Preoperative care is becoming increasingly important to cataract surgery outcomes. Just as diagnosis and treatment of dry eye disease are now understood to be essential due to its impact on visual outcomes, it is also necessary to look for retinal pathology that may affect vision or influence cataract treatment decisions.
To do this, I perform ultrawide-field (UWF) retinal imaging with the optomap (Optos) preoperatively on every cataract patient. For the past 7 years, I have found this to be an invaluable diagnostic tool in my practice. In addition to enhancing clinical examinations, integrating UWF imaging has simplified my examination protocol by replacing more cumbersome and time-intensive diagnostic tests. The device is easy for technicians to use and comfortable for the patient. Image capture takes less than a second.
UNCOVERING PATHOLOGY
Although a dilated fundus examination is a valuable standard of care, technology has advanced, and we now have the opportunity to offer patients a much more thorough assessment. A standard fundus photograph provides a view of 15% of the retina. By contrast, a single UWF image is able to capture up to 82% of the retina, including structures beyond the vortex and the ampullae (equator). Imaging through a 3+ cataract is possible in the vast majority of patients.1
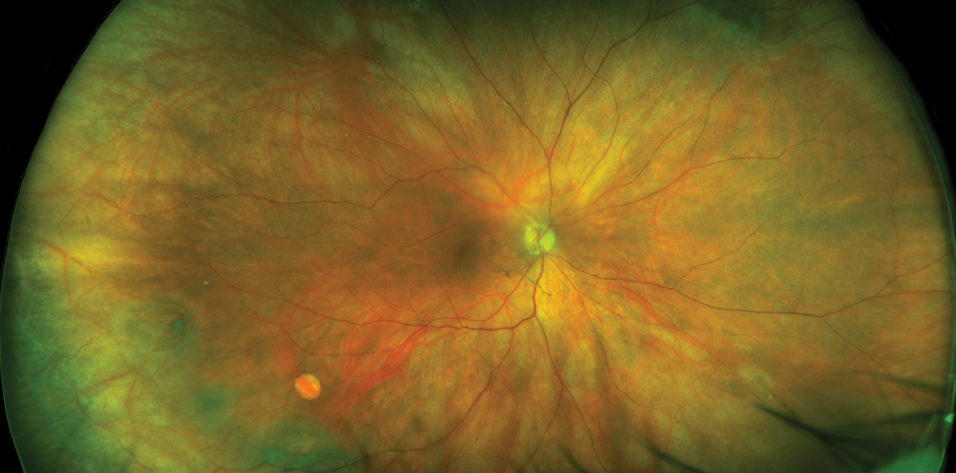
As UWF imaging becomes more widespread, we are beginning to understand the value of imaging the periphery. A review of 32 studies including 3,602 eyes found that an average of 66.43% of retinal findings fall outside of 60º from the optic nerve head.2 In a direct comparison with fundus photography, UWF imaging with optomap reduced the number of ungradable images by 81%, increased identification of diabetic retinopathy by nearly twofold, and revealed peripheral lesions that resulted in a more severe diagnosis of diabetic retinopathy in almost 10% of patients.3 In a comparison of ETDRS seven standard field imaging to UWF fluorescein angiography in 106 patients, retinal vascular pathology that was not identified on standard imaging was identified with UWF imaging in 43.4% of eyes (Figure 1).4

Figure 1. Optomap UWF image of severe nonproliferative diabetic retinopathy with peripheral hemorrhages, with overlay of seven standard fields ETDRS images as comparison.
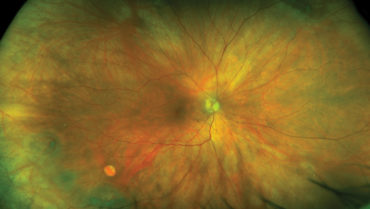
(All images courtesy of Netan Choudhry, MD)
In addition, analysis of UWF imaging has shown that the mean area of perfused retina in a healthy eye is 977.0 mm2, a point of data that may provide a useful reference for assessing the pathologic significance of abnormal findings.5
With the increasing prevalence of diabetes, a thorough retinal examination before cataract surgery provides a valuable opportunity to check for diabetic eye disease. Early changes can have major implications; peripheral signs of diabetic retinopathy appear much sooner than central signs and are associated with heightened risk of progression.6 The RISE and RIDE studies in patients with diabetic macular edema demonstrated greater improvements in vision in eyes treated with an anti-VEGF agent within the first 2 years of diagnosis, compared with eyes with chronic diabetic macular edema associated with irreversible damage.7
Nonmydriatic UWF imaging has been shown to compare favorably with dilated ETDRS photography. Undilated UWF imaging had high sensitivity (99%) and specificity (100%) and agreed within 1 level of severity with ETDRS photographs in 91% of eyes.8 In short, it is equally as effective as photography for finding pathology as well as faster and easier to use (Figure 2).

