
Posterior capsulorhexis (PCR) with posterior optic buttonholing (POBH) is a technique that combines standard surgical and implant skills with the aim of eradicating posterior capsular opacification (PCO). The technique comprises standard PCR, peripheral viscoseparation of the posterior capsule and anterior vitreous hyaloid, and entrapment of the IOL optic into the PCR opening. Any standard three-piece or one-piece IOL with a slim haptic-optic junction can be used in this technique.
PCR with POBH has been thoroughly investigated and described in the literature.1-9 This article recaps the important steps of the technique and imparts pearls for performing it safely and effectively.
POSTERIOR CAPSULORHEXIS
PCR is preferably performed under topical anesthesia, which provides globe stability and allows pupillary retroillumination. After cataract removal and careful cleaning of residual lens fibers from the capsular bag, a diaphragm made up of the anterior and posterior capsules is created. The aqueous is gently expelled by injecting OVD through the main incision without expanding the capsular bag. Instead, the anterior capsule leaf is settled onto the posterior capsule, and both are flattened out.
A central posterior capsular incision and a centered PCR 4 to 5 mm in diameter are then created (Figures 1-4). To execute the PCR, a 27-gauge hypodermic needle is bent bevel up, inserted through a paracentesis, and used to incise the posterior capsule. Then OVD is slowly injected at the level of this incision to inflate the Berger space and separate the anterior hyaloid from the posterior capsule.
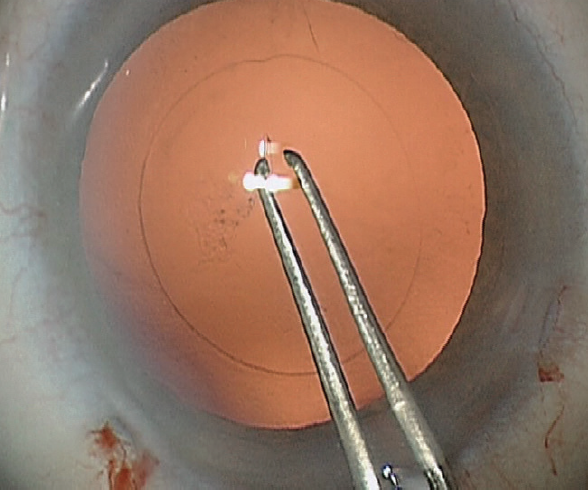
Figure 1. After lens removal and posterior capsular polishing are complete, a central posterior capsular incision is made with a needle, and a PCR is begun with forceps.
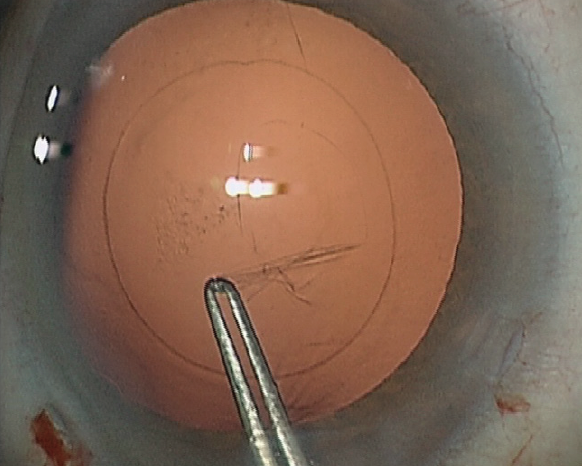
Figure 2. The centered PCR is made 0.5 mm smaller than the anterior capsulorhexis, with the latter used as a ruler.
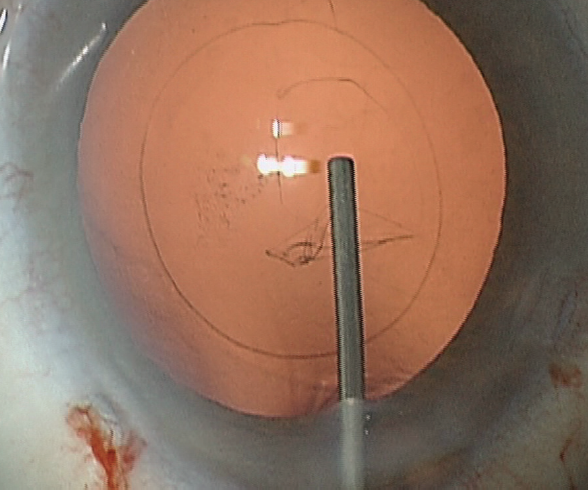
Figure 3. To inflate the Berger space and separate the anterior vitreous hyaloid from the posterior capsule, OVD is slowly injected at the level of the PCR.
