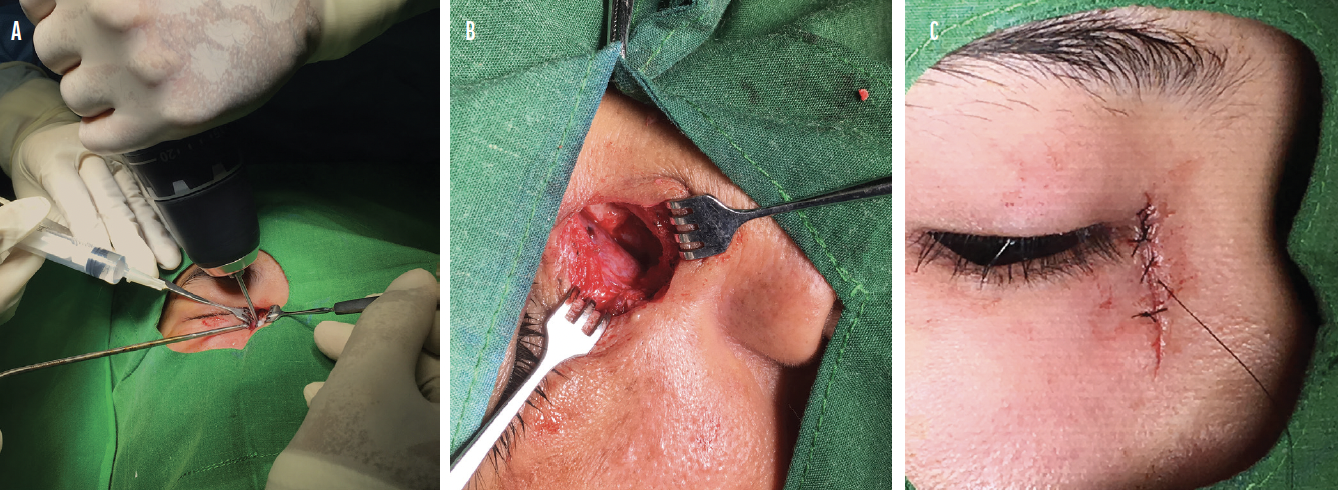
Figure 6. A portable low-speed, battery-powered shop drill can be substituted for a high-speed air-driven or electric surgical drill (A). This can allow dacryocystorhinostomy and conjunctivodacryocystorhinostomy surgeries to be performed in mission settings (B, C).
CONCLUSION
This article describes a few examples of the many alternative surgical devices and techniques that we have employed in medical missions to safely complete surgery when a more creative approach became essential. This creativity has spilled over into my daily practice, providing alternative, fresh approaches to challenging clinical problems.
1. Chang DF. Guidelines issued on short-cycle steam sterilization. Ophthalmology. Published online March 27, 2018.
2. Chang DF, Hurley N, Mamalis N, Whitman J. Evaluation of ophthalmic surgical instrument sterility using short-cycle sterilization for sequential same-day use. Ophthalmology. 2018;125;9:1320-1324.
3. Ponce de León-R S, Bearman G. Guide to infection control in the healthcare setting. Reuse of disposable devices. International Society for Infectious Diseases. February 2018. Accessed September 14, 2021. https://isid.org/guide/infectionprevention/disposabledevices/
4. Mansur JM. Reuse of single-use devices: understanding risks and strategies for decision-making for health care organizations. Joint Commission International 2017. Accessed September 14, 2021. https://www.jointcommissioninternational.org/assets/3/7/JCI_White_Paper_Reuse_of_Single_Use_Devices2.pdf
5. Satish BRJ, Shahdi M, Ramarao D, Ranganadham AV, Kalamegam S. Use of hardware battery drill in orthopedic surgery. Arch Bone Jt Surg. 2017;5(2):114-116.


