



Since its emergence in China in December 2019, SARS-CoV-2 has spread across the world, and COVID-19 was declared apandemic in March 2020.1 The virus is highly contagious andmanifests itself in various organsystems, which can result insubsequent healthcomplications.2
The most prevalent of the ocular manifestations of COVID-19 is viral conjunctivitis,3,4 but the following have also been reported: keratoconjunctivitis, episcleritis, posterior ischemic optic neuropathy, retinal vascular occlusions, polyneuritis, and oculomotor nerve palsy.5 In experimental animal models of SARS-CoV-2 infection, anterior uveitis, retinitis, optic neuritis, retinal vasculitis, blood-retina barrier breakdown, and retinal degeneration have been described.6-10
To date, little information is available on anterior uveitis related to COVID-19. A few case reports have been published on both unilateral and bilateral acute anterior uveitis, occurring mostly as part of a multiinflammatory syndrome associated with COVID-19 in children and young adults,11-16 as well as ocular neuritis or neuroretinitis associated with panuveitis.17-19
This article describes what, to the best of our knowledge, is the largest reported case series of acute bilateral anterior nongranulomatous uveitis and the first reported case of acute bilateral conjunctivitis related to COVID-19 that manifested with severe corneal erosions. All of these individuals were seen in the cornea-uveitis department of the Malayan Eye Center in Yerevan, Armenia, since the start of the pandemic.
UVEITIS RELATED TO COVID-19
Study methodology . We have seen 12 cases of anterior acute bilateral nongranulomatous uveitis related to COVID-19 in our clinic. All of these patients presented between May 2020 and May 2021. We reviewed their files to better characterize the clinical features of this form of uveitis.
One of the patients was male, and 11 were female. Their mean age was 42 years (range, 26–68 years). All of the patients had a history of COVID-19 that was severe at presentation and proven by polymerase chain reaction. None of them had a history of other systemic disorders. All were hospitalized for pneumonia.
Results. Each patient developed ocular symptoms after recovering from COVID-19. On average, 39 days (range, 21–65 days) elapsed between the first manifestations of COVID-19 and the first ocular symptoms. No patient had an ocular history that was remarkable for an episode of uveitis or other ocular inflammatory diseases.
In all cases, the presentation was bilateral but asymmetric. The main ocular manifestations were redness, eye pain, photophobia, blurred vision, and foreign body sensation. BCVA was 20/20 OU in eight patients and 20/40 or better in four patients. IOP and corneal sensation were within normal limits.
Anterior chamber reaction ranged from rare cells to 2+ cells. Interestingly, in all patients, anterior chamber reaction was accompanied by pigmented cells and flare that resembled a pigment storm in the anterior chamber. Fine pigmented keratic precipitates and pigment dusting on the corneal endothelium were also identified (Figure 1). Mydriasis with sectoral iris atrophy, specific for ischemic vasculitis in viral uveitis, was detected in two patients, one of whom exhibited these symptoms bilaterally (Figure 2).
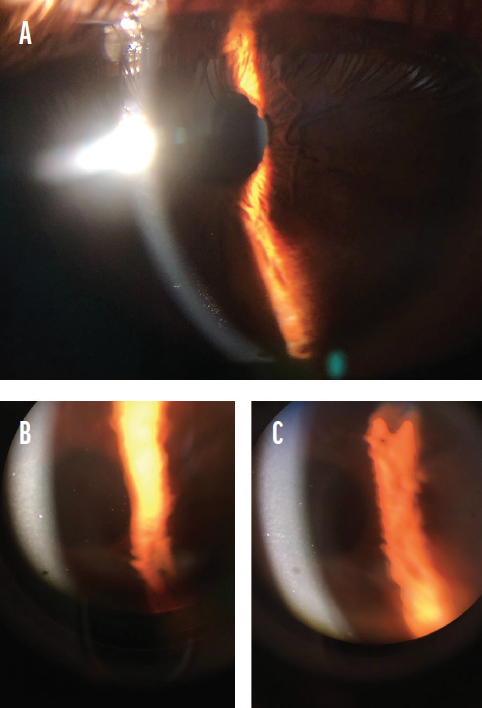
Figure 1. The appearance of fine pigmented keratic precipitates and pigment dusting on the corneal endothelium (A–C).