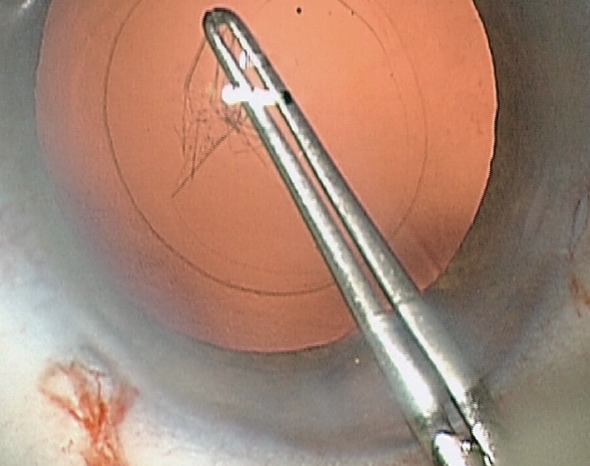
Figure 4. The PCR is completed.
While the OVD is injected, the posterior capsule is kept flat by placing the orifice of the cannula above or beneath the capsular incision as required. The edge of the incised capsule is then grasped with forceps, and a PCR 0.5 mm smaller than the anterior capsulorhexis is created, with the latter used as a ruler. If the posterior capsule turns out to be flaccid, a capsular tension ring may be inserted before or at any time during the procedure.
The peripheral posterior capsule and anterior hyaloid are then circumferentially separated by inserting the cannula through the sideport incisions and gently injecting an OVD beneath the posterior capsule (Figure 5). Progress of the vitreocapsular separation can be seen as a dissection line that moves peripherally.
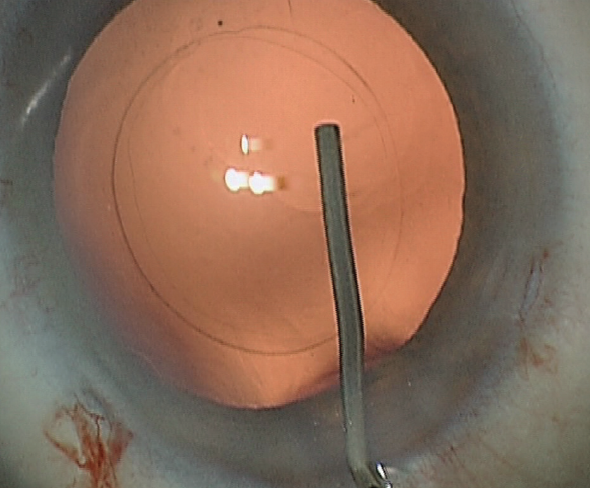
Figure 5. The peripheral posterior capsule and anterior hyaloid are separated by gently injecting OVD beneath the posterior capsule.
IOL INSERTION AND ENTRAPMENT
A pocket in the collapsed capsular ring is created nasally for placement of the leading IOL loop. To do this, the tip of the OVD cannula is maneuvered into the collapsed capsular fornix to gently separate the two capsular leaves. A looped three-piece or one-piece IOL with a slim haptic-optic junction is injected, and the leading loop is directed into the prepared capsular pocket. After the lens unfolds, a phaco spatula is positioned above the optic to control IOL vaulting while a Y-spatula, inserted through the main incision, is used to compress and rotate the trailing haptic into the capsular fornix (Figures 6 and 7).
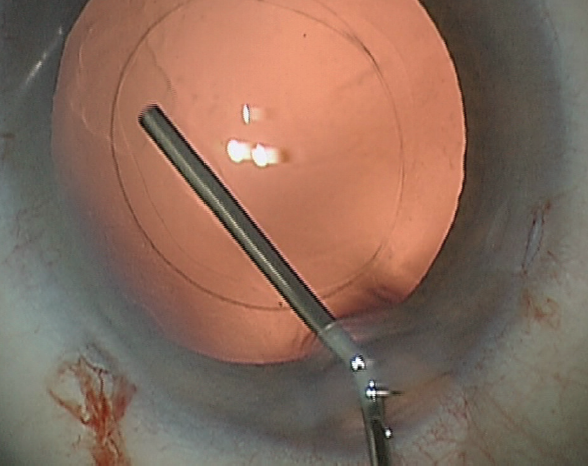
Figure 6. Progress of vitreocapsular separation can be seen as a dissection line that moves peripherally.