Figure 2. Optomap UWF image of a retinal hole with a horseshoe tear in the periphery.
IMPACT ON CATARACT SURGERY
The scanning laser ophthalmoscopy technology used to create the optomap can capture images effectively through small pupils and challenging media, including cataracts. With traditional white-light fundus imaging, the light scatters when it hits retinal opacities such as asteroid hyalosis, making the retina difficult to see. The quick, consecutive images that can be obtained with scanning laser ophthalmoscopy technology enable capture of a floater in different locations. Complaints of flashers and floaters should be investigated, as they can be associated with holes, tears, or traction or adhesions across the retina.
Fortunately, detection of preexisting retinal conditions is relatively infrequent, and, once pathology is ruled out, we can proceed to cataract surgery with greater confidence. When pathology is found, we can treat or refer patients who may benefit from presurgical treatment. Alternatively, we can proceed to surgery knowing of any surgical modifications needed or changes to IOL selection to be made to avoid worsening the patient’s condition.
Modern cataract patients have high expectations for optimal outcomes of surgery, and progressive surgical techniques and lens technologies enable us to consistently deliver what our patients expect. This use of up-to-date technology should extend beyond the OR; it is absolutely essential to perform a thorough preoperative examination to prevent any surprises. Pathology that is revealed only after cataract surgery is alarming to patients and often leads to low patient satisfaction.
PATIENT ENGAGEMENT
Not only is UWF imaging thorough, but it also provides an excellent visual aid for patient education and helps me to engage patients in their care and to manage surgical expectations. When I show patients the pathology in their own retinal images, such as spots of dry age-related macular degeneration, and I explain that we must take precautions to keep the rest of the retina healthy, they tend to be more compliant with treatment and understanding of surgical delays, when necessary.
With UWF imaging, I can avoid overlooking retinal pathology that may potentially interfere with postoperative results. The optomap is an excellent tool to establish a baseline and monitor disease progression in my patients, whether they see me for cataract removal or other pathology. When I document the retinal status before surgery, I can show it to the patient; this way, the patient knows the existing pathology was not caused by cataract surgery.
OFFICE EFFICIENCY
My Optos device is a workhorse. I have imaged thousands of patients, and my experience tells me that I can rely on and trust the information it gives me. Even though I find pathology in only a small percentage of patients, it is worth the investment, particularly because my practice extends beyond cataract surgery to diabetes, glaucoma, and other pathologies. Retinal imaging is also easy to perform and interpret in pediatric eyes.
With all of my patients, I use the Optos device during their regular annual or biannual examinations, particularly in the management of diabetic eye disease. Although optomap imaging is primarily a tool to detect posterior segment pathology, it also helps me to monitor developing cataracts. Even if I am hunting for diabetic eye disease, I can detect clouding caused by the early stages of cataract and explain to patients that not all of their visual loss is caused by diabetic retinopathy.
UWF imaging is essential to running my practice. With 50 to 60 patients seen and imaged each day, I recouped the investment in the Optos device in about 1 year. The clear images and extensive data provided on the optomap provide security to me and assist in educating my patients. Patients are better informed, and we can anticipate and monitor developing pathology that would previously have gone undetected until it progressed to the central retina. This allows us to begin intervention at an earlier stage of disease.
I define a good instrument as one that I start using the first day it is delivered and use progressively more and more. For me, the Optos device fits firmly in that category.
1. Chen W, Friberg T, Eller A, Medina C. Advances in retinal imaging of eyes with hazy media: further studies. Paper presented at: ARVO Annual Meeting; May 1-5, 2011; Fort Lauderdale, FL.
2. Kehoe P. Widefield patient care. Poster presented at: The European Academy of Optometry and Optics Annual Meeting; May 19-22, 2016; Berlin, Germany.
3. Silva PS, Horton MB, Clary D, et al. Identification of diabetic retinopathy and ungradable image rate with ultrawide field imaging in a national teleophthalmology program. Ophthalmology. 2016;123(6):1360-1367.
4. Jones NP, Sala-Puigdollera A, Stanga PE. Ultra-widefield fundus fluorescein angiography in the diagnosis and management of retinal vasculitis. Eye (Lond). 2017;31(11):1546-1549.
5. Singer MS, Sagong M, van Hemert J, et al. Ultra-widefield imaging of the peripheral retinal vasculature in normal subjects. Paper presented at: Macula Society Annual Meeting; February 25-28, 2015; Scottsdale, AZ.
6. Silva PS, Dela Cruz AJ, Ledesma MG, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122(5):949-956.
7. Brown DM, Nguyen QD, Marcus DM, et al; RIDE and RISE Research Group. Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase II trials (RISE and RIDE). Ophthalmology. 2013;120(10):2013-2022.
8. Silva PS, Cavallerano JD, Sun JK, et al. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol. 2012;154(3):549-559.e2.