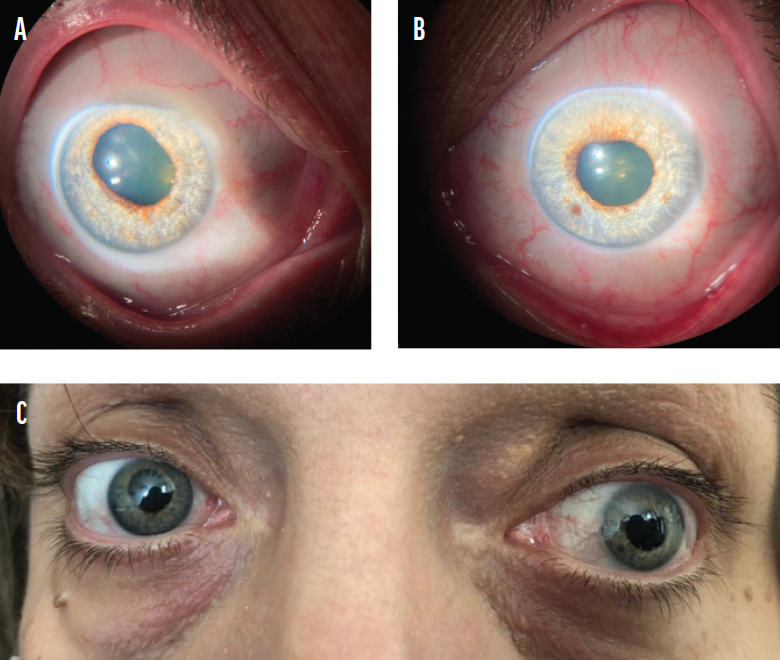
Figure 2. The biomicroscopic appearance of mydriasis in the right (A) and left (B) eyes of a patient with uveitis related to COVID-19. The bilateral presentation of mydriasis in the same patient (C).
Medical therapy for all of the patients consisted of topical corticosteroids and cycloplegic agents. Each individual achieved a good outcome with complete resolution of symptoms and signs. BCVA was 20/20 OU after 3 to 4 weeks of treatment in all patients, and signs and symptoms have not recurred to date.
ACUTE BILATERAL CONJUNCTIVITIS WITH SEVERE CORNEAL EROSIONS RELATED TO COVID-19
In March 2021, a 30-year-old woman presented to our center with a 1-day history of redness, watery discharge, severe photophobia, and pain in both eyes. She stated that 1 week earlier, she had developed nasal congestion, cough, and rhinorrhea and had tested positive for COVID-19.
The history, however, dated back further. The patient had been examined by an ophthalmologist in another clinic for mild symptoms of eye irritation 12 days before presentation to our clinic, and diffuse epitheliopathy had been diagnosed at that earlier visit. Three to four days later, the patient had developed bilateral conjunctivitis with mucopurulent discharge and received a prescription for an antiseptic solution. She started to develop nasal congestion, cough, and rhinorrhea and tested positive for COVID-19. Seven days later, the discharge had ceased, but she developed a sudden onset of photophobia, eye pain, swollen eyelids, and watery discharge and was referred to our clinic.
Upon examination, her BCVA was 20/500 OU. A slit-lamp examination revealed conjunctival injection, follicles, and central corneal epithelial erosions in each eye (Figure 3). The posterior segment examination was unremarkable.

Figure 3. The right eye of a patient with severe corneal erosions. The left eye had a similar appearance, but photography was impossible because of her severe photophobia.