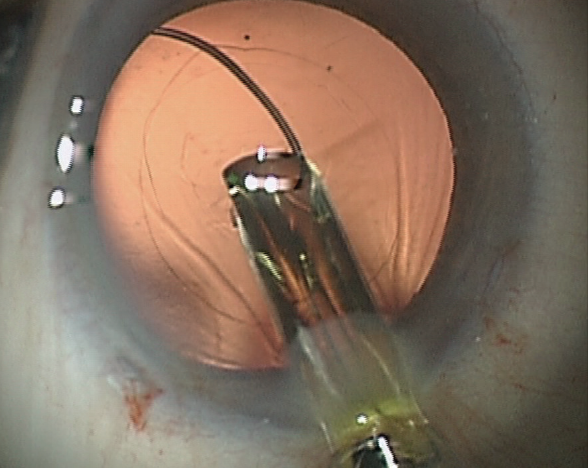
Figure 7. An IOL with a slim haptic-optic junction is injected, and the leading loop is directed into the prepared capsular pocket.
With both loops placed in the bag fornix, the optic is then buttoned into the PCR opening with gentle pushing on the optic’s midperiphery, left and right of the IOL axis, thus tilting the optic slightly and allowing it to slip under the posterior capsule (Figures 8 and 9).
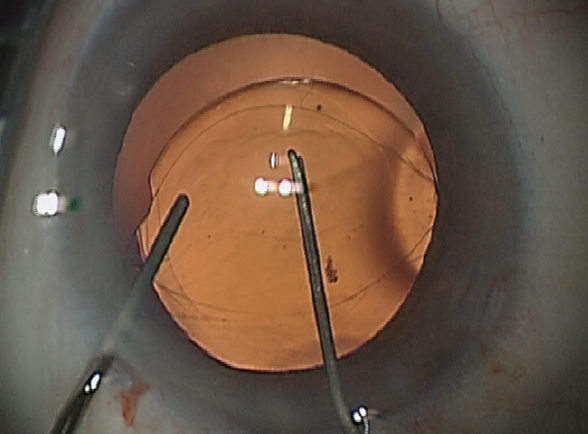
Figure 8. With both loops placed in the bag fornix, the optic is then buttoned into the PCR opening by gently pushing on the optic’s midperiphery, left and right of the IOL axis.
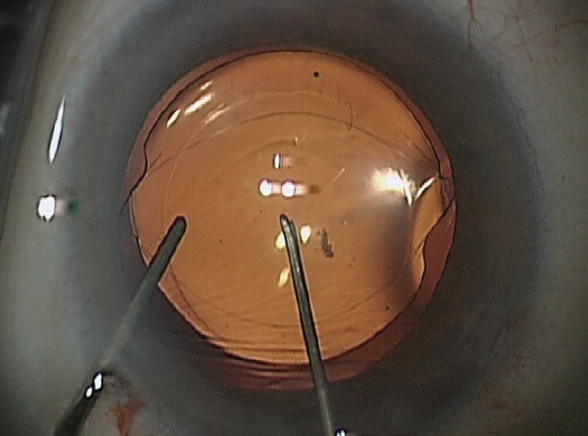
Figure 9. This action tilts the optic slightly and allows it to slip under the posterior capsule.
Once the lens is positioned, the paracenteses are hydrated before the OVD is aspirated with a sleeved coaxial I/A probe. The probe is abruptly retracted to allow the main incision to shut down immediately. These steps are taken to avoid chamber flattening due to bulging of the capsule-lens diaphragm and possible deenclavation of the optic.
ADVANTAGES
In my experience, a major advantage of PCR with POBH over standard in-the-bag IOL implantation is the complete eradication of PCO, eliminating the need for Nd:YAG laser capsulotomy. PCO and Nd:YAG capsulotomy rates are largely underestimated and have increased in recent years as one-piece and hydrophilic IOLs have replaced silicone and hydrophobic acrylic three-piece IOLs with truly sharp edges. In addition, some modern hydrophobic acrylic IOLs have rounder edges than those of 10 years ago. Laser capsulotomy can also cause complications such as floaters, retinal detachment, glaucoma, and uveitis. Even more important, elderly patients do not regularly consult their ophthalmologists after cataract surgery, and these patients typically show up only when the second eye has also developed significant PCO. In addition, Nd:YAG laser capsulotomy requires costly equipment and is not readily available in developing countries.
