DED is Not a Simple Problem
This multifaceted disease requires careful history-taking, for a start.
By Jose L. Güell, MD, PhD

Any ophthalmologist, whatever his or her subspecialty, will see patients with dry eye disease (DED) in daily practice. Although in most cases the condition will not be severe, the management of these patients can be complicated for the physician and unsatisfactory for the patient.
In fact, DED is not a simple problem but rather a multifaceted condition that can have inflammatory, evaporative, and tear insufficiency components. Perhaps dry eye should be considered as a subspeciality by itself.
THE DIAGNOSTIC EXAM
Below are the steps we take in evaluating patients with DED:
Step No. 1: Thorough patient history. As with any disease, taking a thorough history is extremely important. This should include patients’ previous or current use of contact lenses, details about their work and home environments, the nature of their discomfort, systemic diseases or allergies, medications taken, and any other relevant details.
Step No. 2: Slit-lamp examination. This step in the evaluation should emphasize assessment of the eyelids, first in terms of function and anatomy (eg, adequate eyelid closure), then exploring the eyelid border including the meibomian glands.
Step No. 3: Detecting lesions of the ocular surface. Vital stains can be helpful to detect lesions of the ocular surface secondary to dryness: fluorescein to identify epithelial defects and rose bengal and/or lissamine green to identify areas of necrotic cells.
Step No. 4: Objective testing. The height of the tear meniscus and the presence or absence of signs of conjunctival inflammation can also give insights into the situation, as well as clues to evaluate the etiology and to guide treatment choices. Also, complementary tests can help to guide the diagnosis and choice of therapeutic measures; tear breakup time (TBUT), Schirmer (with or without topical anesthesic), and osmolarity testing are the most widely used.
Additionally, examination with the OQAS HD Analyzer (Visiometrics) is extremely useful to generate functional information about visual quality (optical aberrations and scatter) during the breakup of the tear film. This test can easily and dynamically explain why some dry eye patients report very poor visual quality.
TREATMENT OPTIONS
Once we have gathered all possible information on the patient and his or her ocular surface condition, treatment choices are based on what we have observed in our examinations.
Option No. 1: If no inflammatory component is observed, in most cases the frequent use of a tear substitute (preferably hyaluronic acid-based and preservative-free) is sufficient to relieve symptoms. Reversible punctal occlusion can also be considered, albeit this can have widely varying results.
Option No. 2: If there is an inflammatory component, one should consider the use of topical cyclosporine A 0.05% (Restasis; Allergan) and/or short pulses of topical steroids. In these cases, we have had good results using homeopathic artificial tears as a tear substitute. These drops contain natural antiinflammatory components, including euphrasia and cochlearia officinalis among others.
At a Glance
• Steps of the patient evaluation process for DED include a thorough patient history; slit-lamp examination; detection of lesions on the ocular surface; and objective testing such as height of the tear meniscus, the presence or absence of signs of conjunctival inflammation, TBUT, and Schirmer and osmolarity testing.
• Treatment choices should be based on what was observed in patients’ examinations.
• In the near future, treatment of dry eye patients with the amphiphilic glycoprotein lubricin may help protect the ocular surface with a low number of instillations.
• Use of a lubricant eye drop several times daily is a good first line treatment; in more severe cases, a preservativefree drop containing sodium hyaluronate is a better choice.
• Antiinflammatory treatments have become an important part of DED management.
• MGD must be identified and treated as part of the patient’s ocular surface deficiency.
Option No. 3: In eyes with chronic trophic lesions, one should consider the use of autologous serum eye drops or ground amniotic membrane. We have found that this option can be especially useful.
Option No. 4: In clinical situations in which a systemic cause for the dryness is known, management of the underlying disease can significantly improve the ocular surface condition. Such situations include patients who have diseases that have vasculitis as a symptom (eg, rheumatoid arthritis, lupus erythematosus) or graft-versus-host disease.
Option No. 5: Surgery may be necessary in severe cases. Depending on the case, surgical approaches can include eyelid correction, tarsorrhaphy, amniotic membrane transplantation, and other options.