Viral conjunctivitis related to COVID-19 and associated with corneal erosions was diagnosed. Treatment was initiated, including oral doxycycline 100 mg twice daily, topical fluorometholone three times daily, topical cycloplegic agents, and artificial tears.
One day after treatment was initiated, her BCVA improved to 20/100, and the erosions started to heal. At a follow-up examination conducted 7 days after the patient first presented to our clinic, the erosions had healed (Figure 4). The symptoms and signs of both the conjunctivitis and erosions—the tearing, foreign body sensation, photophobia, redness, and discomfort—had resolved completely. Her BCVA was 20/20.
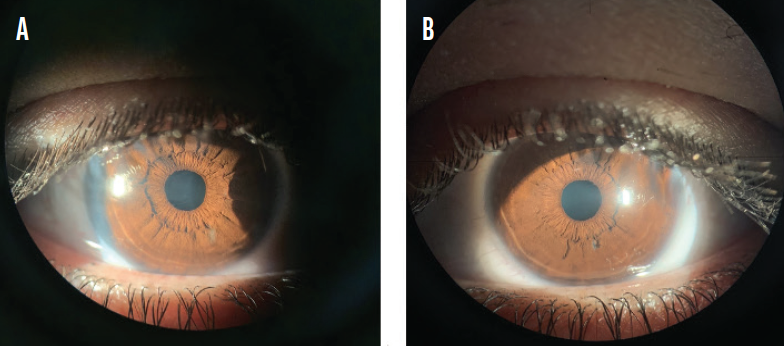
Figure 4. The biomicroscopic appearance of healed erosions in the right (A) and left (B) eyes of the patient shown in Figure 3.
DISCUSSION
Over the course of 1 year, 144 cases of uveitis were referred to our clinic, and 12 of these were related to COVID-19—a prevalence of 8.33%. In the one patient with uveitis related to COVID-19 who developed bilateral iris atrophy mimicking herpetic uveitis, polymerase chain reaction was negative for the herpetic family of viruses, and she was immunocompetent. It is important to note that, in all instances, the onset of uveitis was after the individual had recovered from SARS-CoV-2 infection and that all of the patients responded well to antiinflammatory treatment.
During this period, eight cases of conjunctivitis related to COVID-19 (Figure 5) have been referred to our center, but only one of these was complicated by the development of severe corneal erosions.
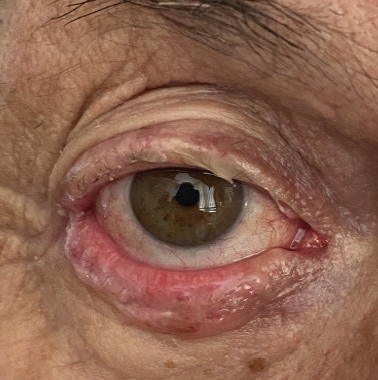
Figure 5. The eye of a patient with conjunctivitis related to COVID-19.
Thirty-two cases of corneal erosions were referred to our center. Of these, 31 were recurrent corneal erosion syndrome (mostly in patients with a history of previous trauma). We had only one case of bilateral corneal erosions, which were associated with conjunctivitis related to COVID-19. This was one of the eight patients with conjunctivitis related to COVID-19.
The takeaways from our experience are as follows. First, anterior uveitis associated with SARS-CoV-2 is not uncommon. This form of uveitis has responded well to topical steroids and cycloplegics and has lasted 4 to 5 weeks. Second, corneal erosions associated with SARS-CoV-2 have responded well to general treatment options, and total recovery has been achieved.
1. Cascella M, Rajnik M, Aleem A, Dulebohn S. Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls. Updated July 18, 2021. https://www.statpearls.com/ArticleLibrary/viewarticle/52171
2. Johnson KD, Harris C, Cain JK, Hummer C, Goyal H, Perisetti A. Pulmonary and extra-pulmonary clinical manifestations of COVID-19. Front Med (Lausanne). 2020;7:526.