The principal advantage of adding POBH to PCR is that the posterior optic entrapment prevents secondary closure of the PCR opening by lens epithelial cells (LECs). In the absence of the central posterior capsule, without POBH, LECs may still overrun the PCR edge and migrate centrally, using the anterior hyaloid or posterior optic surface as an alternative scaffold. I have found that this migration can lead to partial or even total secondary closure of the PCR opening and require Nd:YAG laser treatment. With POBH, the posterior capsular edge is wrapped over and thus lies on top of the IOL optic (Figure 10). Migrating equatorial LECs are diverted into the anterior chamber and cannot access the retro-optic space.
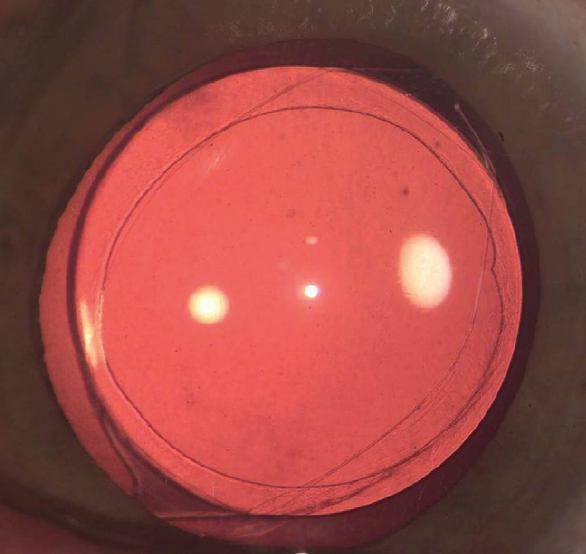
Figure 10. The posterior capsular edge is wrapped over and thus lies on top of the IOL optic. Migrating equatorial LECs are diverted into the anterior chamber and cannot access the retro-optic space. Reprinted with permission from Menapace.2,7
In addition to eradicating PCO, POBH also greatly reduces anterior capsular opacification (ACO). Sandwiching the posterior capsular leaf between the anterior capsular leaf and the IOL optic inhibits anterior LECs from touching the optic surface. Such contact is the prerequisite for myofibroblastic transdifferentiation of anterior LECs, which leads to fibrotic whitening and shrinkage of the anterior capsule. Fibrosis, therefore, remains inherently limited to the small areas where the PCR edge crosses over the haptic-optic junction (Figure 11). Another advantage of POBH is the absence of postoperative refractive shift; entrapment of the optic prevents its axial movement.1
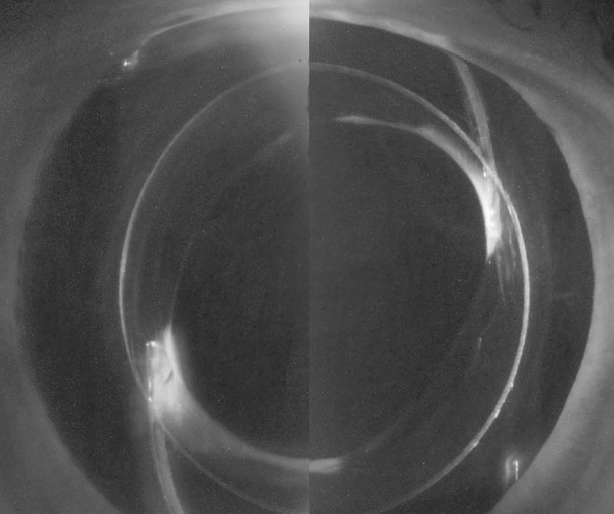
Figure 11. Fibrosis is inherently limited to the small areas where the PCR edge crosses over the haptic-optic junction. Reprinted with permission from Menapace.2,7
PCR with POBH also has advantages over the bag-in-the-lens technique. Although bag-in-the-lens is an exquisitely elegant technique that also eradicates both PCO and ACO, it has certain downsides. First, bag-in-the-lens requires a special IOL implant with grooves along the optic rim to accommodate the capsulorhexis edges. POBH works with any standard IOL that has a slim optic-haptic junction. POBH thus also allows the use of smaller incisions than those required for the bulkier Bag-In-The-Lens (Morcher) IOL. Second, for bag-in-the-lens, both the anterior and posterior capsulorhexis openings must be perfectly round, 5 mm in diameter, and concentric to allow stable fixation of the implant. Inadequacies in these regards may render bag-in-the-lens fixation unsafe or even impossible. In contrast, POBH is very forgiving. Because the haptics reside in the capsular bag fornix, the IOL will center even within a decentered or incongruent PCR. Also, should the surgeon encounter difficulties during PCR with POBH, he or she can fixate the IOL alternatively, whether in the bag with optional anterior entrapment or in the sulcus with optional posterior entrapment in the anterior capsulorhexis opening.