What is Lubricin?
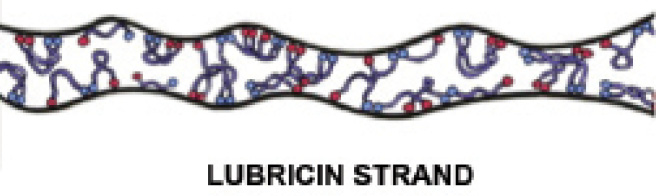
Proteoglycan 4, or lubricin, is the most lubricating and antiadhesive molecule in the human body.1 This large endogenous complex glycoprotein binds to and protects tissue surfaces from friction-induced wear and damage. In addition to the ocular surface, it is also in other tissues throughout the body, including knee cartilage.
The body’s natural ability to produce lubricin becomes impaired in the presence of inflammation caused by injury, disease, or aging. Recently, it has been postulated that supplementation with recombinant lubricin may help to interrupt the inflammatory cascade and restore function to the area in which it is applied.
1. Lubris website. About Lubricin. http://lubris.net/aboutlubricin/. Accessed May 28, 2015.
CONCLUSION
It is important to remember, as mentioned at the outset, that dry eye includes a wide spectrum of clinical situations. In many cases, it may best be managed by a specialist in order to minimize secondary problems on the ocular surface and, thus, visual limitations for the patient.
Optimize Your Comprehensive Dry Eye Treatment Plan
An overview of present and future dry eye treatment strategies.
By Leonardo Mastropasqua, MD; and Mario Nubile, MD
One of the most interesting challenges in ophthalmology at present is optimization of a comprehensive treatment for our dry eye patients. A single therapeutic approach efficient for all types of dry eye is not yet available, mainly because DED is a complex pathology involving several interacting pathophysiologic mechanisms that need specific treatments.
In our cornea and ocular surface center, to which a high volume of dry eye patients are referred from throughout the nation, we have spent significant effort over the past few years optimizing diagnostic procedures for differentiating and staging dry-eye–related clinical manifestations. Increasing scientific evidence suggests that both aqueous-deficient and evaporative DED need customized therapeutic approaches based on the type and severity of their clinical features.
INITIAL TREATMENT
As a first level approach, the majority of patients are treated with artificial tears eye drops. Types and doses of these lubricants are strictly dependent on specific conditions of the ocular surface, tear film dynamics, symptoms, and associated disease. We recommend preservative-free eye drops if frequent instillation (more than four to six times daily) is needed to improve patient comfort and ocular surface features, as well as in contact lens wearers. Large quantities of preservatives, and even low doses distributed over a prolonged period (months or years), can promote significant changes in the delicate network of ocular surface epithelial and goblet cells, affect mucin production, or promote inflammation.
In all patients, comorbidities must be identified and treated either at a local (ie, lid malposition, meibomian gland dysfunction) or systemic (ie, endocrine dysmetabolism, autoimmune disorders) level. Ocular surface inflammation is almost always associated with dry eye, inducing self-maintaining negative effects on the epithelial cells and tear film components. Therefore, we treat inflammation detectable by either clinical or microscopic examinations with local steroid eye drops, using pulsed cycles and tapering the dosage over a 4- to 6-week period. When longer treatments are needed, our preferred choice is cyclosporine.
UNDER INVESTIGATION
One innovative approach we are currently investigating is treating DED patients with lubricants such as recombinant lubricin eye drops. Lubricin is an amphiphilic glycoprotein that is naturally secreted by chondrocytes and synoviocytes, adhering to cartilaginous surfaces and protecting articular cartilage against frictional forces. This superficial zone protein has a molecular structure similar to that of the mucin layer of the tear film and is produced by ocular surface epithelia and meibomian glands. Recent studies in animals1 suggest that the presence of lubricin on the ocular surface may reduce friction between the cornea and conjunctiva and that deficiency of this glycoprotein may play a role in promoting corneal damage. Currently, eye drops containing recombinant lubricin are not available on the market, but it is possible that, in the near future, treatment of our dry eye patients with such molecules may help protect the ocular surface epithelia with a low number of instillations. If this is found to be true, these treatments can be useful to optimize both the clinical effects of DED treatment and patients’ compliance with their regimens.