3. Nasiri N, Sharifi H, Bazrafshan A, et al. Ocular manifestations of COVID-19: a systematic review and meta-analysis. J Ophthalmic Vis Res. 2021;16(1):103-112.
4. Chen L, Liu M, Zhang Z, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. Br J Ophthalmol. 2020;104(6):748-751.
5. Cheema M, Aghazadeh H, Nazarali S, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can J Ophthalmol. 2020;55(4):e125-e129.
6. Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28(3):391-395.
7. Vinores SA, Wang Y, Vinores MA, et al. Blood-retinal barrier breakdown in experimental coronavirus retinopathy: association with viral antigen, inflammation, and VEGF in sensitive and resistant strains. J Neuroimmunol. 2001;119(2):175-182.
8. Detrick B, Lee MT, Chin MS, Hooper LC, Chan CC, Hooks JJ. Experimental coronavirus retinopathy (ECOR): retinal degeneration susceptible mice have an augmented interferon and chemokine (CXCL9, CXCL10) response early after virus infection. J Neuroimmunol. 2008;193(1-2):28–37.
9. Hooks JJ, Wang Y, Detrick B. The critical role of IFN-gamma in experimental coronavirus retinopathy. Invest Ophthalmol Vis Sci. 2003;44(8):3402-3408.
10. Chin MS, Hooper LC, Hooks JJ, Detrick B. Identification of α-fodrin as an autoantigen in experimental coronavirus retinopathy (ECOR). J Neuroimmunol. 2014;272(1-2):42-50.
11. Wong Chung JERE, Engin Ö, Wolfs TFW, Renson TJC, de Boer JH. Anterior uveitis in paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. Lancet. 2021;397(10281):e10.
12. Bettach E, Zadok D, Weill Y, Brosh K, Hanhart J. Bilateral anterior uveitis as a part of a multisystem inflammatory syndrome secondary to COVID-19 infection. J Med Virol. 2021;93(1):139-140.
13. Karthika IK, Gulla KM, John J, et al. COVID-19 related multi-inflammatory syndrome presenting with uveitis – a case report. Indian J Ophthalmol. 2021;69(5):1319-1321.
14. Alonso RS, Alonso FOM, Fernandes BF, Ecard VO, Ventura MP. COVID-19-related ocular hypertension secondary to anterior uveitis as part of a multisystemic inflammatory syndrome. J Glaucoma. 2021;30(5):e256-e258.
15. Mazzotta C, Giancipoli E. Anterior acute uveitis report in a SARS-CoV-2 patient managed with adjunctive topical antiseptic prophylaxis preventing 2019-nCoV spread through the ocular surface route. Int Med Case Rep J. 2020;13:513-520.
16. Öztürk C, Yüce Sezen A, Savaş Şen Z, Özdem S. Bilateral acute anterior uveitis and corneal punctate epitheliopathy in children diagnosed with multisystem inflammatory syndrome secondary to COVID-19. Ocul Immunol Inflamm. Published online April 15, 2021. doi:10.1080/09273948.2021.1909070
17. François J, Collery AS, Hayek G, et al. Coronavirus disease 2019-associated ocular neuropathy with panuveitis: a case report. JAMA Ophthalmol. 2021;139(2):247-249.
18. Hosseini SM, Abrishami M, Zamani G, et al. Acute bilateral neuroretinitis and panuveitis in a patient with coronavirus disease 2019: a case report. Ocul Immunol Inflamm. Published online April 8, 2021. doi:10.1080/09273948.2021.1894457
19. Benito-Pascual B, Gegúndez JA, Díaz-Valle D, et al. Panuveitis and optic neuritis as a possible initial presentation of the novel coronavirus disease 2019 (COVID-19). Ocul Immunol Inflamm. 2020;28(6):922-925.