EVIDENCE OF SAFETY
For the dedicated and skilled surgeon, the learning curve for PCR with POBH is short.2 All steps are fully controllable with no black boxes. Vis a tergo has never been an issue because hydrostatic pressure during phacoemulsification and cortical aspiration provides internal oculopression. Anterior hyaloid laceration or vitreous prolapse can be avoided with proper surgical technique; in the rare cases when either occurs, it has never led to retinal or macular complications in my experience. In my first 1,000 consecutive cases with follow-up of 4 to 6 years, only two cases (0.2%) of retinal detachment were reported.
We have conducted a series of prospective randomized studies comparing the safety profile of POBH to standard in-the-bag implantation and to PCR alone. With POBH, IOL and capsule form a tight mechanical diaphragm that keeps the OVD behind it from prolapsing or dissipating anteriorly. Anterior chamber flare, as measured with a lens-flare meter on postoperative day 1, was even lower than after standard in-the-bag IOL implantation and was identical thereafter.3 IOP without medication in the immediate postoperative period was also identical.4 Unlike with PCR alone, PCR with POBH did not cause postoperative pressure spikes.5
Macular thickness and volume, as well as macular micromorphology as imaged and measured by high-resolution OCT, were identical to those after standard in-the-bag IOL implantation.6 The rate of clinically significant cystoid macular edema was not observed or reported to be higher after PCR with POBH than with standard IOL implantation. Hypothetically, the OVD cushion trapped behind the IOL-capsule diaphragm may act as a diffusion barrier that, during the early postoperative days, may block the diffusion of cytokines from the anterior to the posterior segment and macula.
CONCLUSION
The rationale, technique, and results of the first 1,000 consecutive cases of PCR with POBH have been published in detail in the peer-reviewed literature.7 PCR with POBH is a safe and effective surgical approach that completely and permanently eradicates PCO and significantly reduces ACO. The technique does not require special instrumentation or a special IOL, and it can easily be converted to standard IOL fixation should the surgeon deem it necessary.
1. Stifter E, Menapace R, Luksch A, et al. Anterior chamber depth and change of axial intraocular lens position after cataract surgery with primary posterior capsulorhexis and posterior optic buttonholing. J Cataract Refract Surg. 2008;34:749-754.
2. Menapace R. Routine posterior optic buttonholing for eradication of posterior capsule opacification in adults: report of 500 consecutive cases. J Cataract Refract Surg. 2006;32:929-943.
3. Stifter E, Menapace R, Luksch A, et al. Objective assessment of intraocular flare after cataract surgery with combined primary posterior capsulorhexis and posterior optic buttonholing in adults. Br J Ophthalmol. 2007;91:1481-1484.
4. Stifter E, Luksch A, Menapace R. Postoperative course of intraocular pressure after cataract surgery with combined primary posterior capsulorhexis and posterior optic buttonholing. J Cataract Refract Surg. 2007;33:1585-1590.
5. Stifter E, Menapace R, Kriechbaum K, Luksch A. Posterior optic buttonholing prevents pressure peaks after cataract surgery with primary posterior capsulorhexis. Graefes Arch Clin Exp Ophthalmol. 2010;248(11):1595-1600.
6. Stifter E, Luksch A, Menapace R. Macular morphology and central retinal thickness after cataract surgery with primary posterior capsulorhexis and posterior optic buttonholing. Am J Ophthalmol. 2008;146:15-22.
7. Menapace R. Posterior capsulorhexis combined with optic buttonholing: an alternative to standard in-the-bag implantation of sharp-edged intraocular lenses? A critical analysis of 1000 consecutive cases. Graefes Arch Clin Exp Ophthalmol. 2008;246(6):787-801.