1. Schmidt TA, Sullivan DA, Knop E, et al. Transcription, translation, and function of lubricin, a boundary lubricant, at the ocular surface. JAMA Ophthalmol. 2013;131(6):766-776.
A Range of Treatment Options for Dry Eye
Therapeutic choices depend on the patient’s clinical situation.
By Pierre-Jean Pisella, MD, PhD

When a patient presents with symptoms of DED, one’s treatment choices vary depending on the clinical stage of the disease. Choices are also affected by whether the DED is related to tear production deficiency, evaporation of the tear film, or both. Fortunately, a wide range of options is available in Europe for the management of patients with DED.
FIRST LINE: LUBRICANTS
For any patient with mild to moderate DED, the use of a lubricant eye drop several times daily is a good first step. A number of products that contain preservatives are available without prescription, but for patients with mild to moderate symptoms I always prescribe a nonpreserved formulation.
Even in this basic first line category of nonpreserved tears, there is a variety of choices. Among the name-brand products are Refresh Optive (Allergan) and Systane Ultra (Alcon). In the French market, probably the most popular nonpreserved drop is Lacrifluid (Laboratoire Europhta), in which the active ingredient is carbomer.
If the patient does not respond well to these first line lubricant drops, the picture becomes a bit more complicated. We might go to a more sophisticated lubricant, a cationic mineral oil emulsion such as Retaine MGD (OcuSoft).
In more severe cases, in which superficial punctate keratitis (SPK) involves more than 5% to 10% of the corneal surface, I step up patients’ treatments to a drop containing sodium hyaluronate—again, preservative-free. One such drop is Artelac Rebalance (Bausch + Lomb), which is available as a preserved product as well as in nonpreserved single-dose units. (Editor’s note: For a more extensive list of eye drops containing sodium hyaluronate, see the sidebar Sodium Hyaluronate Eye Drop Solutions, on page 61.)
It should be noted that high-end nonpreserved drops do not represent a large part of the French artificial tear market, and this is probably true in other European countries as well. This is because patients must pay for these rather expensive treatment options out of pocket, as the drops are not covered by our social health insurance. I recently attended the 2015 Société Française d’Ophtalmologie (SFO) meeting in Paris, and, according to discussions there, it appears that sodium hyaluronate drops account for only about 10% of the artificial tear market (personal communication).
LID HEALTH
In more than 50% of DED cases, meibomian gland dysfunction (MGD) is either a primary or secondary component of the disease. MGD must be identified and treated as part of the patient’s ocular surface deficiency. The patient’s lids should be inspected, and the meibomian glands should be expressed to assess the quality of the meibum.
An important element of care for MGD is patient education regarding proper lid hygiene. This can include warm compresses, lid massage, and lid scrubs to help keep the meibomian glands clean and clear. If the glands are in poor condition, a topical antibiotic such as azithromycin or an oral antibiotic such as tetracycline should be prescribed.
INFLAMMATION
It is increasingly recognized that DED is an inflammatory disease; chronic inflammation can affect the ocular surface, the lacrimal glands, and the conjunctiva, often referred to as the lacrimal functional unit. This can lead to chronic ocular surface disease, impaired quality of vision, and a reduction in quality of life.1
For these reasons, antiinflammatory treatments have become an important part of DED management. Cyclosporine ophthalmic emulsion 0.05% (Restasis; Allergan) is an antiinflammatory treatment frequently prescribed by US physicians for patients with dry eye. The situation in France, and all across Europe, is different from that in the United States, however. Here, cyclosporine cannot be obtained at drug stores but rather is solely dispensed by hospital pharmacists. This presents a barrier to widespread use of the drug, which has enjoyed much greater acceptance in the United States than in Europe.
Topical corticosteroids present another useful approach to antiinflammatory treatment for DED. Although their prolonged use is associated with ocular complications including elevated IOP and cataractogenesis, in serious cases of DED with decrease in visual acuity a relatively short but intensive course of topical steroids can help to get inflammation under control. This can then be followed by a switch to a longer-term prescription of cyclosporine.
Dietary supplementation with omega-3 fatty acids has been shown to have antiinflammatory effects and to increase tear production in dry eye. A recent meta-analysis of randomized clinical trials found that omega-3 fatty acid supplementation was associated with better TBUT and Schirmer test results, as compared with placebo.2 However, again, in Europe, the uptake of this mode of therapy is limited because there is no social health reimbursement for the use of these supplements. Therefore, price is a key factor in access to and use of health care options. Probably fewer than 5% to 10% of DED patients are prescribed care with omega-3 supplementation, even though physicians may believe that it can be useful.
SEVERE CASES
Patients with severe DED present a special challenge. Patients can experience pain and photophobia, restricting their level of engagement with the world. Therefore, physicians who treat DED often employ extreme methods in an attempt to help these severely affected patients.
Cyclosporine can be used as a long-term treatment in patients with severe DED. I have more than 60 patients under my care taking cyclosporine on a long-term basis. However, as mentioned above, this is always under the control of a hospital physician in an attempt to influence expenditures under national health insurance. This situation may change in coming months because a new brand of cyclosporine, Ikervis 1% (Santen), is expected to become available in September. If this proves to be a less expensive option, it may change the approach to prescription of this useful medication.
In a few severe cases, use of autologous serum may be indicated, for instance, in patients who are not responsive to cyclosporine or cannot tolerate treatment with cyclosporine, or in patients with extensive corneal involvement with SPK and visual acuity decrease. However, obtaining autologous serum can be challenging in France.
Punctal plugs can also be helpful in patients with decreased tear production, such as in DED associated with systemic Sjögren syndrome. They can also be helpful in patients with DED after refractive surgery, although their efficacy seems to decrease dramatically with time.
Finally, scleral lenses can be helpful in patients with severe DED. These contact lenses rest not on the cornea but on the sclera and can retain a saline solution against the cornea all day long. This can provide some measure of relief for severely affected patients.
CONCLUSION
Treatment choices for DED are many, and their selection depends on the particular situation of the patient, including the nature of the DED and its severity. This article presents only a brief overview of available treatment options for patients with DED. It is hoped that this can serve as a reminder of some of the clinical factors that should be considered in selecting therapeutic options for patients with DED. n
1. Calonge M, Enríquez-de-Salamanca A, Diebold Y, et al. Dry eye disease as an inflammatory disorder. Ocul Immunol Inflamm. 2010;18(4):244-253.
2. Liu A, Ji J. Omega-3 essential fatty acids therapy for dry eye syndrome: a meta-analysis of randomized controlled studies. Med Sci Monit. 2014;20:1583-1589.
Jose L. Güell, MD, PhD
• Director, Cornea and Refractive Surgery Unit, Instituto de Microcirugía Ocular, Barcelona, Spain
• Associate Professor of Ophthalmology, Universitat Autonoma de Barcelona, Spain
• guell@imo.es
• Financial disclosure: None
Leonardo Mastropasqua, MD
• Director of the Ophthalmology Clinic, Center of Excellence in Ophthalmology, National High Technology Eye Center, University G. D’Annunzio of Chieti and Pescara, Italy
• mastro@unich.it
• Financial disclosure: None
Mario Nubile, MD
• Supervisor of the Cornea and Ocular Surface Unit of the Ophthalmology Clinic, Center of Excellence in Ophthalmology, National High Technology Eye Center, University G. D’Annunzio of Chieti and Pescara, Italy
• m.nubile@unich.it
• Financial disclosure: None
Pierre-Jean Pisella, MD, PhD
• Professor of Ophthalmology, University Hospital, Departments of Ophthalmology and Pharmaceutical Sciences
• Université Francois-Rabelais, Tours, France
• pierre-jean.pisella@univ-tours.fr
• Financial disclosure: Consultant (Alcon, Allergan, Abbott Medical Optics, Santen, Thea)



